, Bradley W. Kesser2, Max Wintermark3 and Sugoto Mukherjee4
(1)
Division of Neuroradiology, Department of Diagnostic Radiology and Nuclear Medicine, University of Maryland School of Medicine, Baltimore, MD, USA
(2)
Division of Otology and Neurotology, Department of Otolaryngology – Head and Neck Surgery, University of Virginia Health System, Charlottesville, VA, USA
(3)
Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
(4)
Division of Neuroradiology, Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
Abstract
The external auditory canal is comprised of an outer cartilaginous and an inner bony part and is covered entirely by skin. The tympanic membrane is located in an osseous groove (tympanic annulus) and forms a complex angle, roughly about 55° with the sagittal plane. The normal tympanic membrane may not be visible on CT scans. The anterosuperior portion of the tympanic membrane is comprised of the pars flaccida, and the remainder is the pars tensa. The pars flaccida is the most common site of cholesteatoma formation. The handle of the malleus is attached to the pars tensa (Fig. 8.1).
8.1 Anatomy
8.1.1 External Ear
The external auditory canal is comprised of an outer cartilaginous and an inner bony part and is covered entirely by skin. The tympanic membrane is located in an osseous groove (tympanic annulus) and forms a complex angle, roughly about 55° with the sagittal plane. The normal tympanic membrane may not be visible on CT scans. The anterosuperior portion of the tympanic membrane is comprised of the pars flaccida, and the remainder is the pars tensa. The pars flaccida is the most common site of cholesteatoma formation. The handle of the malleus is attached to the pars tensa (Fig. 8.1).
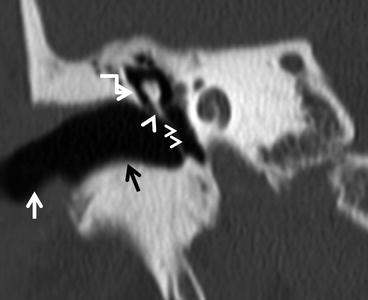
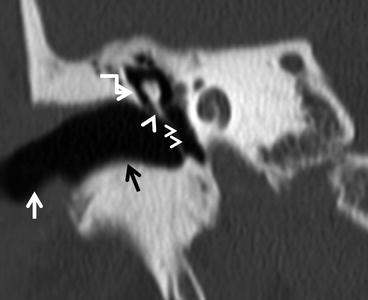
Fig. 8.1
The external auditory canal and tympanic membrane. The white arrow points to the cartilaginous EAC, the black arrow to the bony EAC. The tympanic membrane is oriented at an angle to the EAC. The large arrow indicates the pars flaccida, while the smaller arrowheads point to the pars tensa. The hooked arrow points to the scutum
8.1.2 Middle Ear
The middle ear cavity is divided into the epitympanum (attic), mesotympanum, and the hypotympanum. The mesotympanum is typically what can be seen through the tympanic membrane and is separated from the epitympanum superiorly by the facial nerve and separated from the hypotympanum inferiorly by the inferior bony annulus.
The roof of the middle ear cavity is the tegmen tympani. The floor is related to the jugular bulb. The lateral wall is formed by the tympanic membrane.
The medial wall is comprised of two eminences. The superior of these is produced by the lateral semicircular canal. The inferior eminence is due to the basal turn of the cochlea and is called the promontory. The tympanic plexus of nerves is located on the promontory. The presence of paraganglia in the plexus accounts for the occurrence of glomus tympanicum tumors in this location. Between these two eminences is the oval window niche. The tympanic segment of the facial nerve lies under the lateral semicircular canal but may pass directly over the oval window if its bony canal is dehiscent. The round window niche is located posteroinferior to the promontory at a right angle to the face of the oval window (Fig. 8.2).
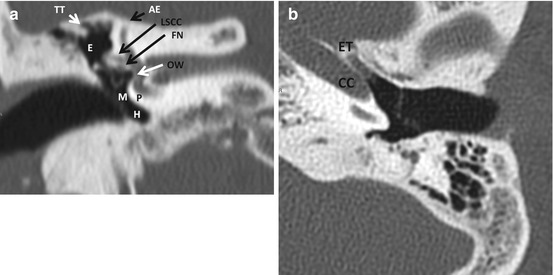
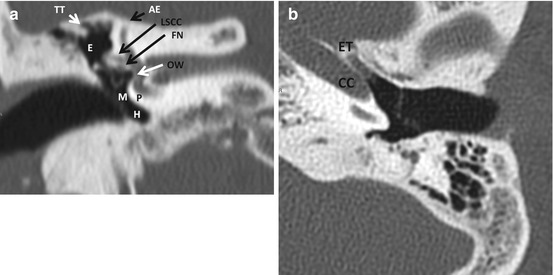
Fig. 8.2
The middle ear cavity. (a) Structures of the roof and medial wall, (b) anterior wall. Abbreviations: TT tegmen tympani, AE arcuate eminence, LSCC lateral semicircular canal, FN facial nerve (tympanic segment), OW oval window, P promontory, E epitympanum, M mesotympanum, H hypotympanum, CC carotid canal (horizontal segment), ET eustachian tube
The anterior wall in its upper portion contains two openings: one for the eustachian tube and the other for the entry of the tensor tympani. In its lower part, the anterior wall is related to the carotid canal (Fig. 8.2).
The posterior wall superiorly contains the aditus ad antrum, a passageway which leads to the mastoid antrum. Inferiorly are two recesses in which cholesteatoma may reside, the tympanic sinus medially and the facial recess laterally. These are separated by the pyramidal eminence, which contains the stapedius muscle (Fig. 8.3).
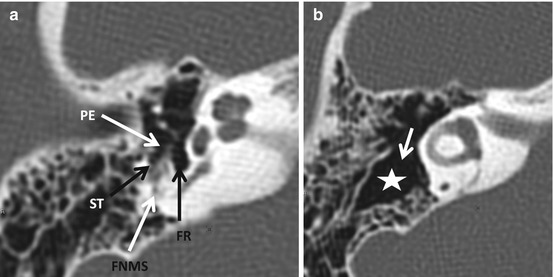
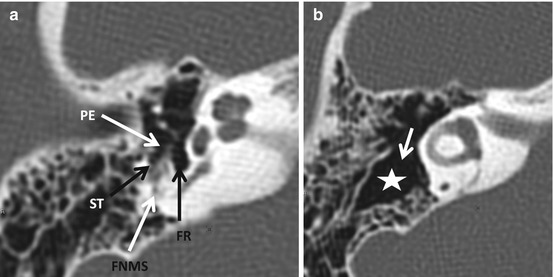
Fig. 8.3
The posterior wall of the middle ear cavity. (a) Inferior section through the mesotympanum at the level of the pyramidal eminence (PE). (b) Superior section through the epitympanum showing the aditus (arrow) and antrum (asterisk). ST sinus tympani, FR facial recess, FNMS facial nerve mastoid segment
The mastoid process can be variably pneumatized. The largest air cell is referred to as the mastoid antrum. The roof of the mastoid air cells is the tegmen mastoideum. The sigmoid sinus plate separates the mastoid air cells from the sigmoid sinus. Evaluation of the integrity of the sigmoid sinus plate is of vital importance in patients with otomastoiditis. The floor of the middle ear cavity is variably related to the jugular bulb and carotid canal (Fig. 8.4).
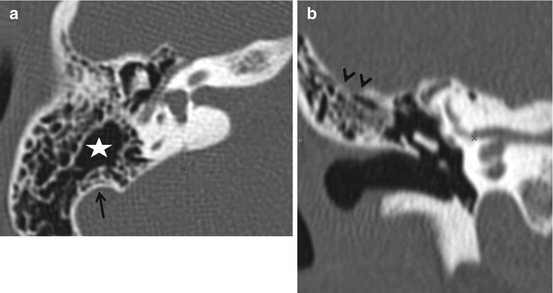
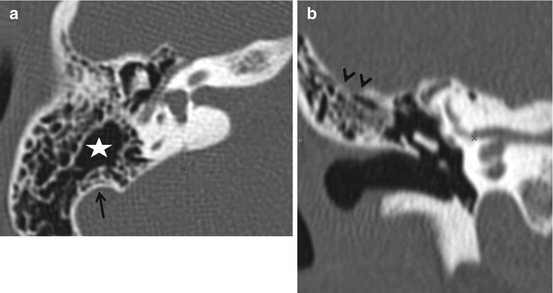
Fig. 8.4
The mastoid antrum is the largest of the mastoid air cells (asterisk). The sigmoid sinus plate is best seen on the axial view (arrow, a). The roof of the mastoid air cells is the tegmen mastoideum (arrowheads in b). The floor of the middle ear cavity is related to the jugular bulb. The bony plate separating the bulb from the middle ear cavity may be thin or absent
Prussak’s space is located in the epitympanum and is bounded laterally by the pars flaccida and a bony spur called the scutum. The medial wall is formed by the neck and head of the malleus. Its inferior wall is the lateral process of the malleus. The anterior and superior walls of Prussak’s space are formed by the lateral mallear ligament. Acquired cholesteatoma is most often found in this space (Fig. 8.5).
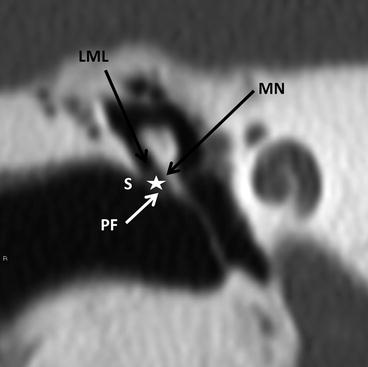
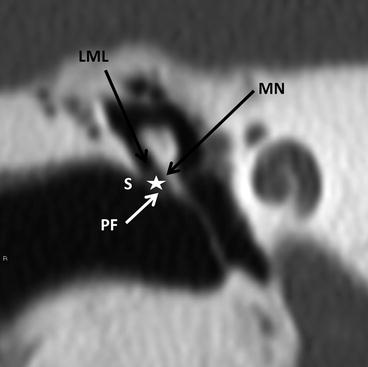
Fig. 8.5
Prussak’s space (asterisk). S scutum, PF pars flaccida, MN malleus neck, LML lateral ligament of the malleus
The middle ear cavity contains three ossicles (Fig. 8.6). The malleus is comprised of a handle (manubrium), neck, head, and a lateral process. The incus consists of a body, a posteriorly directed short process, and a long process that descends into the mesotympanum to end in the bulbous lenticular process. The lenticular process articulates with the stapes. The malleoincudal joint appears as an “ice-cream cone” on axial CT images. The head of the malleus forms the ice cream, and the body and short process of the incus form the cone. The handle of the malleus and the long process of the incus are visible as 2 almost-parallel linear structures on axial images. An oblique reconstructed image, parallel to the long axis of the incus, provides an excellent depiction of the incudostapedial joint. The stapes consists of a head, neck, 2 crura, and a footplate. The footplate articulates through a syndesmosis with the oval window.
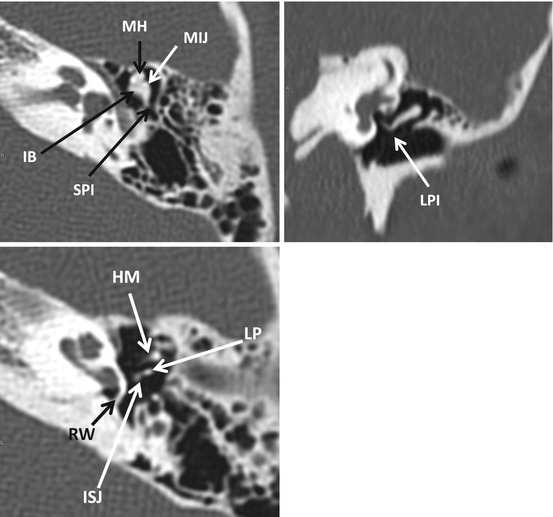
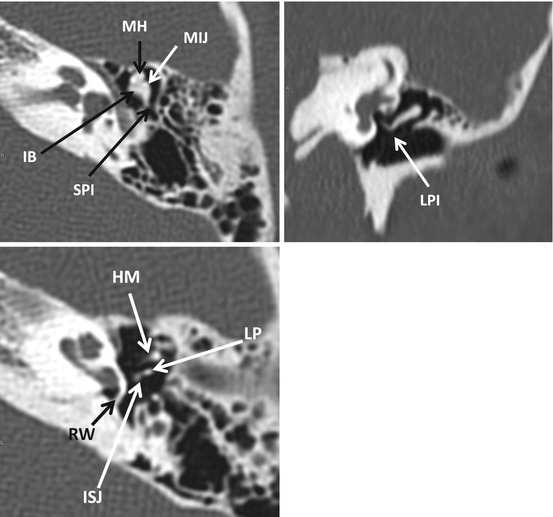
Fig. 8.6
The ossicles. MH malleus head, IB incus body, SPI short process of incus, MIJ malleoincudal joint. LPI long process of incus, LP lenticular process, ISJ incudostapedial joint, HM handle of malleus. The round window is also seen adjacent to the basal cochlear turn
8.1.3 Inner Ear
The internal auditory canal (Fig. 8.7) transmits the facial, superior vestibular, inferior vestibular, and cochlear nerves. The fundus of the IAC is divided into four quadrants, horizontally by the falciform crest and vertically in its upper half by Bill’s bar. The facial nerve occupies the anterosuperior quadrant, the cochlear nerve the anteroinferior quadrant, the superior vestibular nerve the posterosuperior quadrant, and the inferior vestibular nerve the posterior inferior quadrant. The singular canal leaves the posterior wall of the IAC and carries the branch of the inferior vestibular nerve to the posterior semicircular canal.
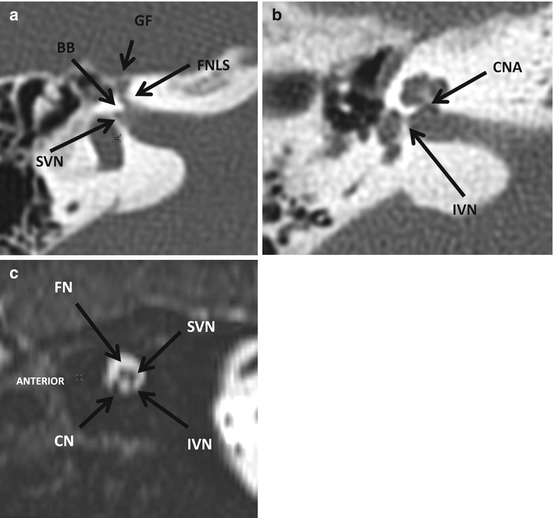
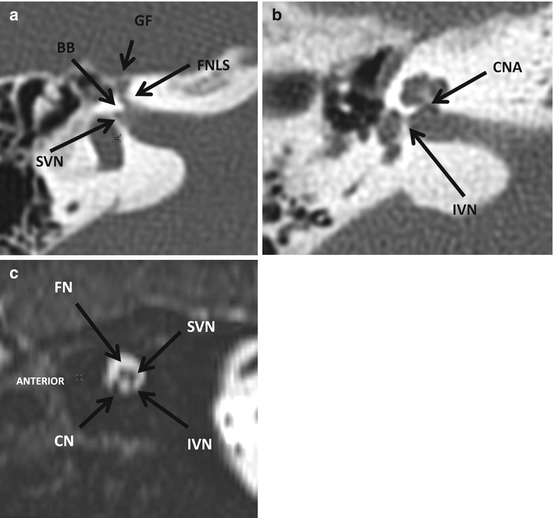
Fig. 8.7
The internal auditory canal (IAC). (a) axial section through the superior part of the IAC, (b) axial section through the superior part of the IAC, and (c) sagittal reformatted high-resolution 3D T2W image through the porus acusticus. FNLS facial nerve canal, labyrinthine segment, GF geniculate fossa, BB Bill’s bar, SVN superior vestibular nerve canal, CNA cochlear nerve aperture, IVN inferior vestibular nerve canal; FN facial nerve, CN cochlear nerve, SVN superior vestibular nerve, IVN inferior vestibular nerve
The dense bone of the osseous labyrinth encloses the delicate membranous labyrinth. The bony cochlea consists of two- and three-quarter turns and is wound around the modiolus. The interscalar septum supports the cochlear turns. At the base of the cochlea is an aperture that transmits the cochlear nerve (Fig. 8.8).
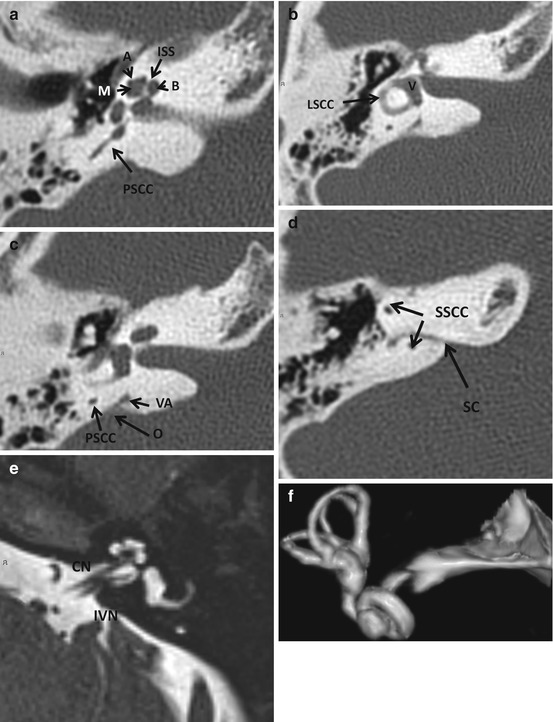
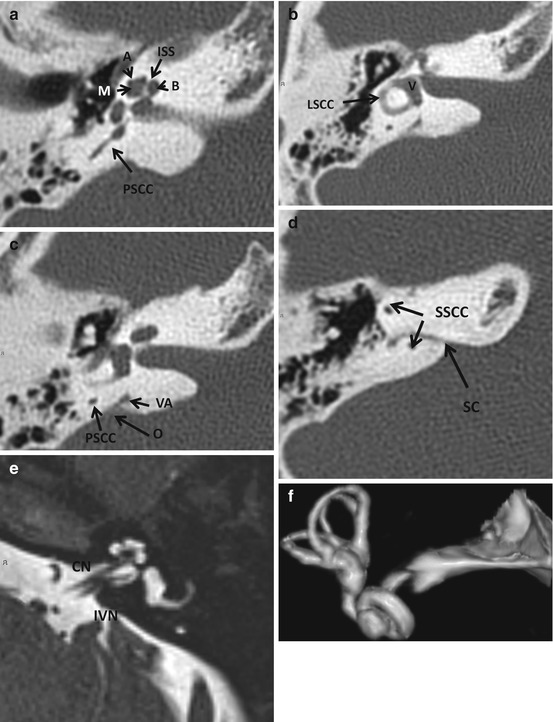
Fig. 8.8
Structures of the inner ear. In (a), the apical (A), mid (M), and basal (B) turns of the cochlea are visible. The interscalar septum (ISS) emanating from the modiolus is also seen. In (b), the vestibule (V) and lateral semicircular canal are demonstrated. In (c), the vestibular aqueduct (VA) with its flared operculum (O) is seen. The normal VA is never larger than the adjacent posterior semicircular canal (PSCC). In (d), the subarcuate canal (SC containing the subarcuate artery) is seen passing between the limbs of the superior semicircular canal. In (e), an axial high-resolution heavily T2-weighted MR image, the hypointense modiolus is seen against the background of bright endolymph within the cochlea. The interscalar septum, the cochlear nerve (CN), and inferior vestibular nerve (IVN) are also demonstrated. Volumetric images of the labyrinth (f) can be generated from both high-resolution CT and MR images
The vestibule contains the utricle and saccule. The three semicircular canals arise from it. The superior semicircular canal of one side is oriented parallel to the posterior semicircular canal of the other side. The vestibular aqueduct leaves the vestibule in a posterolateral direction. The normal vestibular aqueduct is always smaller than the adjacent posterior semicircular canal. It opens via a flared operculum into the endolymphatic sac. On high-resolution MR images, the endolymphatic sac is evident as a fluid-filled elongated structure along the posterior wall of the petrous temporal bone (Fig. 8.8).
8.1.4 Facial Nerve
The course of the facial nerve is divided into five segments: cisternal, canalicular, labyrinthine, tympanic, and mastoid. In the internal auditory canal, it occupies the anterosuperior quadrant. The labyrinthine, tympanic, and mastoid segments are enclosed in the bony Fallopian canal. The labyrinthine segment is anterolaterally directed and is relatively short. It ends in the first genu where the geniculate ganglion is located. From the anterior aspect of the geniculate ganglion, the greater superficial petrosal nerve arises. A small bony defect is usually evident at its origin. The tympanic segment is directed posteriorly from the geniculate ganglion. The segment lies under the lateral semicircular canal. If the bony canal is dehiscent, the nerve may prolapse inferiorly and lie over the oval window and stapes. This finding must always be recognized to prevent inadvertent nerve damage during surgery on the stapes. The tympanic segment ends in the second genu from which the mastoid segment continues. The segment is directed inferiorly. The nerve to the stapedius and chorda tympani arise from this segment. The facial nerve leaves the temporal bone through the stylomastoid foramen. It then passes anteriorly into the substance of the parotid gland where it is located lateral to the retromandibular vein. It then ramifies into five branches. The normal facial nerve in its cisternal and canalicular segments does not enhance on MRI. The remainder of the facial nerve may demonstrate enhancement. This is due to the presence of a perineural venous plexus (Fig. 8.9).
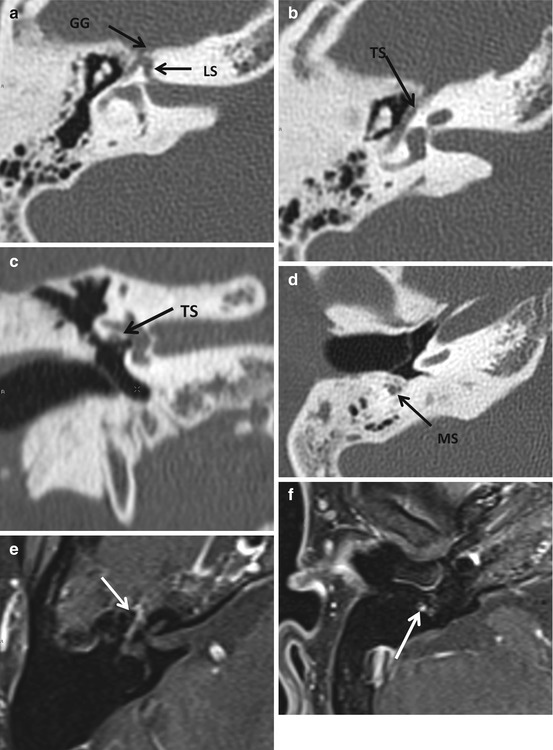
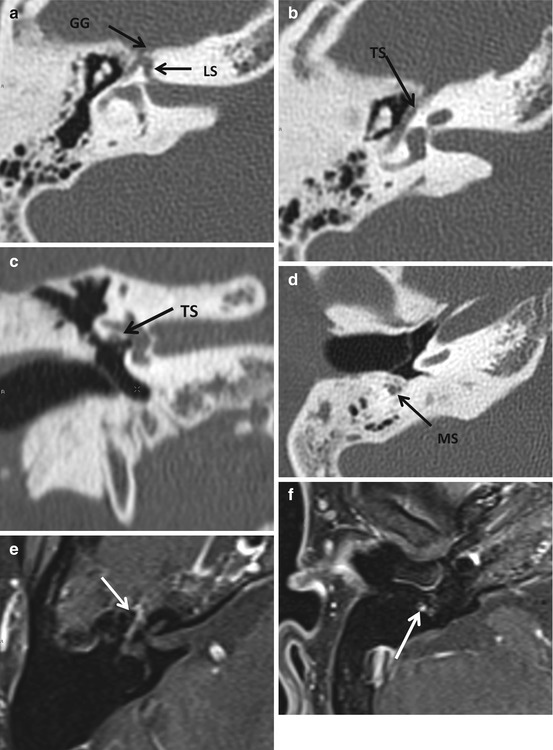
Fig. 8.9
Anatomy of the facial nerve. LS labyrinthine segment, GG geniculate ganglion, TS tympanic segment (note that the TS lies immediately under the LSCC (c) above the oval window niche. Dehiscence of this segment of the canal may cause the nerve to prolapse inferiorly and directly overlie the oval window – a finding of great surgical importance); MS mastoid segment. In (e, f), note that the geniculate ganglion, tympanic, and mastoid segments enhance – a normal finding, thought to occur due to the presence of a circumneural venous plexus. Enhancement of the labyrinthine, canalicular, and cisternal segments of the nerve is always abnormal
8.1.5 Jugular Foramen
The jugular foramen is a cleft between the petrous pyramid and the basiocciput. It is divided into an anteromedial pars nervosa and a posterolateral pars vascularis. The pars nervosa contains the inferior petrosal sinus and the glossopharyngeal nerve. The pars vascularis contains the jugular bulb and cranial nerves 10 and 11 (Fig. 8.10).
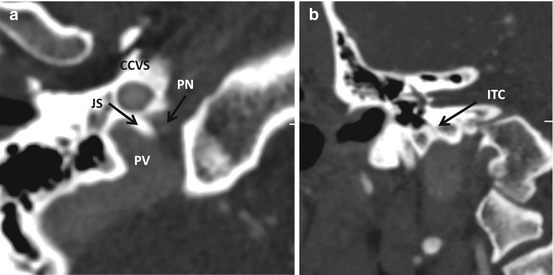
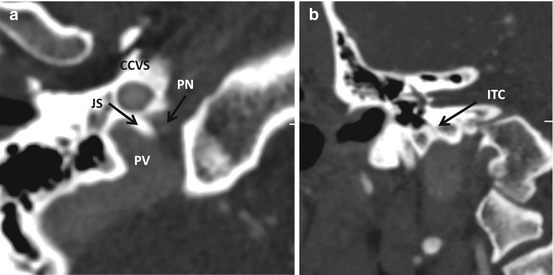
Fig. 8.10
Jugular foramen. (a) The jugular spine (JS) divides the jugular foramen into a smaller anteromedial pars nervosa (PN) which contains glossopharyngeal nerve and the inferior petrosal sinus and the larger posterolateral pars vascularis (PV) which contains the vagus nerve and its auricular branch (Arnold’s nerve), the spinal accessory nerve, the posterior meningeal branch of the ascending pharyngeal artery, and the jugular bulb. CCVS carotid canal, vertical segment. In (b), the inferior tympanic canaliculus (ITC) which contains Jacobsen’s nerve, a branch of the glossopharyngeal nerve and a small artery, is seen ascending from the bulb to the promontory, where it contributes to the tympanic plexus. Jugular paragangliomas may invade the middle ear using the ITC
8.2 Imaging Evaluation
Conductive hearing loss is best imaged by high-resolution CT with images reconstructed in a bone algorithm. Sensorineural hearing loss and vertigo are best evaluated with MRI. The MRI study should consist of pre- and postcontrast T1-weighted images (maximum slice thickness of 3 mm) obtained in axial and coronal planes, supplemented with a volumetric heavily T2-weighted sequence. The precontrast images help exclude rare cases of labyrinthine hemorrhage (which appears hyperintense on T1-weighted images) and serve as a baseline to compare the postcontrast images with. The T2-weighted sequence enables detection of small tumors in the IAC and labyrinth and depiction of vascular loops in the cerebellopontine angle cistern and IAC and is extremely useful in cases of facial or vestibulocochlear nerve hypoplasia.
Tumors of the temporal bone and skull base usually require a combination of CT and MR images. The role of catheter angiography is limited to the evaluation of pulsatile tinnitus when cross-sectional imaging has failed to reveal a cause and in the preoperative evaluation and embolization of vascular skull base tumors.
8.3 Common Congenital Anomalies of the Temporal Bone
8.3.1 External Auditory Canal (EAC) Atresia and Stenosis
Atresia or stenosis of the EAC is frequently associated with abnormalities of the malleus and incus, given that these are derivatives of the first branchial arch. Inner ear anomalies are uncommon with EAC atresia, but a large vestibular aqueduct, a dysplastic lateral semicircular canal, and varying degrees of cochlear hypoplasia may occasionally be encountered. Syndromes that may be associated with EAC atresia include the Goldenhar and Treacher Collins syndromes, Pierre Robin sequence, Klippel–Feil anomaly, and hemifacial microsomia among others.
The stenotic/atretic external ear is best evaluated on high-resolution CT. Awareness of the 10-point Jahrsdoerfer and Yeakley scale for the preoperative evaluation of aural atresia is essential for optimal interpretation of these scans (Box 8.1). Prior to consideration for surgery, the patient must demonstrate evidence of normal cochlear function on audiometric testing and a normal appearance of the inner ear on imaging. The most important determinants for a successful surgical outcome are the presence of a stapes and adequate middle ear pneumatization. As indicated in Box 8.1, the presence of a stapes is assigned 2 points. An open oval window is defined as one that is greater than 2 mm in vertical dimension on the coronal view. If it is less than 1 mm, it is considered stenotic and no point is assigned. An atretic oval window is completely separated by a complete bony plate from the middle ear. A facial nerve that demonstrates an unfavorable course, for instance, when a dehiscent tympanic segment lies over the oval window, directly in the line of surgical approach, receives no points (Fig. 8.11). The course of the facial nerve in most cases of aural atresia is predictable. The tympanic segment is foreshortened, the second genu is more anteriorly located, and the mastoid segment is often directed towards the temporomandibular joint. The presence of a relatively normal malleus–incus complex is assigned 1 point. Often the malleus and incus are fused with each other and are adherent to the atresia plate (Fig. 8.11). If there is no connection between them and the remainder of the ossicular chain, no point is assigned. The incudostapedial joint is best depicted on the coronal oblique reformations where a characteristic hockey-stick appearance is noted. A sclerotic mastoid system results in no points being assigned. The round window is in most cases normal. However, when it is less than 1 mm in width, no point is assigned. The appearance of the external ear is best judged clinically.
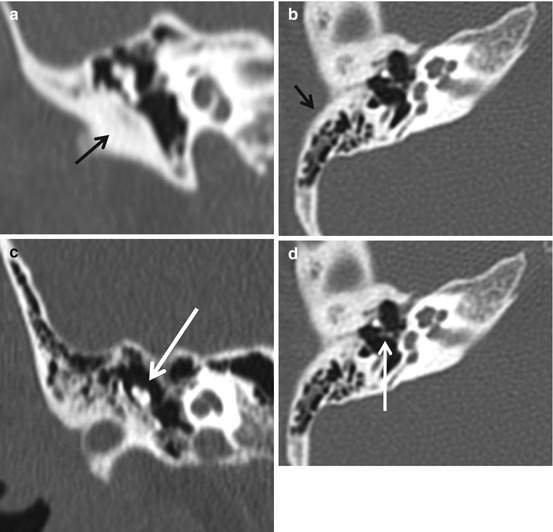
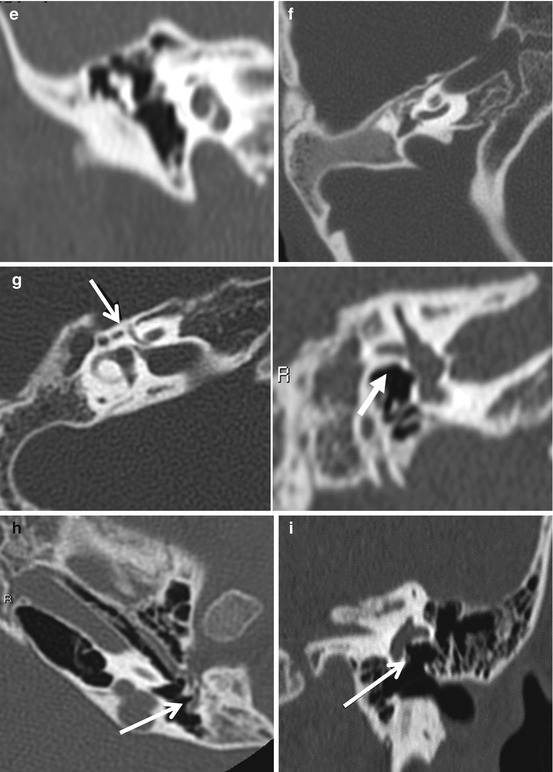
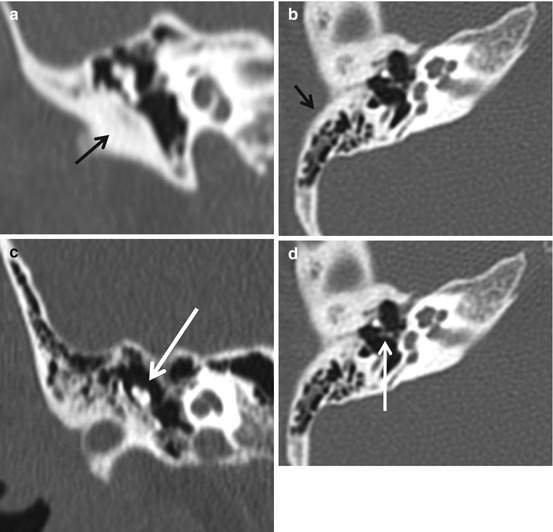
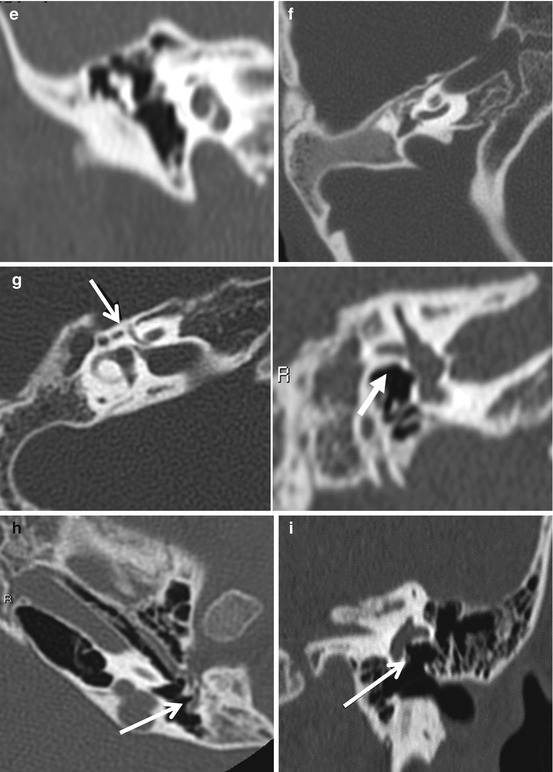
Fig. 8.11
Congenital aural atresia. In (a), a bony atresia plate is evident (arrow), whereas in (b), the atresia plate is pneumatized. In (c), a malformed malleus–incus complex fused to the atresia plate is evident – a fairly common finding in aural atresia. In (d), a normal stapes indicating good surgical prognosis is noted. In (e), note that the middle ear cleft is well aerated, a favorable surgical finding while in (f) the middle ear cleft is not pneumatized at all. This finding essentially precludes reconstructive surgery. In (g) and (h), the typical variant course of the facial nerve canal is demonstrated – a more obtuse than normal angle at the geniculate ganglion, a foreshortened tympanic segment (note that the facial nerve is not visible underneath the LSCC) and a mastoid segment displaced anteriorly to lie in proximity to the glenoid fossa. In (i), in a patient with mild atresia, the facial nerve canal is dehiscent and the nerve lies directly on the promontory. Also note that the stapes is absent. Dehiscence of the facial nerve canal is important to recognize preoperatively to prevent inadvertent nerve injury at surgery
Box 8.1. The Jahrsdoerfer Aural Atresia Scale
External ear | 1 |
Middle ear space | 1 |
Mastoid pneumatization | 1 |
Malleus–incus complex | 1 |
Incudostapedial connection | 1 |
Stapes | 2 |
Facial nerve | 1 |
Oval window open | 1 |
Round window open | 1 |
Total score | 10 |
A score of 7 or more indicates good prognosis for postoperative hearing improvement | |
8.3.2 Middle Ear Anomalies
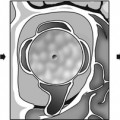
Congenital cholesteatomas are a cause of conductive hearing loss in the pediatric population. They occur usually in the anterior superior epitympanum and may be seen as whitish soft tissue behind the tympanic membrane on otoscopy. They can also occur in the external ear, mastoid air cell system, facial canal, or petrous apex. There is nothing specific about their imaging appearance, but it is important to note that they can progressively enlarge and erode adjacent osseous structures much like acquired cholesteatomas do. A well-defined middle ear mass with displacement of the ossicular chain in a child is usually a cholesteatoma (Fig. 8.12). Meningoencephaloceles may also be seen in the middle ear associated with defects of the tegmen tympani. When a nondependent soft tissue process adjacent to a bone defect and contiguous with the cranial cavity is seen on CT, a meningoencephalocele must always be suspected and evaluated with MRI.
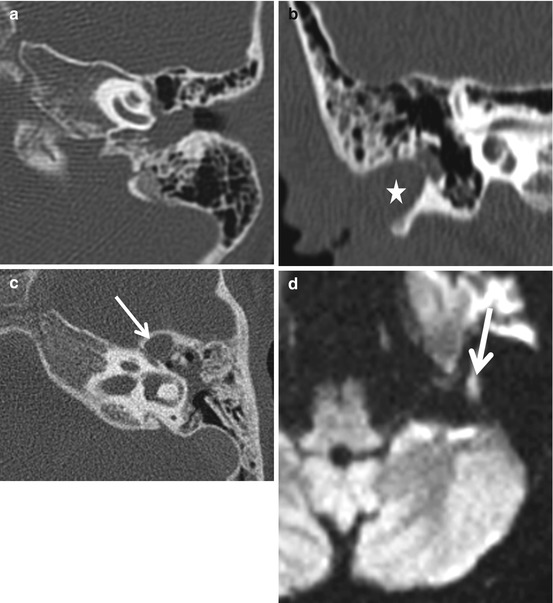
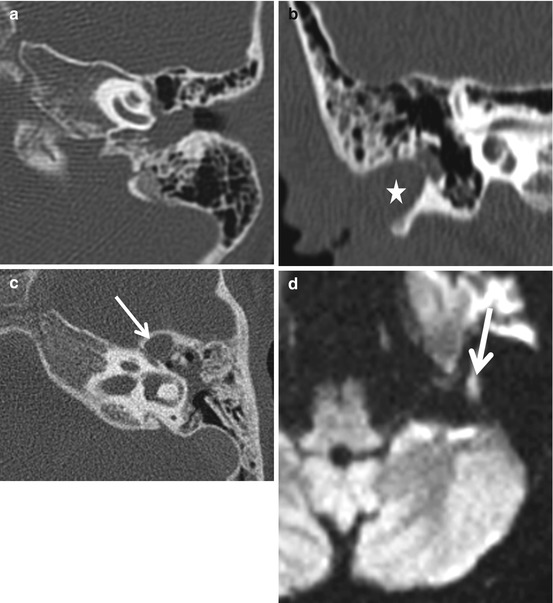
Fig. 8.12
Congenital cholesteatomas present as nonspecific middle ear masses that displace the ossicular chain (a). Stenotic EAC may also harbor a congenital cholesteatoma (asterisk, b). In (c), a soft tissue lesion is present in the anterior epitympanic recess, separated from the middle ear cavity by a thin bony septum, the cog. The diffusion-weighted MR image confirms this to be cholesteatoma
Isolated anomalies of the ossicular chain are uncommon but maybe occasionally encountered. Ossicles may be malformed, absent in their entirety or partially, or malpositioned (Fig. 8.13).
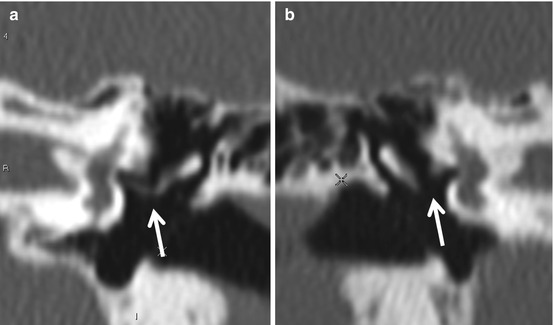
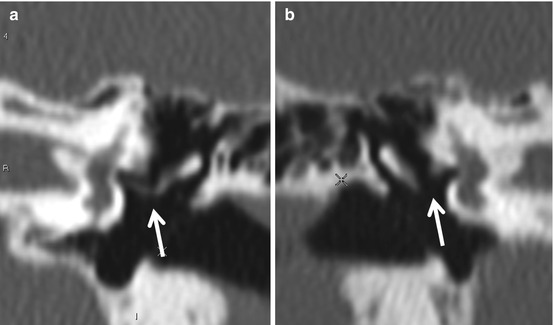
Fig. 8.13
Congenital absence of the long process of the incus. In (a), the appearance of the normal incus long process and the incudostapedial articulation (arrow) is seen. In (b), the long process and stapes are absent
8.3.3 Inner Ear Anomalies
Patients with congenital sensorineural hearing loss (SNHL) often demonstrate no imaging abnormalities. MRI is probably the better modality to image congenital SNHL. A volumetric heavily T2-weighted sequence enables excellent depiction of inner ear anatomy. On both CT and MRI, it is useful to have a checklist of what normal inner ear should look like (Box 8.2). The normal cochlea should contain three turns (apical, mid, basal), a central bony modiolus, a spiral interscalar septum and a cochlear aperture. The vestibule and the three semicircular canals must always be accounted for as one or more semicircular canals may be absent. The normal vestibular aqueduct does not exceed the width of the adjacent posterior semicircular canal in caliber.
The cochlea may be completely absent, sometimes as a part of complete labyrinthine aplasia (Michel anomaly). It may be fused with the vestibule to form a common cavity. When the apical and mid-cochlear turns are fused, the term incomplete partition type II is used. The less common incomplete partition type I anomaly is characterized by a cystic appearance of the cochlea and vestibule and a normal sized vestibular aqueduct. The incomplete partition type III anomaly is the same as the X-linked stapes gusher (see below). Incomplete partition type II is always associated with an enlarged vestibular aqueduct. This may be associated with a large vestibular aqueduct and/or large vestibule (Mondini anomaly) (Fig. 8.14).
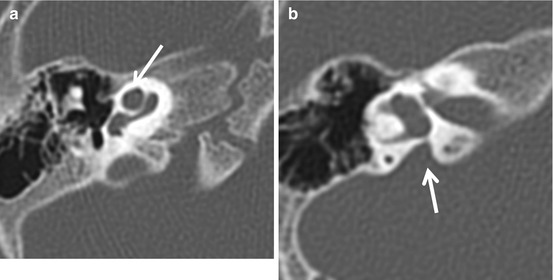
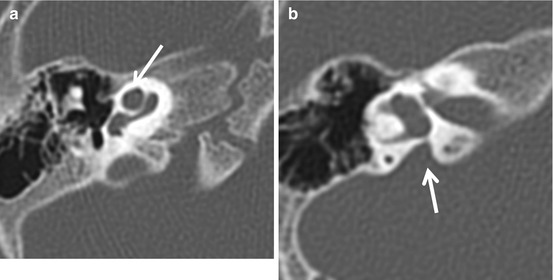
Fig. 8.14
Incomplete partition 2 (Mondini) anomaly. Note the lack of separation between the apical and mid-cochlear turns (arrow, a). In (b), enlargement of the vestibular aqueduct, a finding that frequently coexists with cochlear dysplasia, is seen (arrow)
The large vestibular aqueduct anomaly is the most common imaging finding in patients with congenital sensorineural hearing loss. CT demonstrates the enlarged vestibular aqueduct, and MR, the associated enlarged endolymphatic sac (Fig. 8.15). The onset of sensorineural hearing loss in patients with this anomaly may occur in adulthood, sometimes precipitated by trauma. The normal aqueduct is less than 2.5 mm in diameter in its midportion and does not exceed the width of the adjacent posterior semicircular canal. When an enlarged vestibular aqueduct is found, attention must be turned to the cochlea as the incomplete partition anomaly frequently coexists with his entity. The large vestibular aqueduct is a frequent finding with Pendred syndrome (congenital hypothyroidism with deafness).
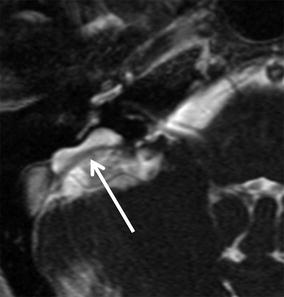
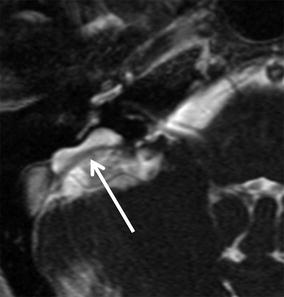
Fig. 8.15
Large endolymphatic sac anomaly. On this axial T2-weighted high-resolution MR image, the vestibular aqueduct and endolymphatic sac are dilated. The dilated (arrow) vestibular aqueduct is seen on both CT and MR, whereas the enlarged endolymphatic sac is typically seen only on MRI. This is the most common imaging finding encountered in a patient with congenital sensorineural hearing loss and is frequently associated with dysplasia of the cochlea
Absence of one or more semicircular canals may occur as an isolated anomaly. The lateral SCC is most often affected. The CHARGE association is frequently associated with semicircular canal absence (Fig. 8.16). The key head and neck imaging findings of this syndrome are summarized in Box 8.3.
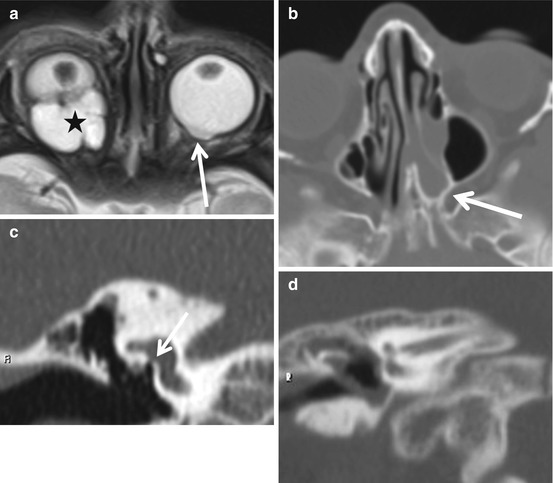
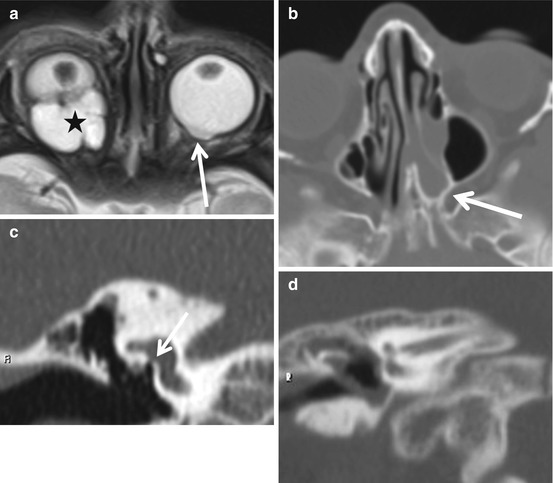
Fig 8.16
The CHARGE association. In (a), a colobomatous cyst (asterisk) and microphthalmia are seen on the right, while on the left, a small optic nerve head coloboma is seen. Bony atresia of the left nasal choana is seen in (b). In (c), the oval window is severely stenotic (arrow). Note the facial nerve lying directly in front of the oval window. Note the complete absence of the semicircular canals in (d)
When the fundus of the internal auditory canal appears bulbous, the diagnosis of X-linked stapes gusher must be considered (Fig. 8.17). This entity, which is bilateral, is associated with congenital mixed hearing loss. The conductive component arises from the associated fixation of the stapes footplate. The base of the cochlea is not separable from the fundus of the IAC. The labyrinthine segment of the facial canal is also widened. If the stapes is manipulated surgically, the increased pressure in the inner ear results in gushing of perilymph at the oval window. Patients with this entity and predominantly conductive hearing loss are therefore best treated with an external hearing aid.
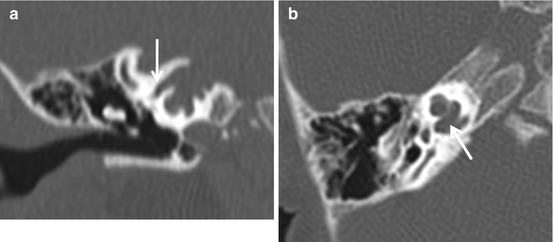
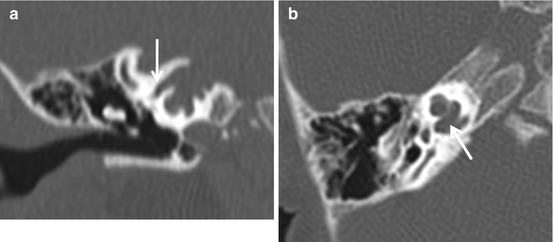
Fig. 8.17
X-linked stapes gusher. In this anomaly, the absence of a bony partition at the fundus of the IAC results in transmission of CSF pressure to the inner ear structures resulting in “gushing” of endolymph at stapedectomy. The increased pressure results in the characteristic widening of the facial nerve canal (arrow, a) and cochlear aperture (arrow, b)
Absence or hypoplasia of the facial or vestibulocochlear nerves is best diagnosed with high-resolution T2-weighted MRI. On a sagittal reconstruction, the facial nerve occupies the anterosuperior quadrant of the IAC, the cochlear nerve, the anteroinferior, the superior and inferior vestibular nerves, and the posterosuperior and posteroinferior quadrants, respectively (Fig. 8.18). Absence or hypoplasia may occur as an isolated abnormality or as a part of entities such as the Möbius syndrome, where absence of the sixth nerve coexists. Evaluation for cochlear nerve deficiency (hypoplasia or absence) is important in the work up for cochlear implantation. Cochlear nerve deficiency can be observed both in association with congenital or acquired (sensorineural hearing loss) SNHL. When present, a hypoplastic internal auditory canal is suggestive for congenital cochlear nerve deficiency.
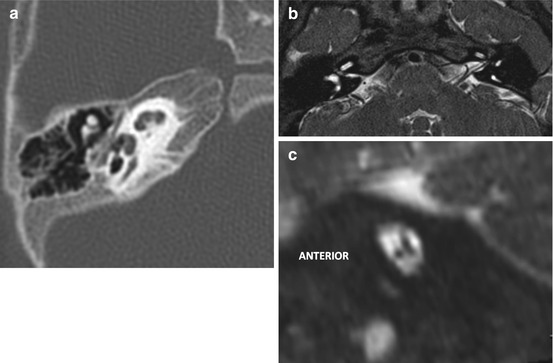
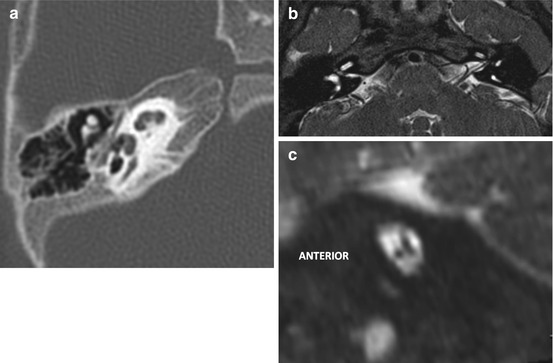
Fig. 8.18
(a, b) Absence of the cochlear nerve. Note the lack of a cochlear aperture in (a) and the diminutive IAC in (b). The left IAC is normal. (c) Absence of the facial nerve. The anterosuperior quadrant of the IAC where the facial nerve would normally be present is empty
Box 8.2. Checklist of Inner Ear Anatomy
Presence of three (2 ¾) distinct cochlear turns |
Presence of a modiolus |
Presence of an interscalar septum |
Patent cochlear aperture |
Size of the internal auditory canal |
Presence of all three semicircular canals |
Size of the vestibule |
Caliber of the vestibular aqueduct – the diameter should not exceed that of the adjacent posterior semicircular canal |
Box 8.3. CHARGE Association: Head and Neck Findings
Temporal bone |
|---|
Inner ear |
Absence of one or more semicircular canals |
Dysplastic vestibule |
Dysplasia/absence of one or more cochlear turns |
Small/absent cochlear aperture |
Enlarged vestibular aqueduct |
Middle ear |
Underpneumatized middle ear cleft |
Dysplastic ossicles |
Oval window atresia |
Round window atresia |
Variable course of facial nerve – can lie directly over atretic oval window |
Nasal cavity |
Choanal atresia |
Orbit |
Coloboma with/without microphthalmia |
Skull base |
Basiocciput hypoplasia and basilar invagination |
Jugular bulb diverticula |
Petrosquamosal sinus |
When large, the jugular bulb is hypoplastic |
May be injured if unrecognized at cochlear implantation |
8.4 Inflammatory Disorders
8.4.1 External Ear Inflammation
Inflammation of the external ear may manifest as an acute process (acute otitis externa, malignant external otitis) or be chronic in nature (keratosis obturans, cholesteatoma, medial canal fibrosis). Simple acute external otitis is not usually imaged.
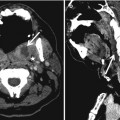
Malignant otitis externa (MOE) (Fig. 8.19) is usually caused by Pseudomonas bacteria and is typically encountered in the elderly and diabetic population. It is a type of rapidly spreading skull base osteomyelitis that begins in the EAC. Infection spreads from the floor of the cartilaginous EAC to the skull base through the fissures of Santorini. As the process extends to involve the skull base foramina, cranial neuropathies begin to manifest. Imaging is best achieved with a combination of CT and MRI. Subtle osteolysis at the bony–cartilaginous junction of the EAC may be the only finding on CT. On MRI, the infiltrative nature of the process is revealed by replacement of the fat that is normally encountered in the skull base, such as in the clivus, petrous apex, pterygopalatine fossa, and parapharyngeal spaces. Replacement of fat is best depicted on precontrast T1-weighted images. Postcontrast fat-suppressed T1-weighted images demonstrate abnormal enhancement in the areas involved. Abscesses are revealed as areas of low signal intensity with thick surrounding enhancement. These findings are, however, nonspecific and may be seen with aggressive neoplasms such as invasive nasopharyngeal carcinoma, lymphoma, and metastases. The presence of discrete abscesses, however, points to osteomyelitis.
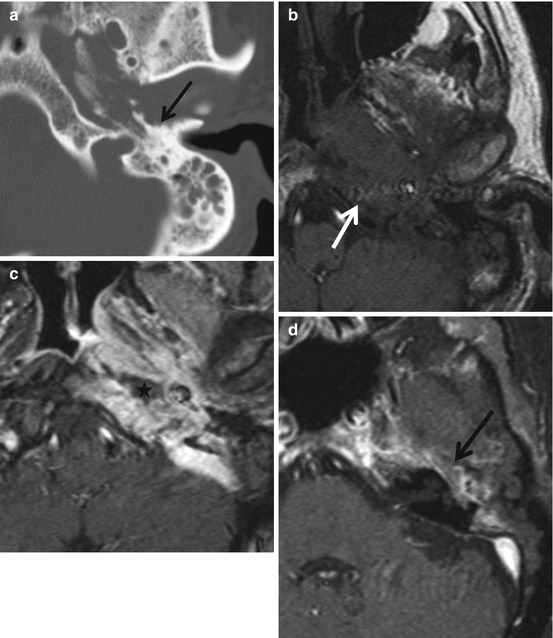
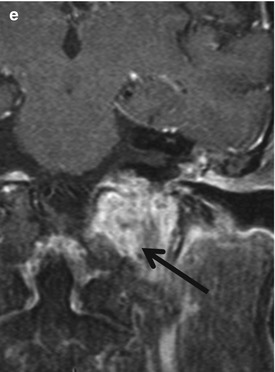
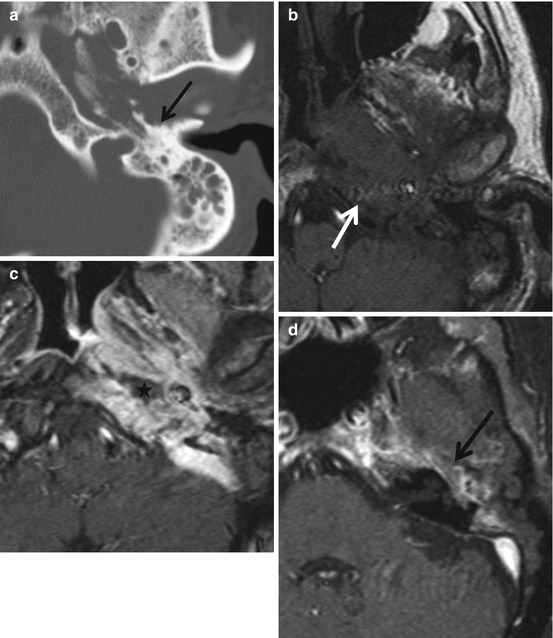
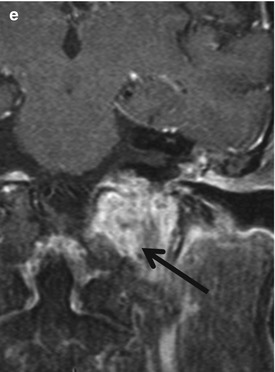
Fig. 8.19
Malignant external otitis. Elderly diabetic patient with otalgia and cranial nerve palsies. (a) Destruction of the walls of the bony EAC, glenoid fossa, and petrous ridge (arrow). Subtle bone destruction in the anterior wall of the EAC at the bony–cartilaginous junction may be seen in early stages of MOE. This may spread to involve the remainder of the temporal bone and clivus as seen on the unenhanced T1-weighted image (arrow, b) where replacement of the clival marrow, and an ill-defined inflammatory soft tissue process involving the skull base, extending to the lateral nasopharyngeal wall are evident. On the enhanced fat-suppressed image (c), a small abscess deep to the fossa of Rosenmuller (asterisk) is noted. In (d), extension of inflammation to involve the petrous temporal bone in the region of the geniculate ganglion (arrow) is observed. Extension into the jugular foramen is demonstrable in (e)
Cholesteatomas of the external auditory canal manifest clinically as otalgia associated with pearly white soft tissue, usually in the posteroinferior aspect of the EAC, adjacent to the tympanic membrane. Although cholesteatomas usually produce irregular bone destruction, smooth bony remodeling may also be seen (Fig. 8.20). In keratosis obturans, a bilateral condition that presents with fairly acute otalgia, the EACs are expanded smoothly by keratin debris.
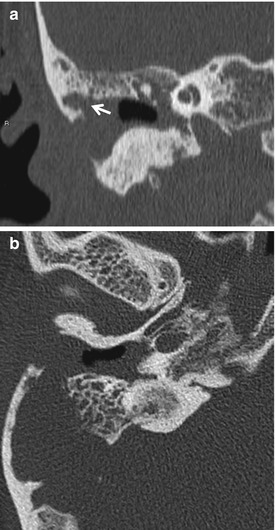
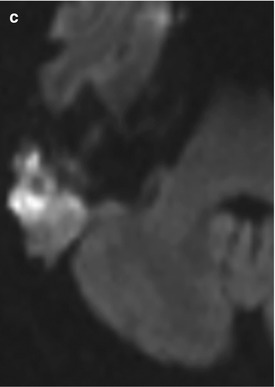
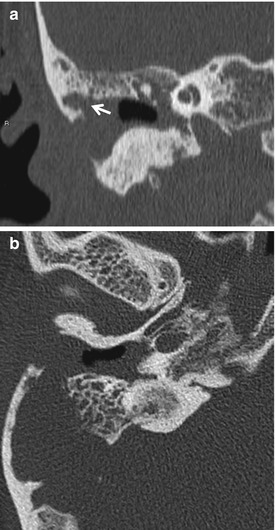
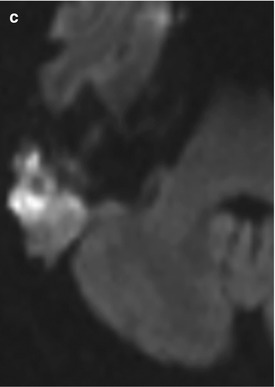
Fig. 8.20
Invasive external canal cholesteatoma in a patient with chronic otalgia. Note destruction of the roof of the EAC by cholesteatoma in (a). In (b), invasion of the mastoid air cells by cholesteatoma is evident. The diffusion-weighted image (c), reveals that almost all of the soft tissue in the EAC and mastoid system is cholesteatoma
Medial canal fibrosis is a chronic condition where an indolent tympanic membrane inflammation progressively leads to fibrous obliteration of the medial EAC lumen, resulting in a “false fundus” appearance clinically and on CT (Fig. 8.21).


Fig. 8.21
Medial canal fibrosis. Note the “false fundus” appearance of the EAC produced by fibrous tissue
8.4.2 Middle Ear and Mastoid Inflammation
8.4.2.1 Acute Otitis Media (AOM)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree