10 The child’s eye
ANATOMY
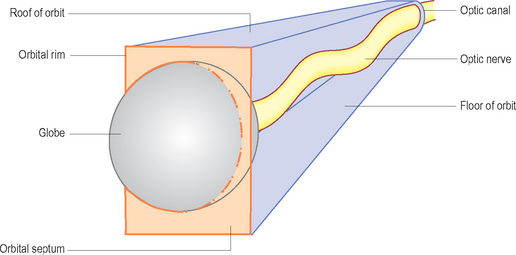
The orbit is the bony part of the skull that houses the globe (Fig. 10.1). This is suspended from the orbital rims by a structure called the orbital septum. The eyelids arise in part from the orbital septum. There are six extraocular muscles which allow movement of the eyeball: four rectus muscles and two oblique muscles. The rectus muscles move the eye up (superior rectus), down (inferior rectus), nasally (medial rectus) and temporally (lateral rectus). The oblique muscles have more complex movements.
The four rectus muscles arise from the optic canal at the apex of the orbit and insert into the anterior portion of the globe; there are intermuscular septa which turn the four muscles with their septa into a cone. A good way to visualize the eye is to think of a cone with a single scoop of ice cream; imagine this lying on its side. The scoop of ice cream is the eyeball and the cone is the complex of four rectus muscles and their intermuscular septa. Now imagine that this cone is lying within a pyramid, also on its side (Fig. 10.2). The pyramid is the bony orbit. The orbital rims are the edges of the base of the pyramid, from which the orbital septum arises, suspending the single scoop of icecream (eyeball). Everything behind the septum is intraorbital and everything anterior to it is extraorbital.
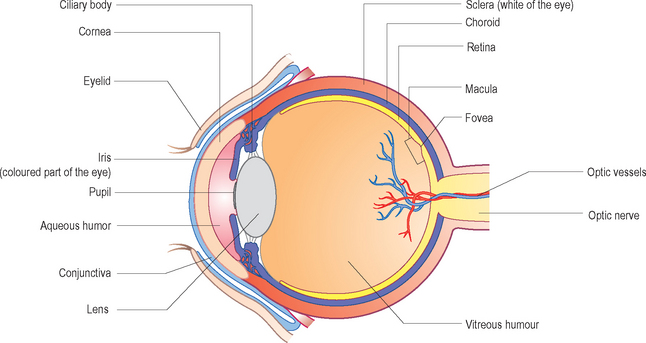
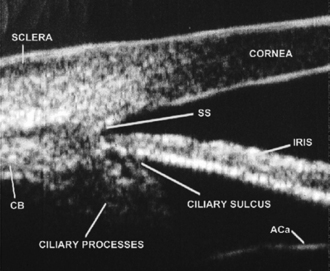
The globe itself is considered by ophthalmologists to have an anterior segment (everything in front of the iris) and a posterior segment (everything behind the lens) (see Fig. 10.1). Ultrasonographically, the anterior segment is best visualized by small-footprint, high-frequency linear transducers (20–50 MHz) and the posterior segment by lower-frequency transducers (5–15 MHz). The anterior segment comprises the cornea, and iris and the anterior chamber which is full of a clear fluid called aqueous. The posterior segment comprises a cavity full of a gel called the vitreous and (from innermost to outermost) the retina, choroid and sclera. The posterior segment is said to have an equator.
ULTRASOUND TECHNIQUE
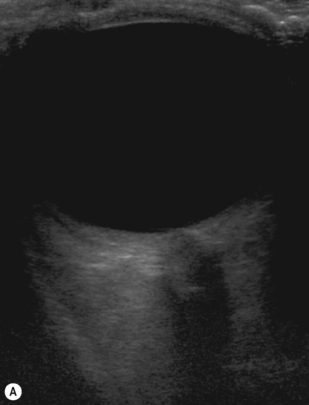
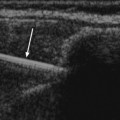
In an ideal world the probe is used in a horizontal plane (with the probe marker by convention, nasal) and then in a vertical plane (with the probe marker, again by convention, superior). The first scan taken should be that of the optic nerve, just to help with orientation (Fig. 10.3). This should be done regardless of the scan plane. Then, if cooperation levels allow, the patient can be asked to look to the right with the probe kept steady. If we were examining the right eye, the temporal retina posterior to the equator would now be scanned. If at the same time as the patient is looking to the right the probe is moved in the opposite direction, the temporal retina anterior to the equator can be examined. By using horizontal and vertical planes, each quadrant of the posterior segment can be seen both anterior and posterior to the equator.
In reality, the child is often reluctant to close his eyes let alone follow precise instructions. This is where the practiced ultrasonographer needs to remember the orientation of the probe while looking at the screen and also glancing occasionally to see where the unexamined eye is looking to understand the direction of the eye being examined. If all else fails, locate the optic nerve to regain your bearings (Box. 10.1).
BOX 10.1 Tips for examining the child’s eye
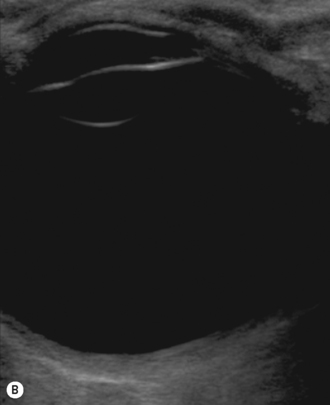
If a lesion in the anterior segment is being examined, it is often necessary to either arrange a high-frequency ultrasound. (Fig. 10.4) or use a water bath (use a rubber glove filled with warm water) to scan (through the closed lids) to help get an idea of what is happening in the anterior chamber. Once the globe has been examined, additional examinations such as Doppler may be performed depending on the clinical question being asked.
COMMON CLINICAL SCENARIOS
• opaque media not allowing adequate examination of the globe
• eyelids will not /can not open
Opaque media
Opaque cornea
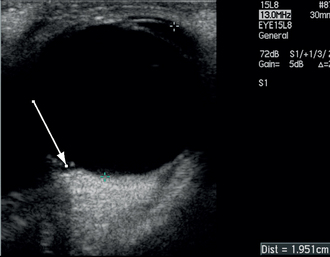
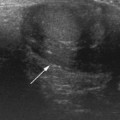
This is usually a rare congenital developmental anomaly. Ultrasound is used in these circumstances to confirm a normal-sized eye. The axial length should measure 16.5 mm at birth, increasing to 23 mm by the age of 13 years with the most rapid growth (3.75 mm) in the first 18 months of life. Children with anterior segment developmental anomalies of the eye can either have small eyes or large eyes secondary to glaucoma, so getting an estimate of the axial length is important (Fig. 10.5). Any anomalies of the retina and vitreous should be noted (see later).
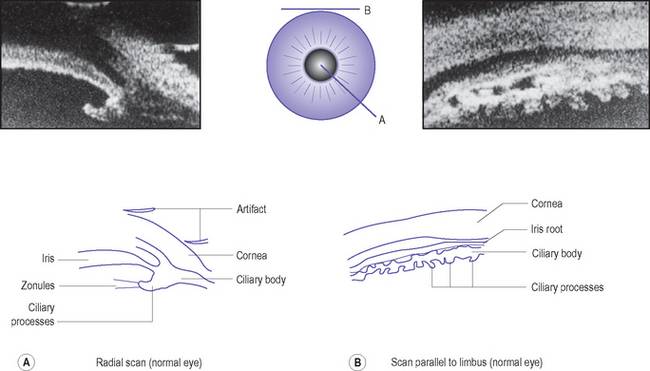
The presence of a cataract should also be noted. In order to get an accurate picture of the anterior segment, high-frequency ultrasound should be used. In infants under the age of 6 weeks this can be done if the child is swaddled and held on a couch. Since this is a contact scan with the eyelids open, it is mostly performed by ophthalmologists. A coupling agent is used (water bath or ocular gel). Most commonly, an examination under anesthetic is required to perform the test. The scanning protocol for this is to scan radial to the limbus or parallel to the limbus, labeling each scan as the clock hour at which it was taken. Axial scans are those taken over the pupillary axis (Fig. 10.6).
Opaque lens
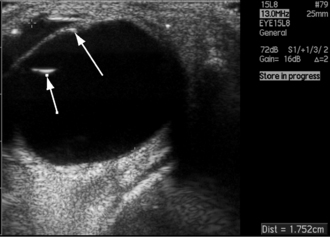
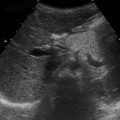
In any case ultrasound will help with the evaluation of the eye. The child may have an anterior capsular cataract; this will normally result in a high echogenicity at the front of the lens with the clear lens proteins being echogenically silent (Fig. 10.7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree