TEMPORAL BONE AND SKULL BASE OSTEOMYELITIS OTHER THAN NECROTIZING OTITIS EXTERNA
KEY POINTS
- Computed tomography can make the presumptive diagnosis of skull base osteomyelitis and necrotizing otitis externa when the disease is beyond its early stage and produces at least some bone erosion.
- Computed tomography and magnetic resonance imaging may be useful in treatment surveillance.
- Radionuclide studies also can help to establish the diagnosis and assess the response to antimicrobial therapy.
INTRODUCTION
Etiology
Skull base osteomyelitis (SBO) other than that related to necrotizing otitis externa (NOE) discussed in Chapter 114 is a very uncommon disease (Figs. 16.1, 16.2, and 114.1–114.5). The portal of the infection might still be the middle ear or mastoid, but the disease is often bilateral and relatively symmetric, making some other source related to the ear, such as the nasopharynx or eustachian tube, possible. Aside from the middle ear and mastoid, the sphenoid sinus may be a recognizable source. Often, the site of original infection is not proven, and the specific organism might not be established.
Proven cases with a known cause outside of that due to NOE and Pseudomonas aeruginosa are sporadic. Other organisms, including Staphylococcus aureus, Salmonella, Proteus mirabilis, aspergillosis/mucormycosis, actinomycosis (Fig. 16.2), Cryptococcus, and blastomycosis, may also be causative agents.
Prevalence and Epidemiology
This is a sporadic condition that occurs principally in older patients. The disease is likely more common in immune-compromised patients, but the cases are so few that this is not a proven risk factor akin to the risks known to be present for NOE in diabetics.
Clinical Presentation
Patients typically will present with otalgia and headaches and perhaps fever and signs of septicemia. Cranial neuropathies are often presenting complaints or are discovered during the initial physical examination; these may affect any of the cranial nerves II through XII.
Pathophysiology
Anatomy
The anatomy of interest is that of the entire temporal bone as described in detail in Chapter 104 and the central skull base (Chapter 78) and cavernous sinus (Chapter 44). It is also useful to understand the relationship of the surrounding anatomy, including the temporomandibular joint (Chapter 101), masticator, and parapharyngeal spaces (Chapter 142), and nasopharynx (Chapter 184).
Pathology and Patterns of Disease
This may be a spreading necrotizing infection of the soft tissues that affects bone from the outside to the inside as seen in NOE. It may also be a primary osteomyelitis beginning in bone and spreading beyond its confines. The earliest findings may be nonspecific soft tissue swelling within the parapharyngeal spaces and nasopharynx.
In the next stage of the disease, bone will be demineralized. The specific site of bone destruction varies; by the time of presentation, it is usually extensive and may spread to involve both sides. The disease appears to often start on one side, spreading along the mastoid and petrous portions of the temporal bone to the petrous apex and adjacent basiocciput/clivus (Figs. 16.1, 16.2, and 115.1–115.6). The pattern in some cases is very much like that seen in NOE, but the patients are not diabetic and the organism is not predominantly pseudomonas. Erosion along the walls of the external auditory canal and into the mastoid air cells may be present, but the mastoid changes are often reactive to adjacent infection; thus, a mastoidectomy approach for tissue sampling and culture does not often lead to a specific diagnosis. Bone may also become intensely sclerotic, and a mixed sclerotic and lytic pattern may result. Frank subperiosteal or other abscess formation may be present.
Intracranial spread is typically limited to the dura and epidural space as phlegmon and/or abscess.
Pathologically Altered Function
Typically, there are no specific deficits created early in the pathogenesis of the infection. More extensive or aggressive lesions can cause cranial neuropathies. Inner ear dysfunction secondary to labyrinthitis and intracranial and vascular complications are likely more common than those seen with NOE.
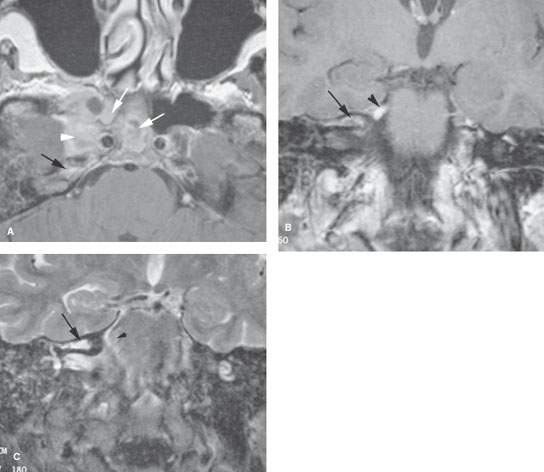
FIGURE 115.1. Sphenoid sinus origin of fungal skull base osteomyelitis. Magnetic resonance imaging examination. A: Contrast-enhanced T1-weighted (T1W) image showing disease within the sphenoid sinus (white arrows) spreading to the adjacent cavernous sinus (arrowheads) and then secondarily to the petrous apex (black arrows). B: T1W coronal image showing that the disease has spread from the sphenoid bone into the superior labyrinthine air cells (arrow). Also note inflammatory enhancement of the trigeminal nerve (arrowhead). C: T2-weighted coronal image showing the inflammatory mucosal thickening in the petrous apex air cells (arrow) and edema at the root entry zone of the trigeminal nerve (arrowhead).
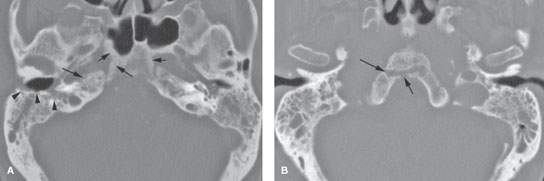
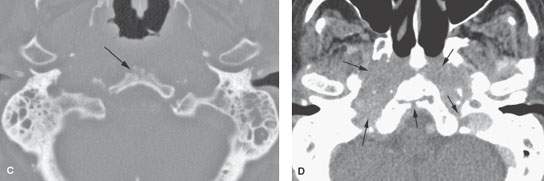
FIGURE 115.2. Computed tomography of a nondiabetic patient with pseudomonas osteomyelitis of the skull base but minimal external auditory canal erosion to suggest necrotizing otitis externa (NOE) (Chapter 114) and an imaging pattern not typical of NOE in its symmetry and bilateral central skull base invasion. A–C: Middle ear and mastoid mucosal thickening is present on both sides. The clivus is eroded and sclerotic changes are present in the petroclival fissures (arrows) and in the cortical surface of the sphenoid bone with an unusual tract through the lower clivus (arrows in B). The mastoids and external canals are minimally eroded considering the overall extent of bilateral disease. D: There is soft tissue swelling in the jugular foramen, retropharyngeal space, and throughout the nasopharynx.
FIGURE 115.3. Skull base osteomyelitis presenting in a nondiabetic and not obviously immune-compromised patient with multiple cranial nerve deficits and headaches. A, B: Computed tomography study showing extensive sclerosis of the central and posterior skull base (A) and areas of bone erosion (arrows in B). C: Soft tissue views showing an extensive bilateral infiltrating process of the nasopharynx, retropharyngeal space, and parapharyngeal spaces encasing both distal carotid sheaths to the skull base (arrows). The patient was treated empirically with antibiotics, and all changes and symptoms resolved.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree