Fig. 14.1
Posteriorly located intradural extramedullary hydatid cyst can be seen on sagittal T1-weighted MRI. The cyst was compressing the spinal cord from the posterior aspect at the T7–8 level

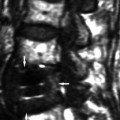
Fig. 14.2
Intradural extramedullary hydatid cyst on T2-weighted sagittal MRI. There was cord oedema
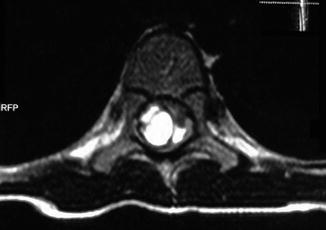
Fig. 14.3
T2-weighted axial MRI shows intradural extramedullary multilocular hydatid cyst. Right-sided lesion was compressing the spinal cord transversely
The most common symptoms and signs in vertebral involvement are paraparesis (62 %), increasing back or radicular pain (55 %), sensory loss (36 %), sphincter disturbance (30 %) and paraplegia (26 %). The time period between the onset of the symptoms and medical consultation varies between 6 and 15 months (Thaler et al. 2010).
A full discussion of the clinical findings of spinal hydatidosis is given in Chap. 8.
Pathology
Portovertebral shunts play an important role in most of the genesis of spinal lesions in hydatid cysts. The vertebral body is generally the first target. When echinococcal larvae are carried to a vertebral body, the parasite grows multilocularly along the bony intratrabecular space and infiltrates and destroys the bone like a tumour, because of a lack of defensive reaction of the bony tissue (Işlekel et al. 1998). Pathological fractures occur due to compression or avascular necrosis of the cortical bone. Subsequently the disease usually spreads to the pedicles, laminae or the ribs. The intervertebral discs are spared in the early stages of the disease. Finally the infestation may extend beyond the vertebral body and periosteum with the development of a cyst with space-occupying symptomatology. It was observed that hydrophilic degeneration of the Echinococcus embryo without reactive osteitis could develop over a number of years, with damage and erosion of the trabecular composition of the bone by the expanding vesicles, with subsequent cystic progression and invasion of all vertebral structures (Tsitouridis and Dimitriadis 1997). When the cyst perforates the cortex, it extends to the paravertebral structures and into the spinal canal or neural foramina (Kalkan et al. 2008). Bone destruction and puslike fluid may be encountered during operation, leading to the name ‘ossifluent abscess’ (Pamir et al. 2002). Papanikolaou (2008) described three mechanisms for the intraosseous invasion as mechanical, ischaemic and cellular process. The mechanical process affects the surrounding tissues by expansion, compression, dislocation and repression which cause bone and nerve tissue atrophy and osteitis. The ischaemic process affects the nutrient vessels by obstruction and compression which cause bone necrosis and sequestra formation. The cellular process affects the bone tissue by osteoclast proliferation and causes destruction.
The pathology of spinal hydatidosis has been discussed in detail in Chap. 9.
Surgical Treatment of Spinal Hydatidosis
Surgery is currently the mainstay treatment modality for spinal hydatidosis. The first surgical intervention in spinal hydatidosis was reported in 1819 by (Reydellet 1819; Rayport et al. 1964). Most of the cases admitted to surgeons with spinal cord compression syndrome symptomatology are urgent surgeries (Pamir et al. 2002). Patients with spinal hydatid disease usually present with a long history of back pain or other non-specific symptoms of spinal cord compression. Weakness of the limbs occurs in the later stages. Paraplegia or radicular compression is said to occur in 25–84 % of patients (Baysefer et al. 1996). Preoperative diagnosis and the real extent of the disease are very important for operative planning. Preoperative diagnosis of the lesion guides the surgical preference. The correct diagnosis, natural history and serological and radiological studies are essential (Kalkan et al. 2008). Generally, routine laboratory tests do not show specific values. Eosinophilia is mostly limited (15 %) or absent. An intradermal Casoni test result is positive in 95 %, but there are up to 40 % false-positive results. Indirect haemagglutination test and enzyme-linked immunosorbent assay are established methods for the detection of anti-Echinococcus antibodies (immunoglobulin G). Serological tests are 80–100 % sensitive and 88–96 % specific for liver hydatid disease. They have 50–56 % sensitivity for lung disease and only 25–56 % for other organs like spinal cyst hydatid (El-On et al. 2003; Thaler et al. 2010).
Successful treatment of the spinal hydatidosis is challenging because of its invasiveness and its potentially severe complications. Surgical excision is the first and most effective option. The total eradication of the cyst without rupture should be the primary goal of the surgery (Thaler et al. 2010). In clinical practice, however, this is not possible in the spine because there is no one cyst but a multitude of small cysts. Either anterior or posterior approaches can be preferred for the surgical treatment. Pure intradurally or epidurally located lesions at all spinal levels are approached posteriorly. In these cases surgical excision without intraoperative rupture results in cure (Pamir et al. 2002). Bone involvement is very important for defining the recurrence rates. Surgical planning should be made according to this.
Spinal disease most frequently involves the thoracic segments (46–50 %). Lumbar segments (20–29 %) and sacral segments (20–23 %) are also involved frequently. Cervical spine is the least common affected segment (Pamir et al. 2002). Twenty-eight reports of spinal hydatid disease, published during the past five decades, from Turkey, were reviewed, and 71 patients with spinal hydatid disease were collected (Turgut 1997). According to this study, spinal echinococcus involved the thoracic segment of the spine in 35 patients (49 %), the lumbar segment in 28 patients (39 %), the cervical segment in three patients (4 %), the thoracolumbar segment in three patients (4 %) and the sacral segment in one patient (2 %) (Turgut 1997). One patient had non-contagious lesions in the cervical and lumbar segments (Turgut 1997).
Surgical Treatment of Cervical Spinal Hydatidosis
Hydatid disease in the vertebral column is rare in cervical spine. Several procedures can be useful for the spinal hydatid cyst in the cervical region. Cervical laminectomy is the favourite approach for spinal hydatidosis affecting the cervical aspect of the spinal canal. Intradural lesions are also approached posteriorly. The posterior approach to the cervical spine is relatively straightforward and is well known by all neurosurgeons. Avoidance of risk to the anterior vascular and visceral structures is an advantage of this approach. Potentially greater discomfort and longer hospital stays and increased incidence of spinal deformity are the major disadvantages of this surgery. Postlaminectomy kyphosis is common if the laminectomy is performed in an immature spine. Resection of 50 % or more of one facet or its capsule results in a significant risk of subsequent instability (Tandon and Vollmer 2006). The use of lateral mass plating is a significant improvement for the treatment of cervical spine instability. Keller et al. (1997) reported a case of postoperative kyphosis after an anterior corpectomy with simple bony fusion in a spinal hydatid patient. Progressive myelopathy occurred, in this reported patient, and it was successfully treated with a posterior lateral mass plating.
The anterior approach may be utilised for decompression and stabilisation of the cervical spine in a variety of conditions. Anterior approaches including corpectomy with simple bony fusion and corpectomy with anterior plating have been reported for the treatment of cervical spinal hydatidosis (Keller et al. 1997). Anterior instrumentation, in addition to bone grafting, has been generally successful in the cervical spine when treating infection and may obviate the need for posterior instrumentation.
Surgical Treatment of Thoracic Spinal Hydatidosis
Spinal hydatidosis most commonly affects thoracic spinal segment (Figs. 14.4, 14.5, and 14.6). The reported approaches in thoracic cases were mainly posterior. The posterior approach via laminectomy is the main choice of treatment (Pamir et al. 2002). Complete surgical removal and most extensive removal of the infected bone must be the goal of the surgery. Decompression of the cord, resection of the cysts, infected bone resection and deformity correction can be done in one approach under direct vision of the cord through a posterior approach (Figs. 14.7 and 14.8). Extradural multiple cysts and cysts located in the bone or in the paravertebral region are the most commonly seen scenario (Figs. 14.9 and 14.10). Daughter cysts may form within the main cyst (Işlekel et al. 1998). Surgical excision without intraoperative cyst rupture results in a cure in pure intradural or pure epidural lesions. In most cases the cysts are multiple and extensive. It is nearly impossible to remove these cysts without rupture. During laminectomy, cysts are almost always ruptured (Işlekel et al. 1998). More extensive lesions with vertebral body involvement can be also approached posteriorly via a transpedicular route (Pamir et al. 2002).
