7 The ankle and foot
Introduction
It is also necessary to appreciate the importance of accurate diagnosis and prompt treatment of conditions in this area; disorders affecting this region, such as Morton’s neuroma or intermetatarsal bursitis, can have a far-reaching effect on the patient due to the disruption of lower kinematic chain mechanics.1,2 Although orthopaedic testing can provide some information as to the range of diagnostic possibilities, further imaging, particularly MR imaging, can often prove key in identifying the pain-producing structure. Although ultrasonography is being increasingly utilized, this modality can be very operator-dependent, which makes it less reliable and prone to producing false negative results.3,4
History and examination
Much of what holds true for the knee also applies to the ankle and foot; this should not be surprising as they are directly connected elements in what, in standing posture, is a closed-loop kinematic chain.2 Because of this, the knee, ankle and foot often need to be assessed as a unit and the reader should direct themselves to Chapter 6 in order to review this material.
Differential diagnosis
The foot is susceptible to many conditions; these can mimic each other and exist as comorbidities. Although a thorough history will help to direct the clinician’s thinking, more than any other joint, the ‘V-I-N-D-I-C-A-T-E’ mnemonic will help to avoid the missed diagnosis (Table 7.01).
Table 7.01 Differential diagnostic considerations for the foot and ankle
| Vascular | Diabetes mellitus, thrombophlebitis, Raynaud’s syndrome |
| Infection/Inflammation | Osteomyeltis/gout, Reiter’s syndrome/ plantar fasciitis, bursitis, tendinitis, cellulitis |
| Neoplasm | Primary or secondary cancers |
| Dermatological | Complex regional pain syndrome (Sudek’s atrophy) |
| Iatrogenic | Drug interactions, postsurgical syndromes |
| Congenital | Morton’s toe, talipes |
| Anatomical | Accessory muscles, Morton’s neuroma, calcaneal spur |
| Trauma | Acute or chronic |
| Endocrine/Environmental | Syndromes related to footwear |
Clinical indications for imaging
The clinical indications for MR imaging of the ankle and foot are varied and may also depend on the clinical protocols established by the imaging centre and the availability of resources. Based on current evidence, MR imaging of the ankle and foot is considered the imaging modality of choice for conditions such as internal derangements (for example, impingement syndromes or tarsal tunnel syndrome) that commonly affect the distal lower extremity or for postoperative evaluation.5–7 MR imaging gives the anatomical detail needed to identify both the pathology and the effect on the surrounding structures; this is important to evaluate since it will affect both the clinical management of the patient and their prognosis.
Procedure and sequences
MR imaging of the ankle requires that the patient lies supine with the ankle perpendicular to the lower leg; however, if the course of a particular tendon requires analysis, the position of the ankle may need to be modified in order to avoid technical artifacts such as the magic angle effect (explained in detail in Chapter 8). A support may be used to immobilize the patient and maintain the position during the imaging study.
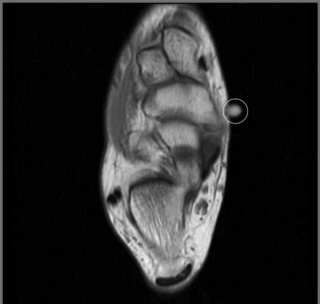
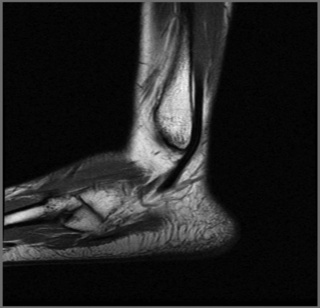
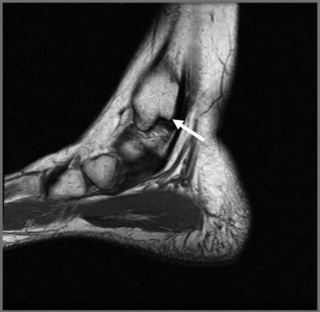
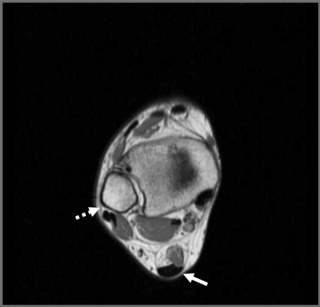
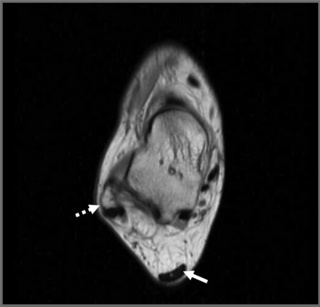
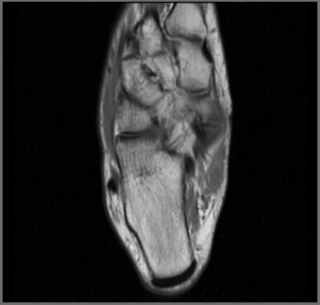
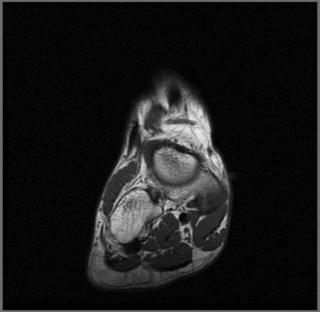
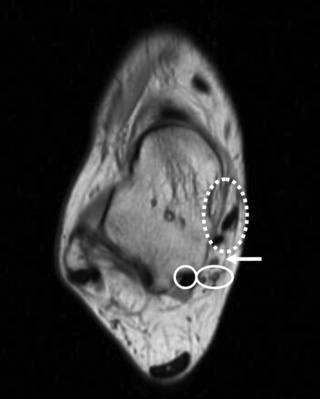
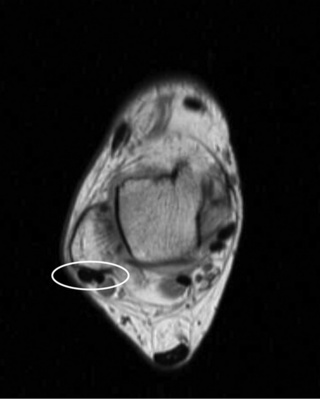
A surface coil is usually used to increase the signal capture; a skin marker may be added to signal to the person reading the image the region of clinical interest (Figure 7.01). The sequences usually consist of all three planes: sagittal (Figures 7.02–7.04), axial (Figures 7.05–7.07) and coronal (Figures 7.08–7.10), using a combination of T1- and T2-weighted (or STIR) sequences, depending on the clinical scenario.
Normal imaging appearance
Tendons
Posterior
The posterior tendons include the Achilles (calcaneal) and plantaris, both of which have associated bursae (Figure 7.11). The Achilles tendon has a broad insertion along the posterior aspect of the calcaneus, which is often irregular in this region due to the development of degenerative changes associated with soliciting the tendon during the activities of daily living. The tendon is best seen on the sagittal and axial cuts. Normally, on the sagittal imaging, it is noted as a long, relatively thick, low signal intensity structure that courses from the intermediate signal of the gastrocnemius muscle to its insertion on the calcaneus. It thickens somewhat just above this insertion; this should not be interpreted as a focal tendinosis. The tendon should be evaluated on both the T1- and T2-weighted images; on both sequences, it should be seen as a low signal intensity structure.
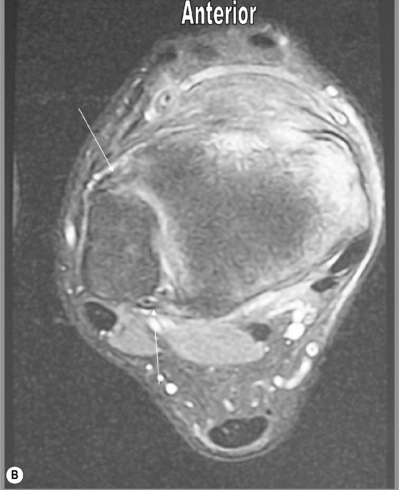
Medial
Medially, the flexor tendons descend under the flexor retinaculum; these comprise the tibialis posterior, flexor digitorum longus and flexor hallucis longus (mnemonically referred to as ‘Tom, Dick and Harry’). The tibialis posterior tendon is prone to rupture, though not as frequently as that of the Achilles tendon.8
As the tendon descends to its insertion on the navicular and metatarsals, the shape of the tendon changes on the axial slices from an oval structure to a flatter configuration as it courses past the medial aspect of the talus. As the tendon continues to descend, it divides into smaller bundles as it approaches the navicular and metatarsals.9 The appearance of this normal fibrous division may be confused with a distal tear; however, tears in the insertions of the tendon are rare and the normal appearance can be confirmed by the lack of high-signal oedema on the fluid-sensitive sequences (Figure 7.12).
The flexor digitorum longus tendon runs alongside and superficial to that of the tibialis posterior. It is rarely injured in isolation and is more commonly associated with a generalized regional tendinopathy. The flexor hallucis longus tendon has a rather unusual course that can render it susceptible to injury. As it passes behind the talus, in those patients who have an os trigonum, friction may be created between the tendon and the accessory ossicle; this can lead to symptoms of posterior impingement, including discomfort and pain on plantar flexion and perhaps focal swelling palpable behind the ankle joint. In the same region, the tendon changes its course from being a predominantly vertical to a more horizontal orientation; during this transition, it can be more prone to injury. The tendon of the flexor hallucis longus is well depicted in its proximal course in both the sagittal and axial planes; as it turns to become more horizontal, it is initially well visualized on the axial and then the sagittal/long axis images as it approaches its insertion.10
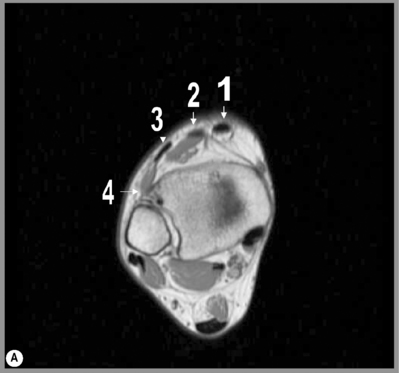
Lateral
The peroneus longus and brevis tendons are located laterally (Figure 7.13). Both these muscles share the action of eversion and dorsiflexion of the foot.11 As both tendons descend, they are located posterolaterally to the lateral malleolus. As the tendons pass this region, they are stabilized in part by the superior peroneal retinaculum, which, depending on the imaging quality, can be identified. At this level, the tendon of the peroneus longus is seen as a rounded structure in the axial plane; this helps distinguish it from the flatter appearance of the peroneus brevis tendon. As it passes further distally, the peroneus brevis is located anterior to the peroneal tubercle of the calcaneus. Both tendons may be surrounded by a thin layer of fluid on the fluid-sensitive sequences, which is normal. Although there is no formal measurement for the quantification of fluid, more than just a thin layer may be considered as tenosynovitis.
Anterior
The tendons in this region comprise the tibialis anterior, which lies most medially, then the extensor hallucis longus, extensor digitorum longus and peroneus tertius (Figure 7.14).12 The tendons pass inferiorly to the superior and inferior divisions of the extensor retinaculum, which may be identifiable on MR imaging. These structures are only occasionally affected by pathology; of the anterior tendons, the tibialis anterior tendon is most frequently involved. In particular, the tibialis anterior tendon course is straight with limited opportunity to be impinged by surrounding structures, unlike the posterior compartment structures. The appearance of the tendon on axial slices is that of a round or oval structure, which, as it approaches the insertion points on the first metatarsal and medial cuneiform, becomes flatter. The normal thickness of the tendon within 3 cm of these insertion points is that of no more than 5 mm.13 Injuries are usually either of a direct nature, which may occur at any age and which may be associated with fractures of soft tissue lesions, or as a result of degenerative processes, in which case the patient is often 60 to 70 years old with chronic symptoms.14