MR imaging has increasingly been used to image joints since its inception. Historically, there has been more emphasis on the evaluation of internal derangement rather than cartilaginous disease. This article reviews cartilaginous diseases of the upper extremity emphasizing those that can be assessed using current clinical MR imaging protocols and addresses the limitations of current imaging techniques in evaluating the articular cartilage of smaller joints. It also provides a brief overview of novel techniques that may be instituted in the future to improve the diagnostic performance of MR imaging in the evaluation of the articular cartilage of the upper extremity.
Cartilaginous injuries and degenerative processes involving the joints afflict millions of individuals each year with enormous socioeconomic ramifications. Although most imaging studies have centered on the evaluation of the articular cartilage of the knee, with the advancement in treatment options, the recent interest in developing disease-modifying drugs, and the necessity to noninvasively monitor the success of treatment, the role of imaging will inevitably continue to expand. Noninvasive methods of acquiring morphologic and physiologic details play an ever-increasing role in the treatment and management of patients with cartilaginous disease. MR imaging, with its excellent tissue contrast, is currently the imaging modality of choice for evaluating articular cartilage. However, imaging of smaller joints, such as those found in the upper extremity, present several challenges secondary to thin overlying cartilage in conjunction with complex surface geometry. Current MR imaging techniques often lack adequate spatial resolution and tissue contrast to appropriately evaluate the articular cartilage of smaller joints. With the introduction of dedicated multichannel extremity coils, higher field strength scanner, and new morphologic and quantitative MR imaging techniques, the future holds promise in overcoming these obstacles.
This article reviews cartilaginous diseases of the upper extremity emphasizing those that can be assessed using current clinical MR imaging protocols and addresses the limitations of current imaging techniques in evaluating the articular cartilage of smaller joints. It also provides a brief overview of novel techniques that may be instituted in the future to improve the diagnostic performance of MR imaging in the evaluation of the articular cartilage of the upper extremity.
Shoulder
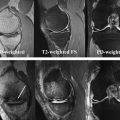
Cartilaginous degeneration within the glenohumeral joint is relatively uncommon, particularly when compared with the weight bearing joints such as the hip or knee. Autopsy studies have shown a relative high frequency of shallow fibrillation involving the glenohumeral joint. However, higher Outerbridge grades II to IV lesions were infrequent in the absence of trauma. The incidence of higher-grade cartilaginous lesions at arthroscopy has been estimated at 5% and supports the autopsy results. Therefore, if a past history of trauma or infection is not elicited and imaging demonstrates more diffuse and severe cartilaginous loss, other causes such as crystalline depositions disorders, inflammatory arthritides, metabolic disorders, synovial osteochondromatosis, and neuropathic osteoarthropathy should be considered in addition to primary osteoarthritis ( Figs. 1 and 2 ). Rapid chondrolysis after arthroscopy has been reported with several plausible causal agents, including the application of thermal or radiofrequency energy typically used for capsulorrhapy, intra-articular administration of gentian violet at the time of arthroscopy, and the use of a continuous bupivacaine pump to aid in the management of postoperative pain.


Cartilaginous Abnormalities and Injury Patterns
Several studies have reported an association between cartilaginous lesions and rotator cuff disease, subacromial impingement, and instability. Peterson found that 75% of shoulders demonstrating cartilaginous disease had concomitant findings of attrition or rupture of the rotator cuff. What remains to be determined is if a true relationship exists or if these are 2 independent processes related to aging. Several theories propose a cascade of events tying the processes together. One possibility is that rupture of the rotator cuff leads to leakage of synovial fluid resulting in loss of the intracapsular pressure and decreased perfusion to the articular cartilage. Instability and superior migration of the humeral head predisposes to altered biomechanics and increased wear of articular surfaces. The mechanical forces and relative lack of nutrition ultimately lead to atrophy of the glenohumeral cartilage, osteoporosis of the subchondral bone plate, and collapse of the humeral head, a phenomenon referred to as cuff tear arthropathy. At arthrography, rotator cuff lesions were identified in more than 90% of shoulders with osteoarthritis of the glenohumeral joint. Gartsman and Taverna, however, reported a much lower prevalence of cartilaginous lesions (13%) in a series of 200 patients with reparable full-thickness rotator cuff tears, with only 5% demonstrating lesions defined as major and involving 150 mm 2 or more of exposed areas of bone.
Patients presenting with clinical findings of subacromial impingement reportedly have a higher prevalence of cartilaginous disease. Guntern and colleagues found a prevalence of 29% for humeral cartilaginous lesions and 15% for glenoid cartilaginous lesions in 52 patients with subacromial impingement syndrome undergoing both MR arthrography and arthroscopy. The investigators stressed the importance of interrogating the cartilage on MR imaging and MR arthrography in this subset of patients because early degenerative joint disease can mimic symptoms of shoulder impingement and can alter the treatment plan.
Trauma and instability often coincide with cartilage injury. Acute dislocations can result in cartilage shear injuries ( Fig. 3 ) and impaction fractures such as a Hill-Sachs lesion, which when large can involve the articular surface of the humeral head. The incidence of cartilage shear injury, osteoarthritis, or Hill-Sachs lesion after an index anterior shoulder dislocation ranges between 24% and 90%. Predictors of osteoarthritis in the setting of instability include time to surgery, age of the patient, presence of a Hill-Sachs lesion or glenoid rim impaction fracture, and presence of a rotator cuff tear.

More focal cartilage injury patterns have also been described. In a small subset of patients developing acute onset of pain after a single traumatic event, focal cartilaginous lesions were identified along the posterosuperior aspect of the humeral head medial to the typical location of a Hill-Sachs lesion. Although all patients had additional pathologic condition involving the shoulder on MR imaging, those undergoing arthroscopy required debridement with good short-term outcomes in individuals with smaller cartilaginous lesions. This cartilaginous injury pattern differs in location and clinical history from the injury pattern near the insertion of the supraspinatus tendon described by Paley and colleagues in 41 symptomatic overhand-throwing professional athletes. The injury pattern occurred in 17% of subjects and typically consisted of Outerbridge grade II or III cartilaginous lesions less than 1 cm in maximal diameter. The cartilaginous lesions were associated with other signs of posterior impingement such as undersurface fraying of the rotator cuff or fraying of the posterosuperior labrum.
Although rare, osteochondral lesions do occur in the glenoid fossa, with the most common imaging features demonstrating either a multiloculated cyst in the subchondral bone plate or a single osteochondral fragment ( Figs. 4 and 5 ). Patients typically relay a history of trauma, and a strong association with instability, capsular redundancy, labral injuries, and intra-articular loose bodies have been reported. These osteochondral lesions should be differentiated from more common cartilaginous injuries to the glenoid referred to as Bankart lesions. Bankart lesions are the direct result of an anterior dislocation leading to impaction of the humeral head into the anteroinferior glenoid rim. This lesion results in a spectrum of injuries to the glenoid fossa from isolated tears of the anteroinferior labrum to labral injuries with concomitant involvement of the subjacent cartilage or cartilage and bone (osseous Bankart lesion). Trauma secondary to forced adduction of the humeral head against the glenoid cavity with the arm in abduction and external rotation may result in a superficial tear of the anteroinferior labrum with involvement of the subjacent glenoid cartilage ( Fig. 6 ), otherwise known as a glenolabral articular disruption (GLAD). In contradistinction to a Bankart or Bankart variant lesion, the GLAD lesion described by Neviaser maintains the integrity of the inferior glenohumeral ligament and is not associated with glenohumeral instability on physical examination or history of dislocation. A less-common injury typically involving the posterior glenoid rim is the glenoid articular rim divot. The cause of this lesion is unknown. However, axial compression has been theorized, with the injury occurring at developmentally weak spots along the fusion sites of the multiple ossification centers of the glenoid.