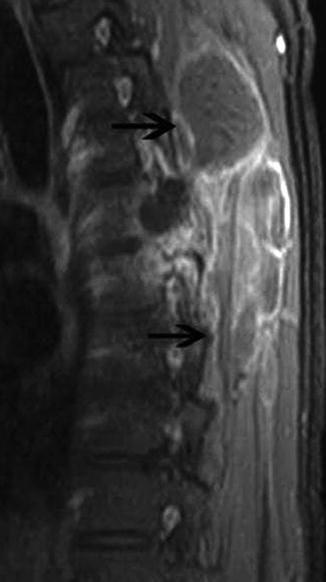

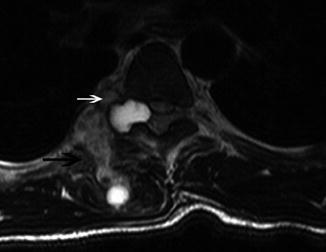
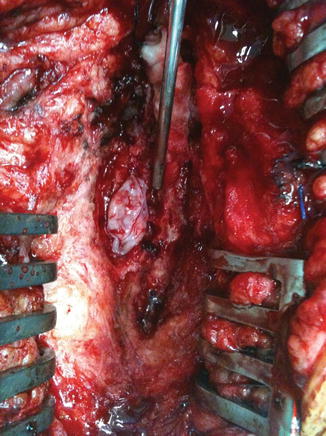

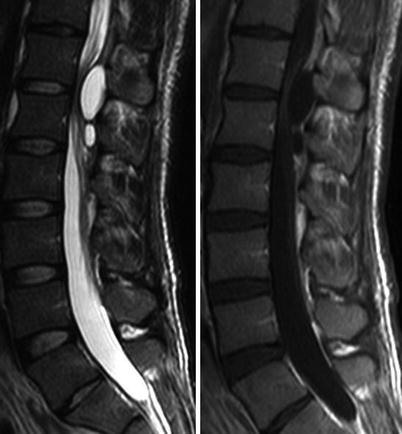
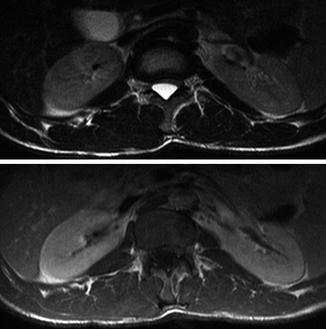
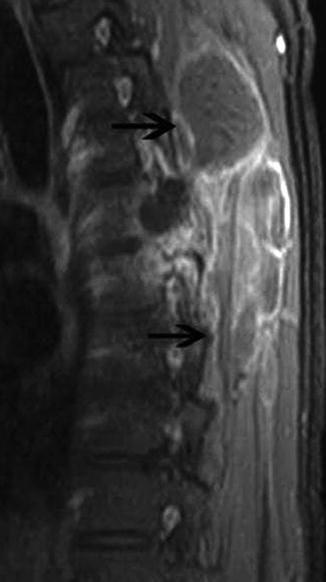
Fig. 14.4
T1-weighted sagittal MRI obtained after contrast administration shows multiloculated cystic lesion at the T4 level. Black arrows indicate rim enhancement of the cystic lesion

Fig. 14.5
T1-weighted sagittal fat-saturated MRI obtained after administration of intravenous contrast material reveals rim-enhancing loculated cystic lesions through posterior epidural space (black arrows)
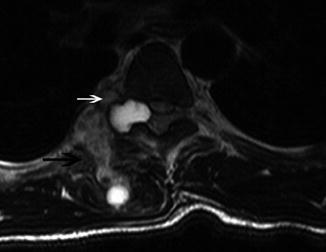
Fig. 14.6
T2-weighted axial MRI reveals heterogeneously hyperintense multiloculated cyst infiltrating paravertebral muscles (black arrow) as well as epidural space through neural foramen (white arrow)
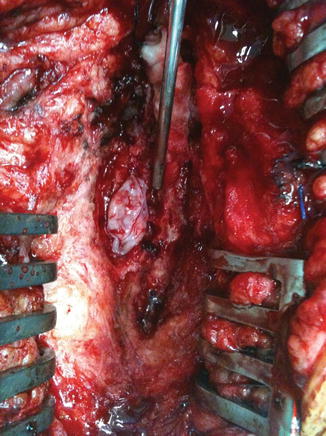
Fig. 14.7
Intraoperative view of a posterior laminectomy site. Extradurally located hydatid cyst can be seen

Fig. 14.8
Some of the cysts which were retrieved during surgery
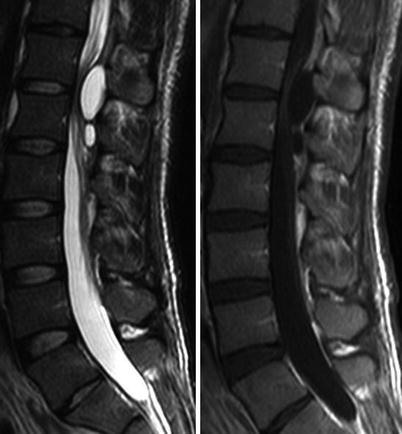
Fig. 14.9
T2- and T1-weighted sagittal contrast-enhanced MRI shows multiloculated hydatid cyst with rim enhancement. The lesion was located in posterior epidural space at the level of T12–L1
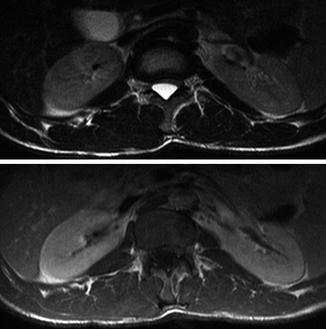
Fig. 14.10
T2- and T1-weighted axial MRI shows cystic lesion which was compressing the dural sac anteriorly
Simple decompression with laminectomy is performed most frequently due to its low morbidity and mortality, but it is not free from risks. Access to the vertebral body through a laminectomy is limited, resulting in poor outcomes, especially in recurrent disease. Despite treatment, the disease frequently relapses with progressive destruction of the vertebral column and neurological deterioration (Senoglu et al. 2009). Kaoutzanis et al. (1989) suggested that routine laminectomy for spinal hydatid did not significantly affect the outcome. Turtas et al. (1980) reported a 50 % recurrence rate after posterior decompression alone. Thaler et al. (2010) indicated that partial hydatid cyst resection, inappropriate stabilisation and posterior multilevel laminectomies without posterior stabilisation have led to progressive deformities of the thoracic spine. They concluded that no cases of reoperations due to spinal deformity were found when cyst resection and posterior laminectomy were combined with anterior or posterior stabilisation.
Khazim et al. (2003) reported seven cases of spinal hydatid disease treated with posterior decompression and were followed up for an average of 20 years. They concluded that the long-term results were very poor, with high rates of mortality, localised and extra-vertebral recurrence, significant neurological deficits, spino-cutaneous fistulae, spinal instability and pain. Spinal column deformity often occurs in children after multilevel laminectomies for spinal tumours, and its incidence, in these patients, has been reported to be 24–100 % (Papagelopoulos et al. 1997).
Herrera et al. (2005) presented a large series which consisted of 20 spinal hydatid cases. In this series seven thoracic region cases were reported: they exposed the spine posteriorly in all except two patients, and they recommended posterior decompression alone only in cases with isolated neural arch and in extraosseous extradural presentations (Herrera et al. 2005). For the lesions situated in the vertebral body, they recommended an anterior approach to remove the infested bone (Herrera et al. 2005). They also recommended a posterior approach to remove the involved posterior elements and to add a posterior fixation (Herrera et al. 2005). Technically, they used Harrington or Luque spinal instrumentation and pedicle screws for posterior fixation (Herrera et al. 2005).
Khazim (2006) suggested that if stabilisation with pedicle screws is performed, the disease might be iatrogenically seeded into the vertebral body if viable scolices are present at the surgical site. Fusion or stabilisation is not recommended if only partial or complete laminectomy without excessive facet joint excision is performed (Khazim 2006). In our clinical practice we decide to add instrumented fusion depending on whether instability is already present or is created by surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree