TEMPORAL BONE TRAUMA
KEY POINTS
- Computed tomography is the primary study for evaluating a patient with temporal bone trauma.
- The concept of a transverse versus longitudinal fracture is not really useful and should not limit or in any way bias a diligent search in every case for all critical injuries.
- Potential injury to the facial nerve and carotid artery, as well as posterior fossa hematomas, must be reported verbally and promptly upon completion of the study.
- Delayed complications, including cerebrospinal fluid leakage, and potential routes of meningitis can be anticipated from fractures and associated findings such as pneumocephalus.
Trauma to the temporal bone is most commonly due to blunt-force skull injuries as a result of motor vehicle accidents, falls, assaults, and sports injuries. Penetrating trauma is much less common and often due to gunshot wounds. Unexpected iatrogenic trauma is unusual.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
All of the temporal bone anatomy must be completely understood to evaluate the trauma patient. This is discussed in Chapter 104.
In particular, the detailed anatomy of the facial nerve canal and carotid canal is of most importance in critical acute management decisions. The anatomy of the ossicles and inner ear will enter more into subacute and chronic clinical decision making with regard to possible restoration of posttraumatic hearing deficits. The anatomy of the mastoid and middle ear roofs and posterior walls will be important in assessing possible complicating posttraumatic cerebrospinal fluid (CSF) leakage, meningitis following trauma, and/or acquired meningocele or encephalocele.
IMAGING APPROACH
Techniques and Relevant Aspects
Specific protocols for computed tomography (CT) and magnetic resonance (MR) studies for investigating temporal bone trauma appear in Appendixes A and B. Traumatic conditions are typically studied simply with dedicated non–contrast-enhanced CT studies of the temporal bone acutely. Other imaging studies are typically not necessary initially. Computed tomographic angiography (CTA) may be used to identify carotid complications if fractures cross the carotid canal or symptoms or signs dictate that this is necessary.
Pros and Cons
CT provides a critical assessment of the bony structures related to facial nerve function, conductive hearing, and vestibular and cochlear function. Bone injury may also provide clues to sources of CSF otorrhea, a cause for posttraumatic meningitis, or defects that might lead to herniation of intracranial contents into the middle ear or mastoid. CTA can be added to evaluate carotid injuries.
Magnetic resonance imaging (MRI) is usually not required. It may be used to confirm a meningocele or encephalocele.
Controversies
The concept of classifying temporal bone fractures as longitudinal or transverse and somehow relating the odds of injuries to specific structures such as the facial nerve canal is not useful. It is unfortunate that such concepts are reinforced on various examinations taken by trainees. In fact, what really matters is that any fracture places all critical structures at risk, and all must be systematically evaluated regardless of the dominant pattern of injury. This chapter will not use this system of classification. Abandonment of this relatively useless categorization has recently been advocated in the clinical literature.1–3
The carotid canal may be fractured but is only infrequently associated with arterial injury of any significance, although CTA is now almost always done when carotid canal injury is noted. Some would suggest reserving CTA for selected patients, although the proper section criteria are not entirely clear or agreed upon in any consensus-based documents.
BLUNT-FORCE, PENETRATING, AND IATROGENIC TEMPORAL BONE TRAUMA
Etiology
Trauma to the temporal bone is most commonly due to blunt-force skull injuries as a result of motor vehicle accidents, falls, assaults, and sports injuries. Penetrating trauma is much less common and often due to gunshot wounds. Unexpected iatrogenic trauma is unusual and will occur in otomastoid surgery but more often during neurosurgery as an untoward complication.
Prevalence and Epidemiology
These are sporadic occurrences. When associated with other more life-threatening head and bodily injury, their effects may not be noticed acutely. Some injuries will become apparent only when revealed by complications such as otorrhea, otomastoiditis, and meningitis or thromboembolic disease if the carotid is injured.
Clinical Presentation
Trauma to the temporal bone can cause conductive hearing loss either through ossicular disruption or fluid/blood within the middle ear cavity. Sensorineural hearing loss will accompany fractures through the otic capsule. However, acutely, facial nerve paralysis or thromboembolic complications from a carotid injury will be the most pressing concerns.
Conductive, mixed, or sensorineural hearing loss or vestibular dysfunction may be present. CSF otorrhea may be present immediately or as a delayed complication. Complicating acute or chronic otomastoiditis may produce fever and ear pain. Signs and symptoms of meningitis may appear as a result of breaches in temporal bone structures. If the glenoid fossa is involved, TMJ discomfort or dysfunction may be present.
Pathophysiology and Patterns of Disease
Basic Mechanisms of Blunt-Force and Other Injury
As discussed in Chapter 104, the normal essentially “X” configuration of the skull base helps to explain the mechanism of blunt-force trauma. Such an event can squeeze the skull between the lateral margin of the orbit and the opposite mastoid tip, in which case a compression type of injury of the temporal bone region might occur (Figs. 120.1–120.7). A force applied to the mandible that is transmitted through the external auditory canal causes a sheering action that involves the more lateral portions of the temporal bone. A compression of the skull from bilateral application of pressure causes both shearing and compression to be applied to the temporal bone with disruption of its posterior table and impaction fractures of the middle ear cleft. Blunt-force trauma in the high parietal region can cause a fracture along the long axis of the temporal bone. The parietal compressive force causes the skull to momentarily indent and then recoil. The vector of force radiates in a starlike pattern from center of the point of injury, with one of the fracture lines going down the temporal bone. This same type of indentation and recoil phenomena can occur with occipital injuries, creating transverse fractures.
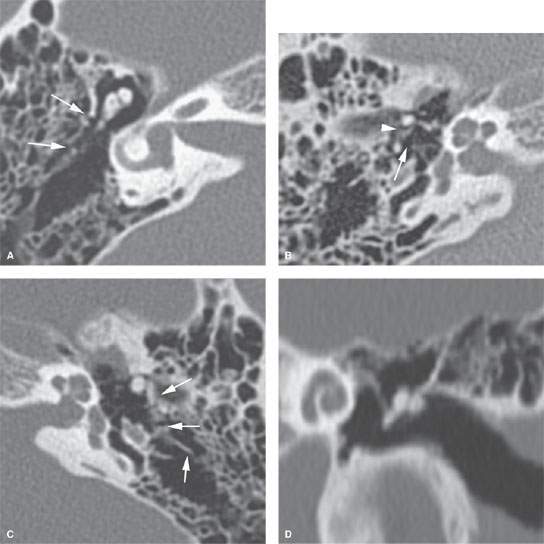
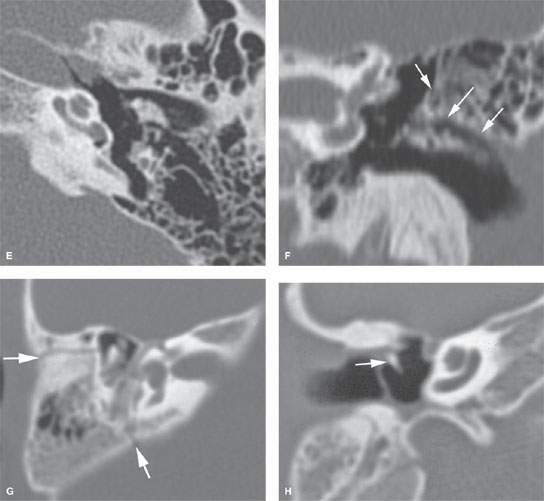
FIGURE 120.1. Computed tomography findings in posttraumatic conductive hearing loss due to ossicular disruptions in two patients. A–F: Patient 1 with bilateral fractures. In (A) and (B), on the right there are relatively subtle fractures in the lateral epitympanic wall (arrows in A) with malleoincudal (arrowhead in B) and incudostapedial disruption (arrow in B) present. In (C), on the left, horizontal fracture lines are running through the mastoid and lateral epitympanic wall (arrows in C). The incus is displaced, and there is gross malleoincudal and incudostapedial dislocation (D–F). G, H: Patient 2. There is a fracture through the roof of the external auditory canal and epitympanum (arrows in G) with associated fracture dislocation through the neck of the malleus resulting in displacement of its manubrium (H). This is the least common ossicular injury.
Penetrating trauma is usually due to a gunshot wound (Fig. 120.8). Direct injury, as well as concussive forces, deposited in the bullet path will lead to essentially the same problems as encountered in blunt-force trauma.
Iatrogenic trauma during neurosurgical procedures will most often be due to inadvertent drilling or cutting into the mastoid or bony labyrinth. If unrecognized and therefore not repaired, this can lead to CSF leakage and infectious complications. Such encounters are typically recognized and repaired and actually required during otologic procedures. If the repair is inadequate, complications may be later in their presentation. Disruption of the ossicles is uncommon during neurosurgery but may occur in otologic procedures4 (Fig. 120.3C).
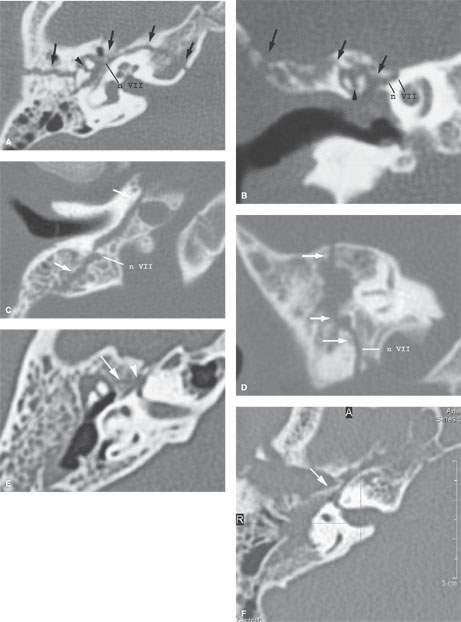
FIGURE 120.2. Temporal bone fracture associated with facial nerve injury in four patients. A, B: Patient 1 had facial nerve paralysis immediately after the trauma—a fracture (arrows) through the roof of the external auditory canal and extending to the petrous apex involves the anterior genu of the facial nerve (n VII). There is also malleoincudal disruption (arrowhead). C, D: Patient 2 had delayed onset of facial nerve paresis due to a fracture (arrows) running along the vertical (mastoid) segment of n VII. E: Patient 3 had immediate onset of facial nerve paresis due to a subtle fracture (arrow) running along the first genu segment of n VII. There was full recovery of facial nerve function with conservative management. F: Patient 4 had immediate onset of facial nerve paralysis due to a fracture (arrow) displaced into the first genu segment of n VII. No function was recovered.
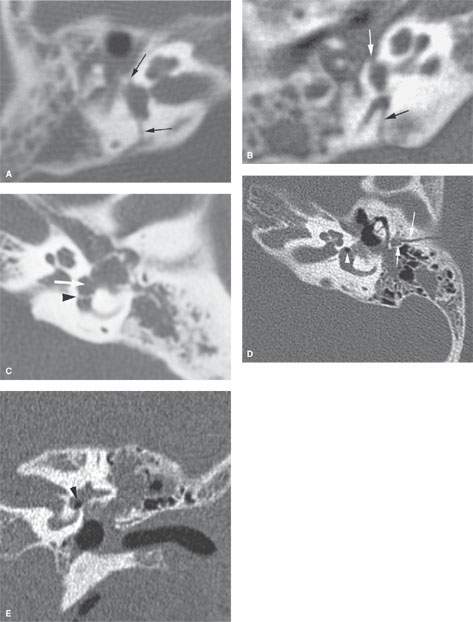
FIGURE 120.3. Fractures involving the oval window and stapes foot plate system in three patients. A, B: Patient 1 is a 10-year-old boy who suffered from recurrent meningitis. He has a history of head trauma, and computed tomography reveals a fracture (arrows) of the petrous bone running through the vestibule; the oval window and likely the stapes foot plate are fractured. Partial opacification of the middle ear cavity and mastoid is present, likely related to leakage of fluid from the membranous labyrinth. C: An oval window fistula (white arrow) can be due to iatrogenic injury. In Patient 2, this occurred during dissection of a cholesteatoma off the stapes. The stapes is fractured, and the foot plate is displaced into the vestibule (arrowhead). D, E: In Patient 3, the oval window fracture extension from that along the mastoid (arrows) resulted in pneumolabyrinth (arrowheads).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








