Hip pain is a common but potentially vexing clinical problem; symptoms may be protean, referred, and poorly localized. History and physical examination can be unreliable in discriminating between intra-articular and extra-articular origins of pain. MR imaging augments clinical evaluation by providing information about the hip joint as well as the periarticular structures, which can be a source of symptoms. This article presents an anatomy-based review of common and less common tendon pathologies on MR imaging, which are considered in the differential diagnosis of hip pain.
Key Points
- •
History and clinical examination may not reliably stratify those patients with arthritic pain from those with nonarthritic pain.
- •
MR imaging is an important adjunct to the clinical examination because of its ability to evaluate the joint as well as the periarticular structures, which can be a source of symptoms.
- •
An anatomy-based search process can facilitate MR imaging interpretation and ensure that both common and less common entities are considered in the differential diagnosis.
Introduction
One in 164 visits to family physicians is for hip pain. Unfortunately, hip pain can be a vexing clinical problem; symptoms may be protean, referred, and poorly localized. Moreover, history and physical examination have been found unreliable in discriminating between the intra-articular or extra-articular sources of hip pain. In approximately half of the patients studied, Martin and colleagues determined that extra-articular pathology was responsible for patient symptoms despite imaging evidence for labral abnormalities.
Overuse injuries, including tendinopathies, are on the rise. The higher level of performance of competitive and recreational athletes, an emphasis on the health benefits of physical activity leading to greater sports participation in all age groups, and increased longevity of the population probably all contribute to this trend.
These points stress the importance of considering tendon pathology in the differential diagnosis and the need for imaging in the work-up in patients with hip pain. MR imaging augments clinical evaluation by providing information about the hip joint as well as the periarticular structures, which can be a source of symptoms.
Imaging evaluation for extra-articular causes of hip pain necessitates knowledge of normal anatomy and common pathologic tendon conditions in this region.
Hip pain can be characterized as anterior, lateral, or posterior. The content of this review is organized using this anatomic approach ( Fig. 1 ):
- •
Anterior pain (excluding osteoarthritis): enthesial and proximal iliotibial band (ITB) pathology, disorders of the iliopsoas tendon (internal snapping hip and iliopsoas impingement), and disorders of rectus femoris
- •
Lateral pain: disorders of the hip abductor tendons and external snapping hip syndrome (ESHS)
- •
Posterior pain: disorders of the hamstring tendons

Disorders of the ischiofemoral space and groin pain are discussed elsewhere in this issue by Torriani and colleagues, and Zoga and colleagues, respectively.
Introduction
One in 164 visits to family physicians is for hip pain. Unfortunately, hip pain can be a vexing clinical problem; symptoms may be protean, referred, and poorly localized. Moreover, history and physical examination have been found unreliable in discriminating between the intra-articular or extra-articular sources of hip pain. In approximately half of the patients studied, Martin and colleagues determined that extra-articular pathology was responsible for patient symptoms despite imaging evidence for labral abnormalities.
Overuse injuries, including tendinopathies, are on the rise. The higher level of performance of competitive and recreational athletes, an emphasis on the health benefits of physical activity leading to greater sports participation in all age groups, and increased longevity of the population probably all contribute to this trend.
These points stress the importance of considering tendon pathology in the differential diagnosis and the need for imaging in the work-up in patients with hip pain. MR imaging augments clinical evaluation by providing information about the hip joint as well as the periarticular structures, which can be a source of symptoms.
Imaging evaluation for extra-articular causes of hip pain necessitates knowledge of normal anatomy and common pathologic tendon conditions in this region.
Hip pain can be characterized as anterior, lateral, or posterior. The content of this review is organized using this anatomic approach ( Fig. 1 ):
- •
Anterior pain (excluding osteoarthritis): enthesial and proximal iliotibial band (ITB) pathology, disorders of the iliopsoas tendon (internal snapping hip and iliopsoas impingement), and disorders of rectus femoris
- •
Lateral pain: disorders of the hip abductor tendons and external snapping hip syndrome (ESHS)
- •
Posterior pain: disorders of the hamstring tendons
Disorders of the ischiofemoral space and groin pain are discussed elsewhere in this issue by Torriani and colleagues, and Zoga and colleagues, respectively.
MR imaging technique
According to the American College of Radiology, plain radiographs of the pelvis and hip are the most appropriate imaging study for the initial evaluation of chronic hip pain. Radiographs may reveal fractures, osteoarthritis, hydroxyapatite crystal deposition diseases, and other common entities that may explain symptomatology. Initial radiographic findings and clinical information can then guide the choice of more advanced imaging. In cases of suspected musculotendinous etiology, noncontrast MR imaging is the next most commonly performed study because of its ability to diagnose the myriad potential osseous and soft tissue causes of hip pain around the pelvis.
Tendon pathology can be evaluated on standard MR imaging planes. MR imaging protocols can be standardized; the authors use 3 imaging protocols. All start with large field of view (FOV) coronal short tau inversion recovery (STIR) images of the pelvis using the body coil; this provides an overview of the pelvis and allows a radiologist/technologist to modify the imaging protocol to evaluate unexpected pathology if necessary.
The protocol for the bony pelvis continues with large FOV imaging of the pelvis using anatomic (T1 and proton density [PD]) and fluid-sensitive (fat-suppressed T2 or PD) sequences, and a sagittal sequence through the affected side if there is symptom laterality.
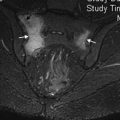
In patients younger than 50 years of age (in whom diagnosing intra-articular pathology is relevant to management), axial fat-suppressed T2, axial oblique PD, sagittal fat-suppressed PD, and coronal PD are performed using a high-resolution technique that uses a flexible surface coil wrapped around the affected hip ( Table 1 ). The affected hip is positioned closest to isocenter with the surface coil in place at the start of the examination; off-isocenter position optimizes imaging of the affected hip and in the authors’ practice does not have a significant impact on the diagnostic quality of the large FOV sequence for the remainder of the pelvis ( Fig. 2 ).
| Sequence | Plane | Slice Thickness | Tr | Te | FOV | Matrix | Comment |
|---|---|---|---|---|---|---|---|
| STIR | Cor | 5 mm | 4000 | 35 | 350 | 192 × 256 | Cover whole pelvis |
| PD TSE | Cor | 3 mm | 3000–3500 | 34–38 | 160 | 192 × 256 | Unilateral |
| PD TSE FS | Sag | 3 mm | 2900–3000 | 22–35 | 160 | 256 × 256 | Unilateral |
| T2 TSE FS | Ax Straight | 3 mm | 3500–4500 | 40 | 200 | 224 × 256 | Unilateral |
| PD TSE | Obl Ax | 3 mm | 2800–3000 | 33 | 140–160 | 224 × 256 | Unilateral |
For patients over age 50 (in whom marrow abnormalities, including fractures and metastatic disease, may be a concern), the large FOV STIR coronal sequence is followed by a large FOV T1 coronal sequence ( Table 2 ). Subsequent coronal, sagittal, and axial images are done of the affected hip only.
| Sequence | Plane | Slice Thickness | Tr | Te | FOV | Matrix | Comment |
|---|---|---|---|---|---|---|---|
| STIR | Cor | 5 mm | 4000 | 35 | 350 | 192 × 256 | Cover whole pelvis |
| T1 SE | Cor | 5 mm | 500–735 | 12 | 350 | 240 × 320 | Cover whole pelvis |
| PD TSE | Cor | 3 mm | 3000–3500 | 34–38 | 160 | 192 × 256 | Unilateral |
| PD TSE FS | Sag | 3 mm | 2900–3000 | 22–35 | 160 | 256 × 256 | Unilateral |
| T2 TSE FS | Ax Straight | 3 mm | 3500–4500 | 40 | 200 | 224 × 256 | Unilateral |
Skin markers placed in the region of symptoms can help ensure adequate imaging coverage and direct attention to the region of clinical concern during image interpretation.
General considerations/pitfalls/caveats
Tendons are designed to transmit forces generated from muscle contraction to bone. Their tensile strength is owed in large part to densely packed and aligned collagen fibers. Thus, healthy tendons do not rupture under normal conditions. Repetitive submaximal tendon loading due to chronic overuse, however, results in tendon degeneration; this reduces the tendon’s strength and puts it at risk for failure.
Tendons undergo stereotypic changes with aging and injury regardless of their location. This alters their size, signal, and morphology on imaging. Peritendinitis represents the earliest injury, and manifests as increased T2 signal around the tendon ( Fig. 3 ). Tendinosis or tendinopathy is the result of mechanical, degenerative, or overuse injuries. Whether the result of myxoid, hypoxic, hyaline, fatty, fibrinoid, or calcific degeneration, structural changes and accumulated degradation byproducts leave the tendon more prone to injury. This is reflected on MR imaging as an increase in size and signal heterogeneity (see Fig. 3 ). Tears within a weakened tendon are identified as fluid-filled defects on PD, T2, or STIR sequences ( Fig. 4 B). Partial thickness tears may heal over time and leave the tendon thickened, thinned, irregular, or lax. Full-thickness tears are defined as complete fiber discontinuity and can be associated with tendon retraction, fluid gap, and muscle atrophy ( Fig. 5 ).
Spuriously increased intratendinous signal may be the result of magic angle phenomenon. Seen on sequences with short echo times, the signal in a tendon may increase as the orientation of the intratendinous collagen is aligned at an angle with the main magnetic field. This is greatest at 55% and can be mitigated with the use of longer echo times (30 ms for gradient echo, 40 ms for spin echo, and 70 ms for fast spin-echo imaging at 1.5 T).
Decreased tendon signal can be related to the deposition of basic calcium phosphate, such as hydroxyapatite, in the setting of calcific tendinitis. This can be clinically silent; symptomatic crystal deposition is most common in patients in their 40s to 60s. The hip is the second most commonly affected joint; calcium deposits are most common around the greater trochanter (hip abductor tendons) and ischial tuberosity (hamstring tendons). They are also seen at the femoral insertion of the gluteus maximus tendon and at the origin of rectus femoris and vastus musculature ( Fig. 6 ). Initial patient presentation can be dramatic. The painful inflammatory response can manifest as bone and soft tissue edema and bone erosions, which can mimic infection or malignancy both clinically and on MR imaging. Although osseous involvement is rare, when present in the hip, the proximal linea aspera of the femur is most likely affected (see Fig. 6 A, B). Enthesial calcifications without a discrete soft tissue mass are substantiating evidence for this diagnosis on MR imaging. Plain radiographs and CT may help to confirm soft tissue calcifications when they are not evident on MR imaging (see Fig. 6 ).
“Treat the patient, not the imaging” could not be truer than in musculoskeletal imaging. Imaging-detected pathologic changes in the hip abductor tendons and proximal hamstring tendons are common in the asymptomatic population and underscore the point that not all tendinopathy is symptomatic. Imaging findings do not always correlate with clinical symptoms and it is the onus of the clinician to determine their relevance.
Anterior pain
- •
Disorders of the origin of the ITB
- •
Disorders of the iliopsoas tendon
- ○
Tendinopathy/tendon tears
- ○
Internal snapping hip
- ○
Iliopsoas impingement
- ○
- •
Disorders of the tendon origin of rectus femoris
Abnormalities of the Origin of the Iliotibial Band
As the attachment site of tensor fascia lata as well as the external and internal abdominal oblique, transverse abdominis, and gluteus medius, the iliac crest apophysis is at risk for injury in adolescent athletes. Seen in long distance runners between the ages of 13 and 25 years, iliac crest apophysitis is the result of repetitive submaximal traction of the unfused apophysis.
Pathology at origin of the ITB has also been recently reported in a small cohort of adult women from two disparate groups—young athletes and older overweight women.
Anatomy
The ITB represents a thickening of the fascial investiture of tensor fascia lata and gluteus maximus muscles. It originates at the iliac crest apophysis, which appears at approximately age 13 and fuses at age 25. The ITB divides into deep and superficial layers to envelop the tensor fascia lata muscle. At the hip, the ITB receives contributions from gluteus maximus fascia before it continues distally toward its major insertion on the anterolateral tibia at Gerdy tubercle.
The ITB helps stabilize the extended knee and hip, in part through the contraction of gluteus maximus and tensor fascia lata muscles, which tighten it. 16
Imaging
Adequate coverage is the most important aspect of imaging. The authors’ routine large FOV coronal STIR sequence of the pelvis always includes the iliac crest and allows evaluating this region on all patients. When pathology in this region is clinically suspected, this region is included in the axial and sagittal imaging FOV and both anatomic and fluid-sensitive sequences are performed.
In skeletally immature individuals, MR imaging findings of apophyseal widening (3–5 mm), physeal signal hyperintensity, and marrow and muscle edema on fluid-sensitive sequences have been reported after injury ( Fig. 7 ). Acute injury in adults manifests as edema in/around the ITB and within its iliac enthesis on fluid-sensitive sequences ( Fig. 8 ). Thickening of the proximal ITB can be seen on both anatomic and fluid-sensitive sequences in the chronic setting.
Abnormalities Related to the Iliopsoas Tendon
The iliopsoas tendon represents the distal termination of the psoas major and iliacus muscles. Together, these muscles flex the thigh, participate in lateral hip rotation, and contribute to pelvic stability when seated. Abnormalities related to the iliopsoas tendon include tendinopathy, tendon tears, internal snapping hip, and iliopsoas tendon impingement.
Anatomy
The iliopsoas compartment is an elongated extraperitoneal space that extends from the posterior mediastinum to the hip joint. It is roofed by the iliopsoas fascia and contains the psoas major and iliacus muscles, and, when present, the psoas minor muscle.
The long fusiform psoas major muscle arises from lumbar and T12 transverse processes; the fan-like iliacus muscle arises from the inner iliac fossa. As the 2 muscles merge at the L5-S2 level, a groove is formed at their lateral interface. It is through this fat-filled groove that the femoral nerve and iliolumbar vessels bundle are transmitted. The composite iliopsoas muscle exits the pelvis under the inguinal ligament; its tendon inserts on the lesser trochanter. In addition to its tendinous insertion, the iliacus muscle also inserts directly on the anterior femur and distal lesser trochanter. When fluid distended, the iliopsoas bursa can be seen between the iliacus muscle, the psoas tendon, and the anterior hip joint capsule.
Three things are important about the iliopsoas musculotendinous unit with regards to pathology. First, the tendons lie in a shallow groove in the pelvic brim as they exit the pelvis. Second, they course immediately adjacent to the anterosuperior aspect of the hip joint on the way to their insertion. Third, the iliacus and psoas tendons may merge together or attach separately on the lesser trochanter, the iliacus tendon more lateral than the psoas, and the identification of 2 separate tendons should not be mistaken for a tear.
Iliopsoas tendinopathy/tendon tear
Iliopsoas tendon pathology in adults is an uncommonly reported cause of anterior hip pain. Whereas lesser trochanteric apophysitis and apophyseal avulsions are common in active children and adolescents, spontaneous lesser tuberosity avulsions in adults are considered pathologic until proved otherwise ( Fig. 9 ).