Fig. 15.1
A plain CT showing a giant frontal hydatid cyst in a 4-year-old Kazakh boy (a) and an intubated patient and a large skin incision marked in supine position with the head turned a little toward the opposite side of the lesion (b)
Positioning
Craniotomy
The craniotomy should be planned to be larger than craniotomies utilized in usual space-occupying lesions, and the excess should be planed toward the inferior edge of the cyst (Fig. 15.2). It is preferable to use clamps rather than Raney scalp clips to secure hemostasis of the scalp. The sharp edges of the Raney scalp clips may injure the falling cyst. It is preferable to use a manual burr hole handle and a Gigli saw than an electric or air-powered drill because the vibrations of the later may rupture a cyst in its proximity. The bone flap is then carefully lifted and separated from the underlying dura matter and removed as a free flap (Fig. 15.3a). One must be sure not to leave sharp bony edges in the field. These should be carefully trimmed and smoothened to prevent and inadvertent rupture of the cyst (Haddad and Haddad 2003).
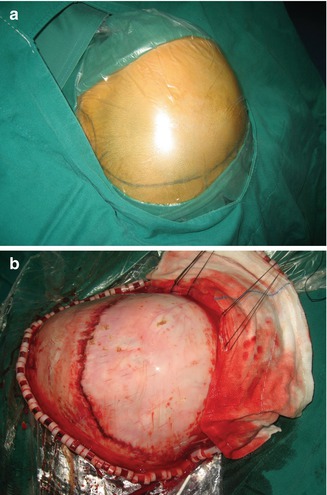
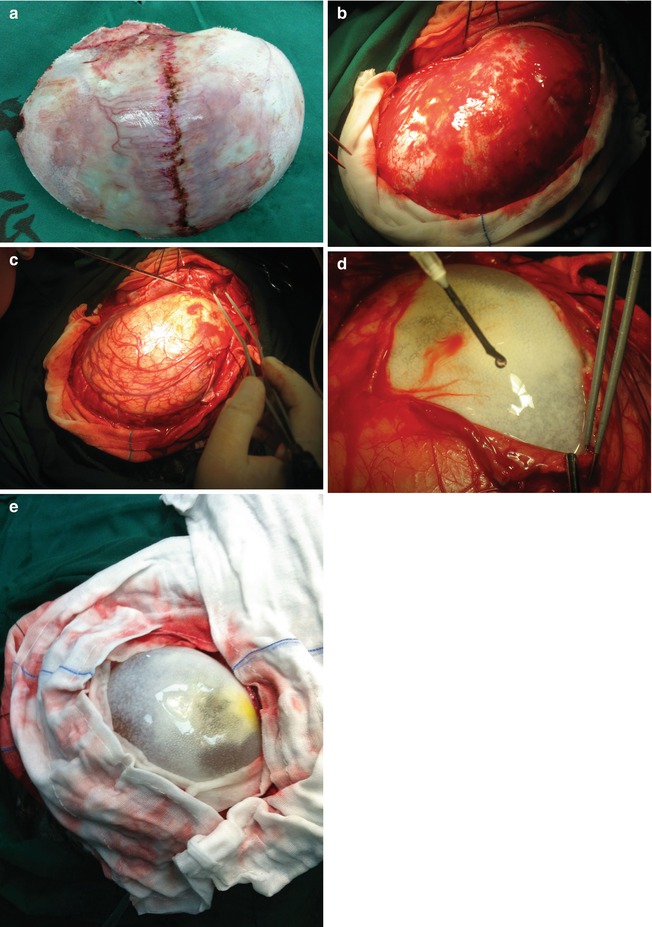
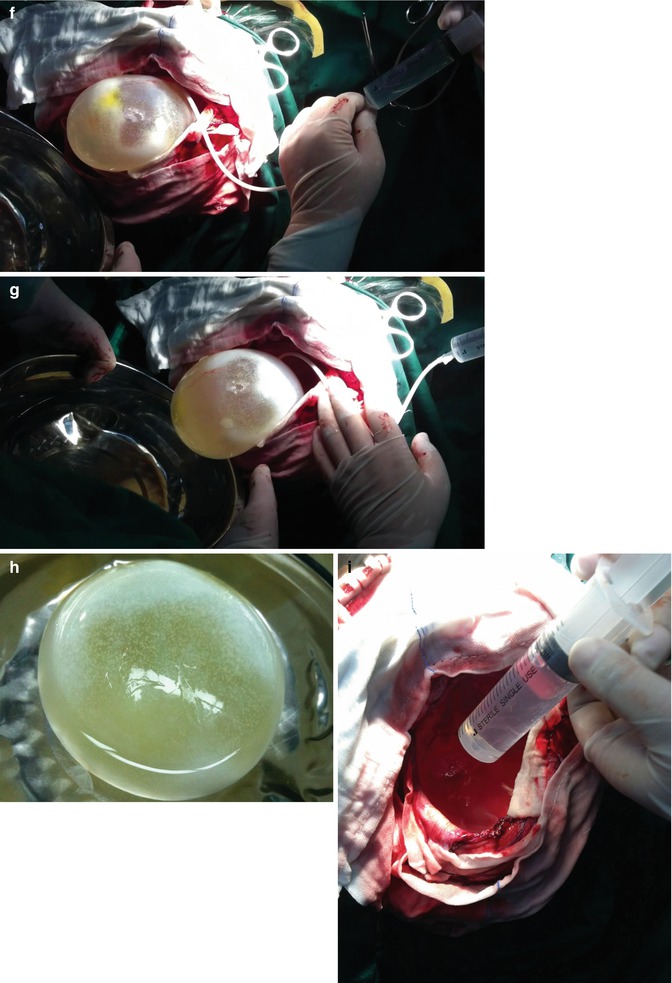
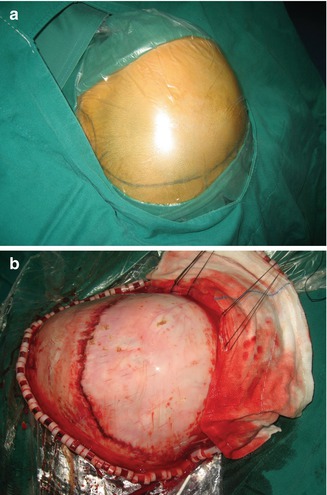
Fig. 15.2
A plain CT showing the operating filed sterilized and draped (a) and a large skin flap reflected (b)
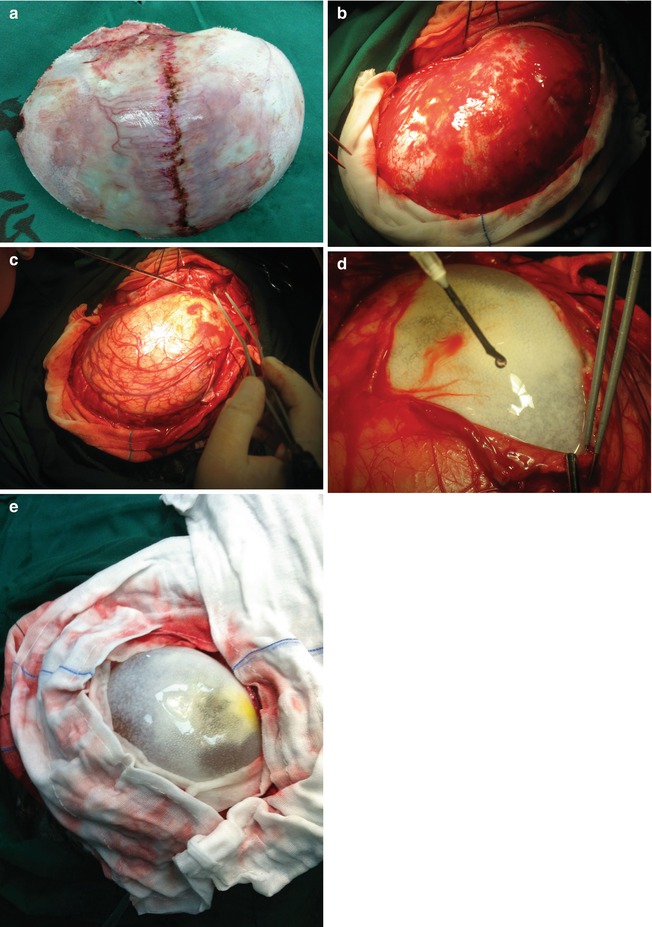
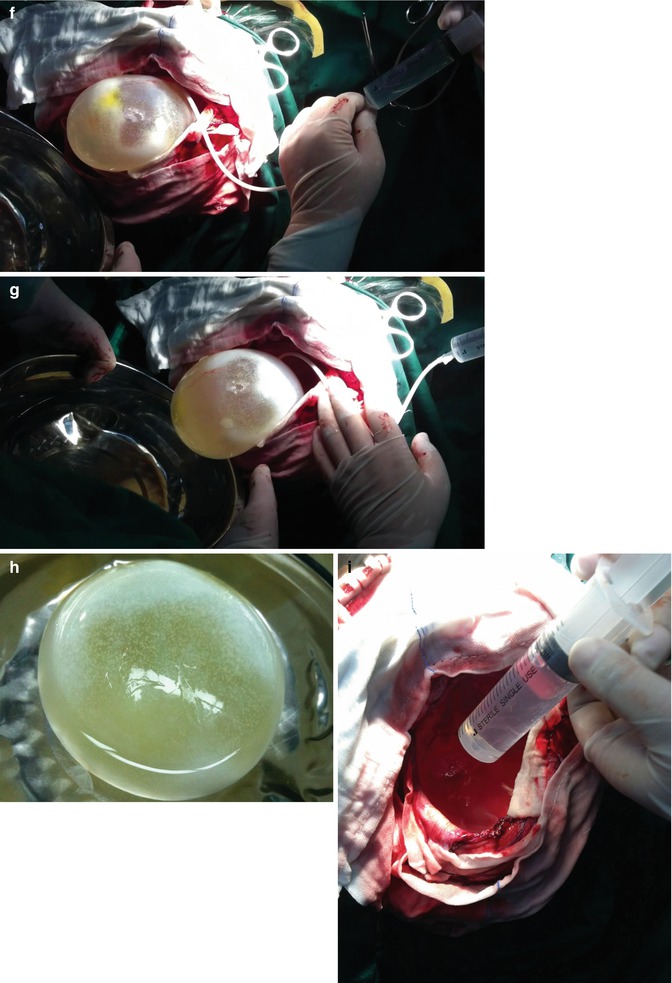
Fig. 15.3
A plain CT showing a large free bone flap removed (a), a tense dura (b), a thin layer of cortical tissue overlying the hydatid cyst (c), a meticulous cortical dissection performed to expose the cystic wall (d), the entire cystic wall exposed (e), the operating table tilted toward the lesion side and the head of the patients lowered and a fine plastic tube inserted between the cystic wall and brain tissue (f), floating of hydatid cyst after injecting saline with the syringe (g), intactly removed hydatid cyst in a bowel with water (h), and the irrigation procedure after the removal of the hydatid cyst (i)
The dura is carefully opened starting away from the expected position of the cyst, and any adhesions to the underlying brain or ectocyst should be released carefully (Fig. 15.3b). Tucking of the dura is strongly recommended after the opening of the dura, not before, to prevent possible injury of superficially lying cysts. On illumination, through the thinned dura, cyst fluid may be observed in some patients once the cranium has been opened (Fig. 15.3c). Usually there is a very thin cortical tissue, if any, under the dura mater (Fig. 15.3c).
Operative Field Draping
This is of paramount importance. It may prevent cyst rupture, and in case of such inadvertent rupture, this draping will minimize the damage. Fine gauze imbibed with 0.1 % Cetrimide is placed around the bone edges of the craniotomy, as well as over the normal brain tissue. The same type of gauze covers all clamps and/or Raney scalp clips and fishhooks if in use. Rolls of wet gauze are tucked between the edges of the dura and the cortex to prevent the seepage of fluid into the base of the brain, in case of rupture.
The Delivery
Usually a small surface of the cyst appears through the cortex. This area is not large enough to permit the safe delivery of the cyst. The arachnoid is carefully opened. As seen in Fig. 15.3d, “episiotomies” are performed in silent areas. While carrying these episiotomies, no cautery, uni- or bipolar, should be used. Any significant blood vessel should be clipped and not coagulated. These vascular clips could be removed at the end of surgery and the blood vessels coagulated then. The episiotomies are carried though the depth of the cortex until the cyst wall is seen (Fig. 15.3e). At this stage the “membranes” should be ruptured to allow a normal delivery. The membrane in these cases is the pericyst. In the brain, there is a very fine pericyst which at times may rupture spontaneously. If it remains intact, it will hamper delivery. One can tear it with a blunt instrument. Once the apparent portion of the pericyst is resected, the head of the patient is readjusted in a way to have the cyst in the most dependent position (Fig. 15.3f). A band of soft gauze, soaked in cetrimide, is laid on the cortex from the interphase between the cyst and cortex, in its most dependent position and extending to the receptacle which will receive the specimen. This receptacle should contain some cetrimide to prevent the direct fall of the cyst against the container’s solid bottom. A fine pliable rubber tube is inserted in the space between the pericyst and ectocyst, and a 0.1 % Cetrimide solution is gently injected to break the adhesive effect between the peri- and ectocyst and to float the cyst (Fig. 15.3g). At this moment Credé’s maneuver by pressing on the cortex superior to the cyst and asking the anesthesiologist to compress both jugular veins in the neck in an effort to increase the intracranial pressure and gradually expulsing the cyst. In case the cyst does not come out, the head is further lowered until the cyst flows out of its cavity in the brain into the prepared receptacle (Fig. 15.3h). It is extremely important to maintain a blunt wide brain retractor in the upper portion of the cavity to prevent the brain from collapsing, which may tear crossing the veins, and to simultaneously fill the cavity with cetrimide while the cyst is being delivered (Fig. 15.3i). Once the cyst is delivered, hemostasis is completed and all the gauze is retrieved. The closure of the craniotomy is then performed in the usual manner (Turgut 2001; Haddad and Haddad 2003; Izci et al. 2008; Duishanbai et al. 2011).
Delivery of Deep Lesions
In case the cyst does not present on the surface of the cortex, the latter should be cut with a fine blunted tip pair of scissors in a silent area overlying the cyst. The opening is enlarged and deepened, with blunt dissection, until the pericyst appears. This procedure, which was called by one of the authors a “cesarean section,” should be performed with extreme care lest the cyst rupture. We have used the cortical ultrasound to detect the remaining distance between the cyst and our instrument. In case the cyst is large, its delivery is similar to the cortical cyst. However, more frequently, one is dealing with small cyst, and we found that an appropriate size kitchen spoon is very helpful in raising the cyst into the receptacle.
Puncture-Aspiration-Injection-Reaspiration (PAIR) Technique
This technique should only be used in case the previously described delivery technique is impossible to use. This, as its name indicates, involves the puncture of the cyst with a fine needle and aspirating its content and partially and carefully injecting a scolicidal solution which should be left in place for a minimum of 10 min. Then the remaining fluid is reaspirated, and the collapsed chitinous membrane is removed with a forceps. The problem in this procedure is that there is always spillage around the needle puncture, and if the cyst is rapidly and completely emptied, it collapses and cannot be refilled properly. Although the area of spillage is irrigated with a scolicidal solution to prevent anaphylactic complications and recurrences, each puncture invariably leads to some spillage of the contents into the operative field, and cyst recurrences are frequent. For example, total removal of a pontine hydatid cyst is practically impossible with Dowling’s technique, which requires forcing saline beneath the cyst in order to displace it outward.
The PAIR technique was introduced in the mid-1980s for treating liver hydatid cyst (Filice and Brunetti 1997). It is usually used for cerebral hydatid cyst in deep location or eloquent areas where removal of the hydatid cyst without rupturing is impossible or may cause additional neurological deficit (Muthusubramanian et al. 2009). Non-intentional burr hole draining was reported, but it is a very risky procedure (Anvari et al. 2009). The PAIR technique should always be performed by skilled and experienced physicians well prepared to deal with complications. According to expert recommendations, the PAIR should be accompanied by chemotherapeutic coverage to minimize the potential risk of secondary echinococcosis. In this indication, albendazole is given in daily oral doses of 10 mg/kg of body weight 24–4 h before and 15–30 days after the intervention (World Health Organization Informal Working Group of Echinococcosis 2001). There are several case reports which speak of a successful outcome in removing pontine, basal ganglion and in the interpeduncular cistern hydatid cysts (Boudawara et al. 1999; Erşahin et al. 1995; Yilmazlar and Aksoy 1999; Beskonakli et al. 2005).
Microsurgery
Hemispheric hydatid cysts usually do not need a surgical microscope, but hydatid cysts in deep locations, eloquent areas, and around vital structures need good illumination and magnification for fine dissections on the approach to the cyst or around the cyst wall. We recommend that microsurgery be applied in deep-seated lesions. The use of the magnification during the early part of the surgery of a hydatid cyst is extremely helpful because, at a crucial stage of the procedure, it prevents inadvertent damage to the very thin cyst wall and allows development of the critical surgical plane (Kurtsoy et al. 1999; Balak et al. 2006). Gamma knife treatment has been tested in only a limited number of cases (Schnider 1999).
Postoperative Care
It is recommended that the patients should stay in a neurosurgical intensive care unit overnight until the anesthesia wears off. Antiepileptic drugs may be administered and patients’ activities restricted to limit fluctuations in intracranial pressure during the early postoperative period. Albendazole is administered at a dose of 10 mg/kg for 3 months in case of cyst rupture (Duishanbai et al. 2010




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree