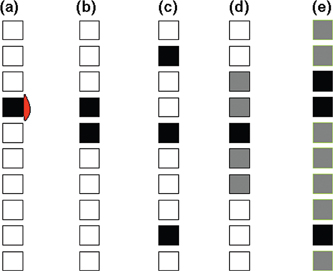
8 Radiosurgery is defined as the delivery of a large, highly conformal dose of radiation to a localized area using a stereotactic approach. One of the defining characteristics of radiosurgery is the rapid fall-off of the radiation dose distribution outside the target volume, allowing for the delivery of a large dose to the target while avoiding the adjacent normal tissue. It is for this reason that radiosurgery requires precise targeting of the target volume. In this context, the accurate delineation of the target tumor is the first and perhaps most critical step in the clinical application of radiosurgery. The process of target tissue delineation should be based on the physical and biological characteristics of radiosurgery, requiring a detailed knowledge and understanding of the particular tumor growth patterns and imaging. In addition, there is both voluntary and physiologic motion of extracranial target sites. Most physiologic motion is secondary to inspiration and expiration. Although there also may be minor organ movements that are related to arterial pulsation or transient elevated intracranial pressure, the spinal cord and vertebrae move relatively little with respiration when a patient is in a supine position. Because physiologic movement of the spine is negligible, including this variable of uncertainty in the determination of the margin for the planning target volume is generally not performed. Nevertheless, the accuracy of patient immobilization and treatment must be carefully considered in the design and planning of each target volume. The proper use of imaging technology is important in delineating the target volume. Image fusion of computed tomography (CT) and magnetic resonance imaging (MRI) is frequently employed in spine radiosurgery. Commercial fusion algorithms are available, using the image stretching method to compensate for different spine curvatures. A preferred method is an image fusion of the involved spine without image modification, although the curvature of the entire spinal column may not match precisely. The MRI must be fused with the planning CT, with the region of interest at the center of both studies. In some cases of bone-only disease involvement, the planning CT images may provide better target delineation than MR images. Avoiding the extra step of obtaining an MRI for fusion planning certainly decreases the overall cost of the treatment and eliminates another test for the patient. Most patients have already undergone diagnostic MRI prior to radiosurgery treatment that provides sufficient anatomical information for contouring purposes. Functional imaging studies such as 18-fluorodeoxyglucose (FDG)—positron emission tomography (PET) to assist in target delineation for spine tumors are currently being explored. Conventional treatment for spine metastases has included the use of palliative radiotherapy, which usually involves one or two rostral and caudal vertebral bodies in addition to the involved vertebrae, employing various fractionation schedules, most commonly 30 Gy in 10 fractions.1 When there is an epidural tumor extension that causes rapid neurological deterioration, open surgical decompression has been favored.2,3 Recently, more aggressive first-line direct decompressive surgery followed by radiotherapy led to a superior outcome over conventional fractionated radiotherapy alone in patients with symptomatic spinal cord compression from metastatic cancer.4 The results of this study emphasize the important role of achieving local tumor control in spine metastases patients with epidural compression of neural structures. In a similar fashion, the goal of spine radiosurgery is to improve local tumor control by delivering a high biological dose of radiation to the delineated target. Because many patients with spine metastases have functional problems related to the spine involvement, in addition to complex medical and oncologic issues, the treatment should be well tailored to the individual patient’s medical and psychosocial needs, with an emphasis on the patient’s functional outcome. Indeed, there are many long-term survivors with spine metastases. A recent meta-analysis of spinal metastases reported an overall 1-year survival rate of 40 to 50%.5 An analysis of radiosurgery for solitary spine metastases also showed a similar survival rate, with varying median survival time according to different tumor histology. The median survival time of patients with breast and prostate primaries and multiple myeloma far exceeds 12 months.6 This fact supports the use of aggressive local treatment to maintain long-term tumor control, as has been demonstrated to be the case for radiosurgery for brain metastases.7 The primary goal of spine radiosurgery is to maximize local tumor control of the involved spine while palliating symptoms. Therefore, the intent of radiosurgery is to treat the entire visible gross tumor in the spine. The treatment algorithm pathway of radiosurgery for spine metastases at the Henry Ford Hospital (Detroit, Michigan) is illustrated in Fig. 8.1. Radiosurgery is most frequently used to treat solitary spine metastasis (Fig. 8.1a). Any soft tissue extension of the tumor causing epidural compression or a paraspinal mass is included in the target volume. Likewise, two contiguous spine levels can be treated with radiosurgery (Fig. 8.1b). In addition, radiosurgery may be used to treat separate lesions that are not adjacent to one another (Fig. 8.1c). When there is diffuse spine involvement with one or two levels of more clinical significance either by symptoms or by epidural compression (Fig. 8.1d), radiosurgery can be used as a boost to those specific vertebral bodies concurrent with conventional external beam radiotherapy. Target delineation in these cases should be the same as for other solitary metastases. In cases of more diffuse metastatic spine involvement, conventional external beam radiotherapy or radionuclide therapy is indicated instead of radiosurgery (Fig. 8.1e). With increased experience, we have found that patients with diffuse spine metastases can also be treated successfully with single-fraction radiosurgery, thus avoiding protracted fractionated radiotherapy, if the symptomatic area is identifiable both radiographically and clinically. In patients who experience a rapid neurological deterioration resulting from direct compression of the spinal cord or cauda equina by either epidural tumor or retropulsed bone, open surgical decompression is indicated. Radiosurgery has been employed successfully in these postoperative cases with a similar type of target delineation as for solitary metastases.8 In a similar manner to postoperative cases, radiosurgery may be used by combining the overall management of the lesion with pretreatment minimally invasive procedures such as vertebroplasty and kyphoplasty.9 Figure 8.1 The decision protocol of radiosurgery for spine metastases. (a) A solitary spine metastasis is treated with radiosurgery. Any soft tissue extension of the tumor causing epidural compression or a paraspinal mass is included in the target volume. (b) Two contiguous spine levels may be treated with radiosurgery. (c) Noncontiguous lesions are treated with radiosurgery. (d) Diffuse spine involvement with one or two levels of more clinical significance either by symptoms or by epidural compression, radiosurgery can be used as a boost to conventional radiotherapy. (e) In widespread diffuse spine involvement, radiosurgery can be used for epidural compression or clinical significance in conjunction with conventional radiotherapy. Several target volumes must be considered in the spine radiosurgery treatment plan. The gross tumor volume (GTV) represents all tumor that is visible on imaging studies. The clinical target volume (CTV) is the volume likely to contain microscopic disease. Because of the rapid dose fall-off inherent to radiosurgery, if the CTV is not included in the target delineation, the patient may have a less than satisfactory clinical and radiographic response. In spine radiosurgery, the planning target volume (PTV) often equals the CTV with no margin accounting for setup error and target motion. There are many factors that influence the process of making decisions on the radiosurgery target volume, including tumor factors, normal tissue constraints, and host factors. These factors are summarized in Table 8.1. In delineating the radiosurgery target volume, there are generally two different types of practices currently employed. The first practice is to include the entire vertebral body and soft tissue component within the target volume, more consistent with the classic teaching of non-imaged-guided conventional external beam irradiation. The other practice is to include only the GTV that is visible on either CT or MRI and not the entire bone. There is currently no consensus on the use of one contouring practice over the other. There are limited data as to whether one method is superior in terms of local tumor control, symptomatic response, or recurrence. At both the Henry Ford Hospital and the University of Pittsburgh Medical Center (Pittsburgh, Pennsylvania) spine radiosurgery programs, it is the current practice to delineate the target volume to include the entire involved vertebral body and both pedicles of the affected vertebrae. When there is paraspinal or epidural extension of the tumor, the involved vertebra or vertebrae and the gross tumor are included in the target volume as well. The reason to employ this method is based on the understanding that the metastatic process likely will involve the medullary bone within the involved vertebral body. Tumor cells within the bone marrow have been found in > 30% of patients with even early breast cancer.10 This would imply that the presence of micrometastasis may be even greater in the bone marrow when the spine is invaded by the gross tumor. The microstructure of the bone marrow renders it particularly vulnerable to tumor cell accumulation and bone invasion. Multiple capillaries near the endosteal bone margin become contiguous with a rich venous sinusoidal system with a capacity 6 to 8 times that of the osseous arterial system. It is thought that metastases to bone are mostly hematogenous, yet the skeletal blood flow represents only 4 to 10% of cardiac output. The high incidence of spread within bone tissue is attributed to this microstructure of bone.11 By including the clinically involved spine within the target volume for radiosurgery, the failure outside the target volume (i.e., at the immediately adjacent spinal level) was < 5% in one clinical series.12
Target Delineation and Dose Prescription
 Target Delineation
Target Delineation
Radiosurgery Treatment Decision Algorithm
Vertebral Metastasis with or without Epidural or Paraspinal Extension
| Tumor factors |
| Tumor histology |
| Extent and number of spine levels involved |
| Shape of the tumor |
| Systemic disease status |
| Normal tissue constraints |
| Spinal cord |
| Kidney |
| Bowel |
| Esophagus |
| Lung |
| Host factors |
| Prior irradiation to the target |
| Concurrent systemic therapy |
| Comorbidity |
| Performance status |
| Estimated survival time |
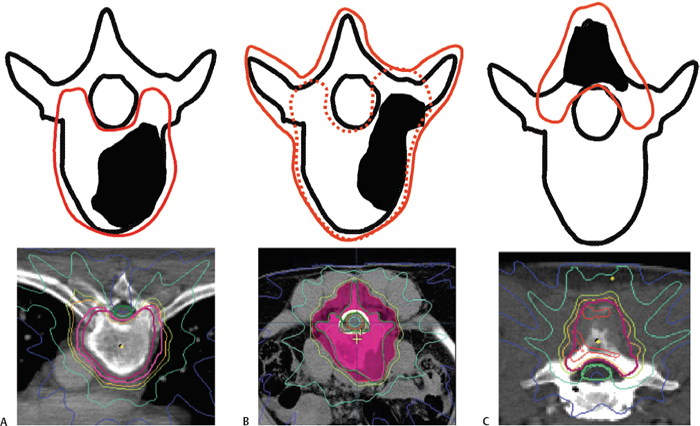
Figure 8.2 The target volume definition of radiosurgery for spine metastases. (A) Involvement of the body of the vertebra is the most common type of spine metastasis. The entire vertebral body and both pedicles are included in the radiosurgery plan. (B) Vertebral body involvement can be treated either to the entire vertebra (vertebral body and dorsal elements) or in the same fashion as in A and C but with a generous margin (dotted line). (C) For involvement of dorsal elements, the target volume is the dorsal elements only (spinous process and lamina), including both pedicles, while sparing the vertebral body.
This method of target delineation is illustrated in Fig. 8.2. There can be several different scenarios of spine involvement. Involvement of the actual body of the vertebra is the most common type of spine metastasis (Fig. 8.2A). In this case, the entire involved vertebral body and both pedicles are included in the radiosurgery plan, as shown. Figure 8.2C demonstrates an example of the treatment of the dorsal elements (spinous process and lamina), including both pedicles, while sparing the vertebral body. Vertebral body involvement, such as that shown in Fig. 8.2B, can be treated either to the entire bony element (vertebral body and dorsal elements) or in the same fashion as in Fig. 8.2A and C, but with a generous margin.
In rare cases, radiosurgery targeting of the GTV only is used when the spinal cord is significantly dose limiting or when the treatment is strictly for palliation of symptoms.
Target Delineation in the Postoperative Setting
Experience with postoperative radiosurgery for spine metastases has been published.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


