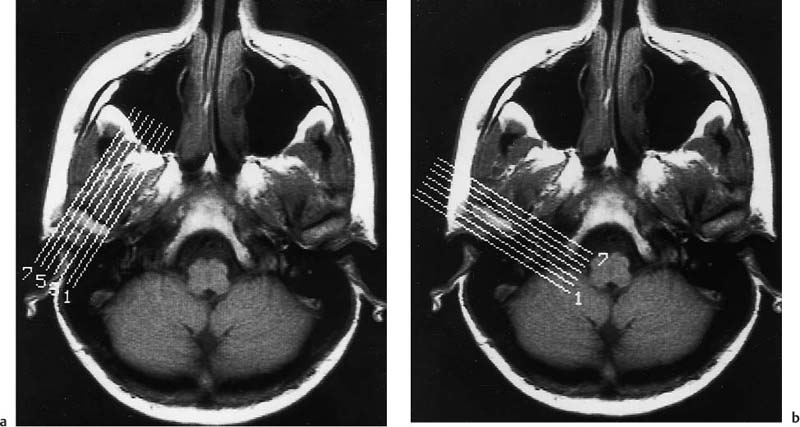
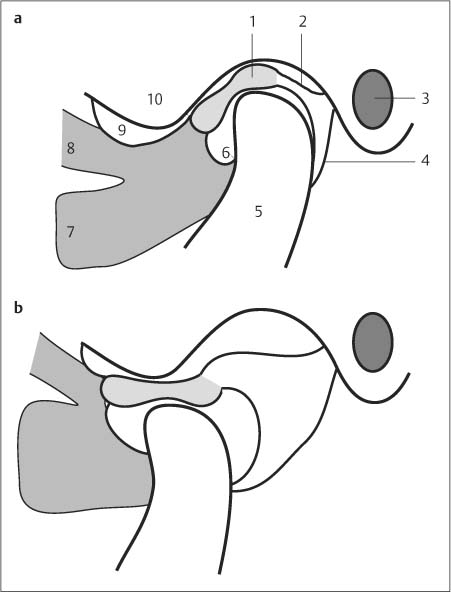
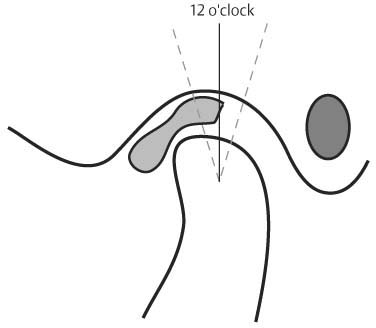
9 Temporomandibular Joint The temporomandibular joint (TMJ) is imaged to detect clinically suspected anomalies and dysfunctions. The role of conventional radiology is limited since only osseous changes are identified with any degree of confidence. Such changes, however, appear only late in diseases affecting this region. In the 1970s and 1980s, arthrotomography was used to diagnose diskoligamentous disorders (13, 25). CT achieves an excellent visualization of osseous changes but its sensitivity for diagnosing disorders of the disk is inadequate (11). With the introduction of MRI, the soft tissue structures of the joint, especially the articular disc, could be imaged noninvasively. MRI has completely replaced invasive and painful arthrography and has become the modality of choice for diagnosing pathologic changes of the TMJ. The examination is performed with the patient supine. The patient is first examined with the mouth closed. The examination continues with the mouth open about 30 mm to achieve an adequate movement of the disk and the mandibular condyle. To keep the mouth open, adjustable jaw openers (2) can be used, or alternatively, simple dental wedges made of plastic or wood. For dynamic studies, in particular, incremental jaw openers are necessary (32). For the examination of the TMJ, it is essential to use a surface coil with a small diameter (5–12 cm) to achieve an adequate spatial resolution with a good signal-to-noise ratio (SNR). The coil is positioned with its center 1–2 cm anterior to the external auditory canal. Since both joints, constituting one functional unit of mastication, show an abnormality in up to 80% of TMJ disorders, the imaging should be bilateral. The simultaneous assessment of both joints can be achieved with special dual coils that are available for most units. The examination begins with a fast T1-weighted sequence, obtained as a localizer in the transverse plane with a body coil and a large field of view (FOV). This allows the position of the joints and the transverse axes of the condyles to be determined. On the basis of this transcondylar image, additional high-resolution sequences are planned for imaging with the mouth open and closed (Fig. 9.1). The surface coils should cover a field of view of 8–12 cm. Continuous sections of 3 mm width and SE images with four signal averages are necessary for adequate detail. Decreasing the section thickness from 3 to 1.5 mm improves the delineation of the articular structures in the coronal plane (37). Thin sections are needed for visualizing complex deformities and can be obtained with 3-D-GRE techniques. With a section thickness of 3 mm, seven to nine sections are generally sufficient to encompass the entire joint. Next, a parasagittal section is selected, with its angulation perpendicular to the long axis of the condular head, as determined from the survey image (Fig. 9.1). The section includes the external auditory canal, floor of the temporal fossa and the ascending mandibular ramus. The articular disk and other articular structures are best seen on the parasagittal plane. The T1-weighted SE sequences (TR = 600 msec, TE 15–30 msec) provide a good anatomic resolution of the structure of the disk, together with good differentiation of muscle, ligaments, and bones. Maintaining the closed mouth position is crucial for evaluating the disk position since even partial opening of the mouth can reduce a displaced disk (5, 21). As the low-signal disk is directly between the low-signal cortex of the condyle and mandibular fossa when the mouth is closed, defining configuration and signal intensity of the disk can be difficult. In these cases, delineating the disk can be improved by partially opening the mouth (5). Furthermore, an anterior displacement of the disk becomes more conspicuous with increasing translation (21). Thereafter, images are obtained with the mouth open, preferably with T1-weighted SE sequences. Since imaging with the mouth open is primarily performed to assess the position and mobility of the disk, the number of signal averages can be lowered to shorten the acquisition time without appreciable loss of image quality. Moreover, keeping the open-mouth position for some time is uncomfortable for the patient and induces involuntary swallowing due pharyngeal pooling of saliva. Avoiding such introduced motion artifacts is another reason to keep the acquisition time short. Fig. 9.1a, b Axial sections through the level of the mandibular condyles with lines indicating the a oblique sagittal and b oblique coronal sections. If the patient has a repositioning appliance (protrusive splint), the examination should be supplemented by a sagittal image with the repositioning appliance in place to document the reduction or adopted position of the disk. Paracoronal sections parallel to the long axis of the condyle should be added for both joints (Fig. 9.1). These sections are best for assessing the degree of sideways disk displacement (14). In particular, for a disk that is not well identified on the sagittal sections, coronal sections are mandatory. T2-weighted SE images have inferior topographic resolution compared with T1-weighted sequences. Because of their high tissue differentiation, T2-weighted SE sequences (TR = 1800–2000 msec, TE 80–120 msec) are suited for detecting a joint effusion in rheumatoid or septic arthritis and after trauma (27). Furthermore, T2- weighted images can assess the degree of disk hydration, though its clinical relevance is still undetermined (8). If a space-occupying process is the reason for the examination, the entire region of the TMJ should be included on transverse T2-weighted images (TR = 2000, TE 25 msec, 90 msec), supplemented by transverse and coronal T1-weighted SE images after IV administration of Gd-DTPA at 0.1 mmol/kg body weight. Contrast-enhanced images have also been found advantageous in diagnosing any involvement of the TMJ in rheumatoid conditions. Using fast GRE sequences can clearly reduce acquisition times. Though the disk is usually well delineated on GRE images, the anatomic resolution of the surrounding structures and the disk itself is markedly inferior to SE images. Consequently, GRE images are less suitable for evaluating degenerative changes of the disk. A further disadvantage of these sequences is their sensitivity to pulsation and motion artifacts as well as to susceptibility artifacts (dental fillings). The fast sequences (FISP– 2 D, FFE, etc.) are suitable for obtaining dynamic motion studies with stepwise acquisition at various mandibular positions within a reasonable time frame (CINE technique) (2, 33). A disadvantage of static MR images restricted to two mandibular positions is their inability to follow the repositioning of the disk when opening the mouth, especially in cases with marked disk displacement. The dynamics and time of disk repositioning can be clinically relevant. The use of a sequential acquisition of several mandibular positions, controlled by a mechanical mouth-opening device, can yield a pseudodynamic visualization of the movements during mouth opening by playing the individual images in a CINE loop. With examination times of less than one minute–depending on the equipment used–even the endpoints of mandibular positions can be documented. Translation, rotation, and sequence of disk reposition as well as condylar hypermobility can be assessed, particularly articular hypermobility with condylar subluxations in front of the vertex of the articular tubercle, which cannot be assessed with static MRI employing conventional SE techniques (18). While a CINE loop displaying the motions of the TMJ is impressive, its therapeutic ramifications cannot yet be conclusively determined (1). A disadvantage of this method is the passive mouth opening, which distorts the intrinsic function. Finally, the quality of the individual images is still rather poor. The TMJ is a diarthroidal joint and constitutes the articular junction between the mandible and the temporal bone. The lentiform to ellipsoid condylar head arises from the condylar process of the mandibular ramus. Its transverse diameter exceeds its sagittal diameter. The long axis of the condyle is perpendicular to the condylar process, resulting in an anterolateral to posteromedial tilt of the axis and the articular fossa of 15–25 degrees relative to the frontal plane. The concave articular fossa is limited anteriorly by the articular tubercle and posteriorly by the osseous wall of the external auditory canal (Fig. 9.2a). The depth of the articular fossa as well as the degree of angulation of the dorsal slope of the articular tubercle is variable. The osseous articulating surface of the articular fossa, the articular tubercle and the mandibular condyle are covered by thin fibrocartilage. A fibrocollagenous, movable meniscus, the articular disk, divides the joint into two completely separate compartments. The upper or meniscotemporal joint cavity is larger than the lower or meniscocondylar cavity. An anterior and posterior thickening of the disk, also referred to as the anterior and posterior band, are connected by a narrow intermediate zone, giving the disk a biconcave configuration. Anteriorly, the disk is attached to the joint capsule and the superior head of the lateral pterygoid. The bilaminar region is the posterior continuation of the posterior band of the disk. It consists of two fibrous leaflets, with the superior leaflet extending into the posterior aspect of the articular fossa to insert at the Glaser fissure in front of the external acoustic canal and the lower leaflet attached at the posterior aspect of the mandibular neck together with the joint capsule. The joint capsule is a thin, loose structure. Its attachment at the margin of the mandibular fossa of the temporal bone extends to the anterior slope of the articular tubercle. The capsule encompasses the condyle and attaches at the condylar neck. It is laterally and medially strengthened by fibers of connective tissue, while it is rather flaccid anteriorly and posteriorly. The sphenomandibular ligament, which is attached to the sphenoid spine of the temporal bone superiorly and to the mandibular foramen inferiorly, is medial and separate from the capsule. The stylomandibular ligament acts as a further stabilizing structure. Mandibular movements are controlled by the four masticatory muscles. The temporalis arises like a fan from the temporal fossa and inserts at the coronoid process. It is the strongest elevator of the mandible. The masseter arises from the zygomatic arch and inserts at the mandibular angle. The medial pterygoid, which extends from the pterygoid fossa to the mandibular angle, acts as the medial pendant to the masseter. These three muscles essentially function to close the mouth. Fig. 9.2a, b Diagrammatic drawing of the oblique sagittal plane with a closed and b open mouth and physiologic position of the disk. With the mouth open, the condyle reaches the apex of the articular tubercle. 1 = Disk 2 = Bilaminar region 3 = External auditory canal 4 = Joint capsule 5 = Condyles 6 = Lower synovial cavity 7 = Inferior head of the lateral pterygoid 8 = Superior head of the lateral pterygoid 9 = Upper synovial cavity 10 = Articular tubercle Oblique Sagittal Plane. This plane is parallel to the ascending mandibular ramus and usually displays the condyle as a hook-shaped structure. On the T1- weighted SE image, the low-signal cortex and the equally low-signal fibrocartilage cover of the condyle and mandibular fossa are easily distinguished from the fat-containing trabecular bone. Condyle and mandibular fossa are smoothly outlined and rounded. With the mouth closed, the condyle is centered in the mandibular fossa (Fig. 9.2). Owing to its composition of densely packed, intertwined fibrocartilage fibers with occasional embedded chondrocytes, the biconcave, elongated disk is delineated as a low-signal, homogeneous structure on T1-weighted SE sequences. A slight increase in signal intensity in the posterior band is seen in more than 50% of normal disks (8) and should not be considered pathologic without concurrent changes of form or location. With the mouth closed, the disk is located between the mandibular condyle and mandibular fossa of the temporal bone. The smaller anterior band is adjacent to the posterior slope of the articular tubercle. The thin intermediate zone is located between the anterior circumference of the condyle and the temporal articular surface (Fig. 9.4). The transition between the posterior band, posterior ligament, and the high-signal bilaminar zone does not deviate more than 10 degrees from a position vertically above the upper condylar pole (Fig. 9.3), the so-called 12 o’clock position, in 95% of asymptomatic joints (5). A position slightly more anterior is observed more frequently than a posterior one. Fig. 9.3 Schematic drawing illustrating the physiologic position of the disk. The disk is within ±10 degrees of the 12 o’clock position in 95% of normal cases. The bilaminar region, which consists of fibrovascular connective tissue, is attached to the posterior band and connects the disk with the posterior joint capsule. The transition between the low-signal disk and the high-signal bilaminar region is well delineated on the T1-weighted SE image, making it easy to identify the disk. If the localization of the disk is uncertain on the SE image, the delineation of the posterior band can be improved following enhancement of the retroarticular venous plexus after administration of Gd-DTPA (28). In our experience, it is rarely necessary to administer contrast medium to determine whether the disk is displaced. The upper layer of the bilaminar zone consists of fibroelastic tissue and is attached to temporal bone. The low signal structures occasionally seen in the bilaminar elastic fibers are attributed to the elastic fibers (12). Function of the Temporomandibular Joint.
Introduction
Examination Technique
 Patient Positioning
Patient Positioning
 Coil Selection
Coil Selection
 Sequences and Parameters
Sequences and Parameters
Special Examination Techniques
 Dynamic Studies
Dynamic Studies
Anatomy
 General Anatomy
General Anatomy
 Specific MR Anatomy and Variants
Specific MR Anatomy and Variants
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree