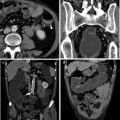
Fig. 12.1
Drainage of a wide abscess of the whole right perineal region and silicone loose seton positioning in two fistula tracks
The two main aspects to be considered at the very beginning for their therapeutic and prognostic implications are the anatomical definition of the fistulous track(s) with associated complications, and the level of inflammation of the colon and rectum. For initial diagnosis of perianal fistulising UC, contrast-enhanced MRI should be considered the procedure of choice; Endoscopic Ultrasound (EUS) has similar sensitivity, but inferior specificity than MRI, and it cannot be performed in the presence of stenosis and painful abscesses; Transperineal Ultrasound (TPUS) should be used in the presence of anal stenosis or abscesses, and both US methods can be improved with hydrogen peroxide enhancement; Computed Tomography (CT) is preferred in emergency settings. Fistulography is no more recommended. All these methods achieve the best results when combined with Examination Under Anaesthetics (EUA). EUA is reported to have an accuracy of 90 % in the hands of an experienced colorectal surgeon, but most important, it permits contemporary identification of all fistulae tracts, loose seton positioning and abscess drainage (Figs. 12.1 and 12.2) [14].


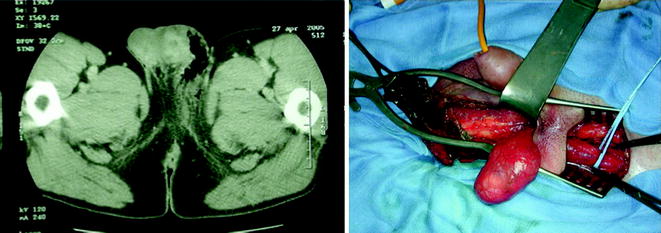
Fig. 12.2
EUA and loose seton positioning for stabilization of a perianal fistula. Left, identification of the track using a probe. Right, silicone loose seton in position
In CD patients, the incidence of perianal disease is 20–25 % in association with terminal ileitis, and it rises as high as 60 % for colonic location and 92 % when the rectum is actively involved. However, in UC patients the rectum is involved by definition, and thus a colonoscopy has to be performed in order to characterize the activity and the extension of the disease [14, 15].
Once a diagnosis of PD is established, there is no consensus for classifying the fistulae. The Parks’ classification should be used for the description of fistulae courses due to its implication in surgical management, but in clinical practice most experts prefer the classification into simple or complex [14, 16]. Simple perianal fistula should be considered a fistula with a straight course connecting the internal and external orifices. Complex perianal fistulae are those with one or more of the following characteristics: multiple internal and/or external orifices; presence of ramifications with external orifices, with genitalia or blind sinuses in the perineal tissues; concomitant abscess, both as a mass or a circular collection between the muscles (horseshoe abscess); upper rectum, pre-sacral, obturatory abscesses or phlegmons; single or concomitant ano-vaginal and recto-vaginal tracts; concomitant severe rectal inflammation. Furthermore, a pelvic floor dysfunction should be addressed and, in case of severe pelvic muscles impairment, a specific rehabilitation programme should be adopted (pelvic floor dysfunction is responsible for several perianal problems in the general population, so it should be excluded as an additional risk factor for PD diagnosis and treatment).
Simple perianal fistulae should be treated only if symptomatic. In case of treatment, loose seton placement and/or antibiotics (metronidazole and ciprofloxacin) should be indicated.
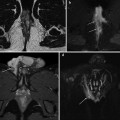
Complex fistulae should always be treated with abscess drainage and loose seton placement. The time of seton removal depends on subsequent medical therapy. In case of active luminal disease, a concomitant pharmacological treatment is indicated. Antibiotics (metronidazole and ciprofloxacin) in association with immunomodulators (azathioprine, 6-mercaptopurine, tacrolimus, etc.) or biological (infliximab or adalimumab) are the treatment of choice. Uncontrolled perianal sepsis in UC patients under steroids and/or immunosuppressant treatment could lead to Fournier’s gangrene, a rapidly progressive, life-threatening condition that requires emergency surgery (Fig. 12.3) [17].