TENSION ORBIT AND ITS ACUTE THREAT TO VISION
KEY POINTS
- The potential for developing tension orbit should be recognized and reported verbally.
- The presence of tension orbit on imaging constitutes a medical emergency until proven otherwise and the treatment team so activated.
- Imaging can assess this risk, help in triage, and help in identifying causative pathology and other complications that might further threaten vision or cause additional problems.
Tension orbit is clinical jargon for a situation whereby vision is threatened because of a mass effect in the orbit and resultant stretching of the optic nerve that compromises vision.
This condition is described in this separate chapter because it is common to a number of etiologies that can be broadly placed in the categories of trauma, tumor, infection, and noninfectious inflammation. As such, it is more expeditious to consider its pathophysiology and general imaging findings and clinical implications in one place. These concepts can then be applied to the variety of clinical settings where tension orbit may become important to the treating physicians who are trying to preserve the patient’s vision.
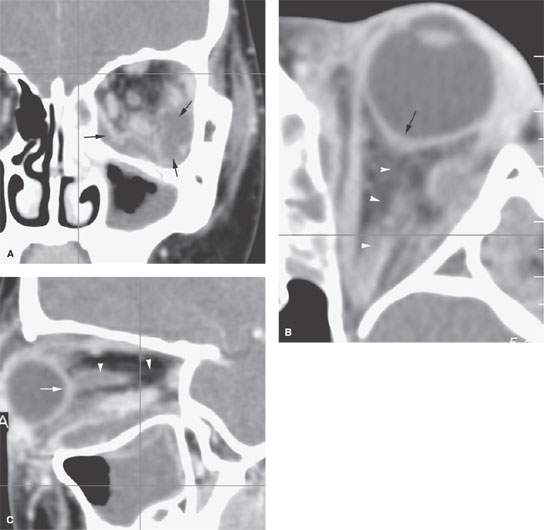
FIGURE 48.1. A patient with orbital abscess secondary to sinusitis. A: Coronal contrast-enhanced computed tomography showing both subperiosteal and intraconal components of the abscess (arrows). B: There is proptosis and early tenting of the eye (arrow), but the optic nerve is not entirely on stretch (arrowheads). C: Sagittal reformation show early tenting of the eye (arrow) and incomplete stretching of the optic nerve and sheath (arrowheads). This case demonstrates early tension orbit; however, a referring service was called emergently with these results. The patient was showing progressive visual loss, and the orbit was emergently decompressed without loss of vision.
PATHOPHYSIOLOGY
Regardless of etiology, the volume of orbital contents increases to a point where there is severe proptosis. The displacement of the eye causes the optic nerve to be stretched. The stretching eventually compromises the vascular supply, leading to ischemic optic neuropathy (Fig. 48.1). In some instances, this occurs in combination with compressive forces at the orbit apex and optic canal as well as a disease process that further compromises the vascular supply.
The presumption in this situation is that these changes are occurring over an acute or subacute time frame. These principles can also be applied in a more chronic setting, and the acuity of medical decision may not be quite as great.
IMAGING FINDINGS AND CORRELATIVE CLINICAL FINDINGS AND IMPLICATIONS
Computed tomography and magnetic resonance imaging show essentially the same anatomic expressions of this condition. These include a procession of changes as outlined below:
- A space-occupying process within the orbit.
- Proptosis.
- Full extension, due to stretching, of the optic nerve/sheath complex so that its entire course from the optic canal to the nerve–globe junction is visible all in one plane of section (Figs. 48.1–48.5).
- The optic nerve sheath complex diameter will diminish due to the stretching effect (Figs. 48.1–48.5). At this point, visual acuity, as well as pupillary response (looking for the development of an afferent pupillary defect), should be monitored at frequent intervals and a team that might be needed to decompress the orbit be made aware of a potential urgent or emergency procedure.

FIGURE 48.2. A patient suffering an orbital floor “blow in” injury. A: Coronal computed tomography (CT) section shows orbital floor injury with upward displacement of the orbital floor typical of this mechanism of injury (arrows) and a circumferential subperiosteal hematoma (arrowheads), both impinging on the normal orbital volume. B: Axial CT section shows moderate tenting of the globe (arrow) and the optic sheath on stretch (arrowheads). This case demonstrates relatively early tension orbit; however, a referring service was called emergently with these results. The patient was showing progressive visual loss (as is not uncommon in this type of orbital injury), and the orbit was emergently decompressed without loss of vision.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree