Picture archiving and communication systems (PACS) and the Internet have changed how clinicians interact with their clinical colleagues, both during the day and at night. Teleradiology may improve the quality of life for radiologists but it also improves the quality of the interpretations for the patients. Given the opportunity this provides to connect subspecialist clinicians with subspecialist radiologists, daytime and nighttime teleradiology is likely to increase. Although teleradiology may worsen the commoditization that started with PACS, patient care will likely be improved, and that should always be the highest priority.
- •
Picture archiving and communication systems and the Internet are the key enablers of teleradiology.
- •
More than half of the radiology groups in the United States are covered by a nighthawk service.
- •
Teleradiology is improving patient care by bringing subspecialist interpretations to small and rural practices.
The times they are a-changin’ —(Robert A. Zimmerman aka Bob Dylan, 1964)
Teleradiology has probably been around in one form or another since there were radiologists. In the early days of the last century, plain films taken in physicians’ offices were sometimes couriered to radiologists for expert interpretation. In the early days of magnetic resonance (MR) imaging almost 3 decades ago, I received images by FedEx and interpreted them remotely before dictating a report or calling the referring radiologist. Although these methods of dissociating the site of image acquisition from the site of interpretation could be called teleradiology, a more modern definition would involve sending digital images over the Internet. With the widespread implementation of picture archiving and communication systems (PACS) and increasing Internet bandwidth, teleradiology for nighttime coverage and daytime subspecialty reads became possible approximately 20 years ago. This article reviews the history of teleradiology with parallels to the changing times of radiology as a specialty and the recent advent of the Digital Age. It examines the bright and dark sides of teleradiology with regard to lifestyle, quality interpretations, and potential for commoditization and predatory practices.
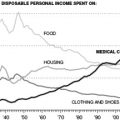
A little more than 50 years ago, radiologists were viewed as ancillary. They did not provide nighttime or weekend coverage; they just read out whatever accumulated during the off hours during the next business day. There was not much demand for them to provide after-hours readings because most clinical specialists thought they could read radiographs as well as radiologists. Most radiology groups consisted of fewer than 5 so-called utility infielders, interchangeable and generalists, who covered all the bases. Because it did not really matter who read what, they might have been considered to be a commodity. With the introduction of computed tomography (CT) and then MR imaging, most clinicians realized that they did need radiologists for the interpretation, and that they needed them 24/7. Add to this the trend toward increasing subspecialization, and the fellowship-trained radiologists were becoming part of the clinical team, and clearly not a commodity. Radiology groups were also tending to increase in size to adequately load the radiology subspecialists with work.
Radiology took a step backward with regard to commoditization with PACS. Before full PACS implementation several years ago, our clinicians used to come down to the Radiology Department to discuss their cases. It was good for us because the clinicians either provided additional history, which might lead to a better diagnosis, or confirmed a diagnosis already made, which is important feedback about our image interpretation skills. In the process, we got to know each other. Over time, if we generally provided accurate interpretations, the clinician would make allowances if we subsequently made an error. Some clinicians wanted specific, personalized radiologists to review their cases. As mutual respect was developed, we found ourselves supporting each other on potentially contentious medical staff issues.
Now that PACS has been fully implemented, we rarely see our clinicians. They can see the images and read our reports in their offices, or in the clinics or on the floors of the medical center. What a time saving in a medical world where efficiency is paramount! The only time the referring physicians now call is when they disagree with a reading. They rarely come to the Radiology Department anymore because we can each access the same image on PACS from different locations to discuss over the phone. As a result, many of the clinicians cannot put a name to the face of many of our junior faculty, fellows, and residents (and vice versa). The camaraderie of the old days is gone and we are being increasingly commoditized. Furthermore, with increasing priority being placed on productivity, many radiologists do not even want to see or talk to the clinicians because it just slows them down with non-relative value unit (RVU)-producing work. So although I do not disagree that teleradiology may contribute to commoditization, I think the real culprits are PACS and a culture that is becoming increasingly RVU-driven because of the decreasing reimbursement for radiology examinations and the desire to maintain income. When the only activity that provides bonuses is image interpretation productivity, and not friendly consults or attendance at tumor boards, radiologists adapt, and not necessarily in a good way.
This article discusses nighttime coverage and daytime subspecialty readings separately because they evolved independently.
Nighttime coverage
Nighttime coverage has gone through 5 stages: (1) wake up and drive to the hospital, (2) wake up and read from home, (3) stay up at night and cover the emergency department (ED) internally, (4) outsource nighttime coverage to another US-based group working at night, and (5) outsource nighttime US coverage to another group working from offshore where it is daytime. Each of these stages is discussed from my personal experience.
Stage 1: Wake up and Drive into the Hospital
When I started practicing radiology in 1981, I had to drive my Toyota Celica into the hospital to read an emergency film. Each call resulted in about 2 hours of lost sleep, but at least we were awake by the time we arrived at the hospital. If the emergency room (ER) physician was reasonable, he would not call us in, except for extreme emergencies, such as a lateral cervical spine film for a broken neck (which turned out not to be as accurate as we thought once we started doing CT). The ER physicians would interpret the films at night, render treatment based on that interpretation and we would do the official reading the next morning. If there were a discrepancy, we would contact the ER and they would contact the patient if a different treatment was needed. This process was not exactly optimal patient care nor was it optimal for radiologists because they also had to work the next day after occasionally coming into the hospital the night before.
Stage 2: Wake up and Read from Home
In the mid-1980s, the first camera-on-a-stick teleradiology systems became available. I can remember our radiology group discussing whether we really wanted to adopt this technology because it might increase the number of times we were called at night. Although ER physicians might have a high threshold for calling us physically into the hospital, they would likely have a lower threshold to ask us to look at cases from a video unit in our homes. It turned out not to seriously affect the number of cases we were asked to see at night and it had the advantage (for us) that we could view the images at our bedside and not fully wake up. Reading a study while half asleep might not be thought to be optimal patient care, but this was the standard of care for the next decade, and I still dreaded my nights on call. It was the worst part of being a radiologist.
Stage 3: Stay up at Night and Cover ED Internally
In 1993, the Office of the Inspector General realized that management of patients at night was being based on the ER physician’s interpretation of the images, not our interpretation the next morning. They decided that they would only pay for contemporaneous readings. At that time, I was part of a 60-person radiology group (Memrad Medical Group, Inc.) that covered 7 hospitals in southern California. Memrad’s president (Paul Berger, MD) realized that this ruling could potentially result in a significant loss of income to the group. If the ER physicians could read during the night, they would argue that they should be able to read during the day, which would decrease our income by 30%. Dr Berger was determined to provide contemporaneous readings, but to do it by having only 1 person stay up all night covering all 7 hospitals. This strategy was accomplished with expensive T1 lines and rudimentary teleradiology systems all feeding into 1 radiologist at the main hospital, Long Beach Memorial. Similar multihospital coverage was performed by other large private groups at about the same time.
Our system went live on January 1, 1994. The night call was initially rotated among everybody in the group. My entry in the log book on January 4, 1994 was “worse night of my life since internship.” In addition to getting several calls at once from different hospitals (where I did not work during the day), I was talking to ER physicians whom I did not know and who did not know me (commoditization). This system reduced the total number of nights we were on call and had the advantage that we were wide awake and probably rendering better contemporaneous readings than we had been doing half asleep at night from a video system at home. Because everyone in the group initially had to rotate through the system, we had neuroradiologists reading emergency body CT scans and body radiologists reading emergency brain MR images. We might have been awake but, because we were all subspecialized, we were not necessarily all skilled at reading emergency studies involving multiple organ systems.
It did not take long for the senior partners to start paying the junior partners (who were closer to residency and still utility infielders) to take their call. For those of us who were subspecialized, we argued that this was better patient care; the junior partners were also willing to work for the extra money. Market forces prevailed: after a few months the group paid the junior partners $1000 per night and gave them the next day off. Call generally occurred for a week at a time to minimize adjustments to the circadian rhythm. However, after about a year, even the junior partners burned out working 5 to 7 nights in a row, so we hired 4 radiologists whose job was to cover nights 1 week a month and cover days as internal locums 1 other week each month. They could take the other 2 weeks a month as vacation or they could work for more pay. The nighttime radiologists were dubbed “nighthawks.” By extension, the same people working during the day became known as “dayhawks.” However, there was still a premium for working at night; when I left Memrad for the University of California, San Diego (UCSD) in 2002, the nighthawks were each making 30% more than a full partner and were working 30% fewer hours.
Stage 4: Outsource Nighttime Coverage to Another US-Based Group Working at Night
When the 4 nighthawks were first hired, they dictated all the cases they saw at night. The argument was that there would be fewer films to read the next morning so we could cut the number of radiologists at a given hospital from, for example, 5 to 4, thereby covering the added cost of the nighthawks. This never happened. Those who had been used to 12 MR scans per day being a good day’s work were reluctant to read more. Thus, to help pay for the nighthawks, we began covering for other groups, in effect insourcing their night calls. By relaxing the requirement that all studies be dictated by the nighthawk, we were able to cover more outside groups with just wet readings and bring in more outside income to cover the added cost of the nighthawks. At the same time, several commercial entities arose that only provided nighttime coverage to outside groups. These companies started providing coverage in the same state, then in the same region, and eventually throughout the United States. Radiologists found that they could make the same income just performing preliminary reports at night from home as going into a hospital where they had to deal with final detailed reports, referring clinicians, and even occasionally with patients. The process of commoditization was advancing further.
Stage 5: Outsource Nighttime US Coverage to Another Group Working from Offshore (Where it is Daytime)
In September 2000, we installed PACS in the MR imaging center at Long Beach Memorial. The next month I was lecturing in Xian, China, and was asked to read a neuro-MR imaging case from Long Beach by logging into our PACS unit over the Internet. When I called the neurosurgeon back home, it was the middle of the night there and the middle of the afternoon in China. I realized that radiologists no longer needed to be up at night. As a result of PACS and the Internet, they could read from anywhere in the world where it was daytime while it was nighttime in the United States. I discussed this with Paul Berger (who had retired from Memrad in 1995) and he turned the idea into NightHawk Radiology Services (NRS). Their first reading center was in Sydney, Australia, where the NightHawks read from midafternoon to midnight; a second center was subsequently established in Zurich, Switzerland where they read from 6 am to midafternoon. By decoupling the nighttime US coverage from working at night, the extra pay premium for being up at night was obviated and compensation could be based on productivity and accuracy.
One of the advantages of reading the most difficult emergency radiology studies from around the country is that the readers quickly become skilled at emergency radiology. Because most cases are dictated by the local group when previous studies and additional history are available the next morning, this led to a built-in quality assurance program. Any discrepancies between the wet reading and the final report were noted, providing feedback to both the nighthawk and the local radiologist. In addition to becoming skilled in ER radiology, the nighthawks were wide awake because it was their daytime. Reading from virtual centers of 20 radiologists or so scattered physically across the globe but linked electronically in an e-office, interesting cases could be shown around and second opinions sought on the more difficult cases.
In the last several years with the expansion of emergency CT scans, there has been an increasing demand for final reads in the middle of the night. Because the Centers for Medicare and Medicaid Services (CMS) requires that all Medicare and Medicaid studies be read from the United States (vs offshore), the number of offshore teleradiologists has recently decreased relative to the number staying up at night in the United States. However, should CMS come to the realization that it does not matter where an American board–certified, state-licensed, hospital-credentialed radiologist is physically located, I expect the number of offshore American radiologists to again increase.
The original model for nighttime teleradiology was to provide preliminary wet reads that only involved sending the current CT. With a limited amount of data being transmitted, a stat report could be expected back within 20 to 30 minutes. With the trend to final reads, it has been pointed out that teleradiologists are at a disadvantage because they do not have access to the same resources that on-site radiologists have, namely prior imaging examinations, radiology information system (for prior reports) and hospital information system (for laboratory reports). Although this may be a problem today, the likely increase in bandwidth in the next several years should largely obviate it as a disadvantage.
It is important to stress that these are American trained and licensed physicians reading from offshore. There are plenty of excellent offshore radiologists who were not trained in the United States and do not have their American Boards who would love to read for us. Because radiology training is currently not standardized in other parts of the world and they have not taken our American Board of Radiology certification examination, it is difficult to know how competent they are. This is 1 of the reasons that American payers only pay for American trained and boarded radiologists. Such offshore American trained radiologists occasionally put their names on hundreds of reports per hour that were interpreted by radiologists who do not have their American Boards. This practice is called “ghost reading” and constitutes Medicare fraud.
Several years ago, our Dean insisted that the UCSD Radiology Department provide 24/7 attending readings to rule out pulmonary embolism and appendicitis. Realizing that they might be up half the night when they were on call, the chest and body faculty members threatened to resign en masse. The 30 or so Fellows at UCSD (all Board-certified utility infielders) eventually agreed to cover from 5 pm to 11 pm and we contracted with NightHawk (now vRad) to cover from 11 pm to 7 am . The NRS radiologists who covered us all had California medical licenses and were credentialed on our medical staff as attendings.
Although there were 120 radiologists working as independent contractors for NightHawk during this time, only a small subset of them routinely covered UCSD, So our residents are covered by almost the same group of NightHawks from night to night. Thus, the residents and ER doctors became familiar with the names on the reports or the voice on the other end of the phone. Although, superficially, this might look like commoditization, it is no more of a commodity than we currently have with PACS and (in academics) with residents and fellows coming and going.
At the time of this writing, more than half the hospitals in the United States use a nighttime service for coverage. Although this may be driven by the desire for an easy lifestyle by radiologists, it could be argued that readings are more accurate when provided by fully awake emergency radiology subspecialists. As a result, off-site teleradiology continues to increase and is spreading to daytime subspecialty readings.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree