Chapter 1
The Diagnostic Approach to Malignant Type Calcifications on the Mammogram
The first step in analyzing the calcifications is to determine their site of origin:
- Within the ducts: Casting type and secretory disease type calcifications, the subject of the previous volume in this series.1
- Within the terminal ductal lobular units (TDLUs):
- – Crushed stone-like calcifications: the subject of this volume.
- – Powdery/cotton ball-like calcifications: the subject of the next volume in this series.
- – Crushed stone-like calcifications: the subject of this volume.
- Outside the glandular tissue (miscellaneous types): calcifications in the walls of blood vessels, in sebaceous glands in the skin, or in sclerotic stroma are usually characteristic for benign processes and seldom cause differential diagnostic problems.
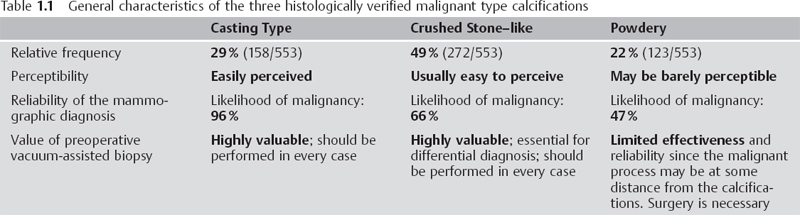
Each of the three groups of malignant type calcifications— the casting type, the crushed stone—like and the powdery—has its own unique characteristics from the viewpoint of histology, imaging (see Table 1. 1), and outcome.
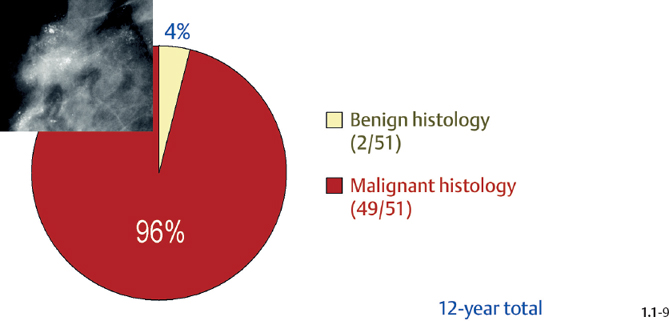
(A) Casting type calcifications are easy to perceive and diagnose radiologically and histologically, but there is a considerable discrepancy between their tumor characteristics and their surprisingly poor outcome.1 The underlying malignant process is often diagnosed as in situ carcinoma or as Grade 3 in situ carcinoma occurring over a large area associated with microinvasion and/or small (1-9 mm, 10-14 mm) invasive tumor foci, but the outcome may correspond to that of an advanced carcinoma. This important breast cancer subgroup requires a concerted interdisciplinary effort if we are to succeed in improving the currently poor prognosis of patients presenting with extensive casting type calcifications on the mammogram.
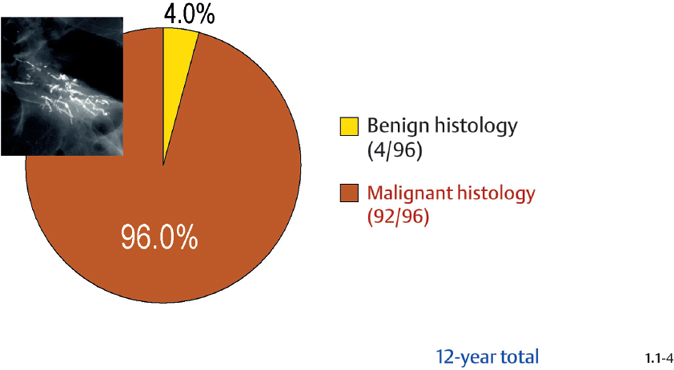
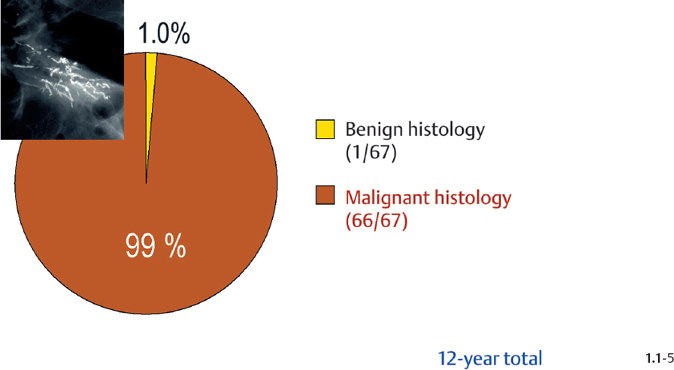
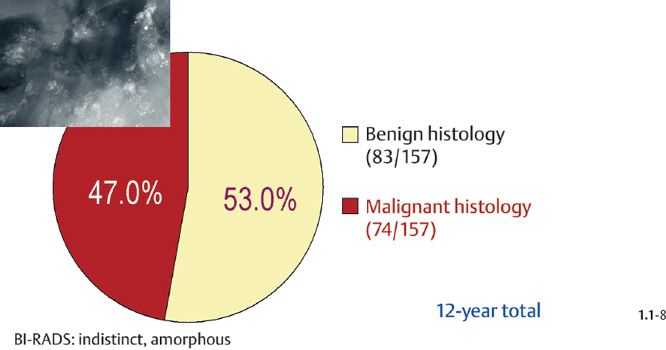
(B) At the other extreme, powdery calcifications may be barely perceptible on the mammogram. Unlike the casting type calcifications that represent a clearly defined disease subgroup, powdery calcifications-corresponding to psam-moma body type calcifications on histology-may represent a number of benign breast lesions (sclerosing adenosis with or without atypia, blunt duct adenosis, lactational change) in addition to Grade 1 in situ carcinoma. The mammographic appearance of these different diseases may be identical, making a definitive radiological diagnosis impossible. While surgical excision of casting type calcifications will result in a malignant histological diagnosis in more than 95% of the cases, even if there is no associated tumor mass (Figs. 1.1-4 & 5), the corresponding figure is about 50% when only powdery calcifications are seen on the mammogram (Figs. 1.1-8). Also, preoperative vacuum-assisted biopsy is strongly recommended in cases with casting type calcifications, since the malignant cells and their product, the amorphous calcifications, are in close proximity. In powdery calcification cases, the psammoma body like calcifications may be located in a benign process, at a site remote from an incidental malignant process, or they may be associated with the Grade 1 in situ carcinoma itself. For this reason, the effectiveness and reliability of preoperative vacuum-assisted biopsy is limited. Excisional biopsy is the method of choice for the definitive diagnosis of powdery calcifications.
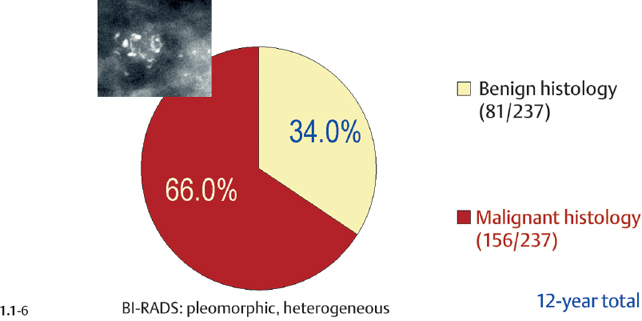
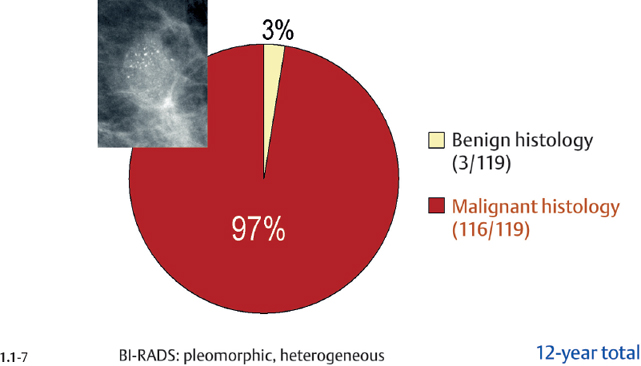
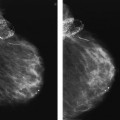
(C) Crushed stone-like calcifications are those most frequently encountered in mammography screening and also require the most extensive preoperative work-up. This is because their benign differential diagnostic counterparts-fibrocystic change, fibroadenoma, and papillomaare far more frequent than breast cancer and can be managed satisfactorily with the use of large-bore percutaneous needle biopsy procedures. The differential diagnosis is a challenge, because Grade 2 in situ carcinoma, fibrocystic change, and fibroadenoma all originate from the TDLU. Therefore, when both the malignant and benign processes have associated crushed stone-like calcifications, the result will be a cluster or multiple clusters of similar calcifications. Subgross, 3D histology is of considerable help for understanding the underlying pathophysiological processes producing these diseases and learning the capabilities and limitations of radiological differential diagnosis.
Overview of the Diagnostic and Management Problems Encountered When Malignant Type Calcifications Are Detected on the Mammogram
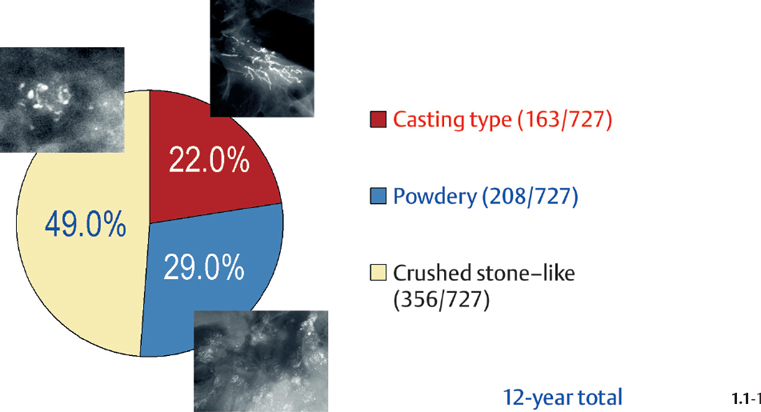
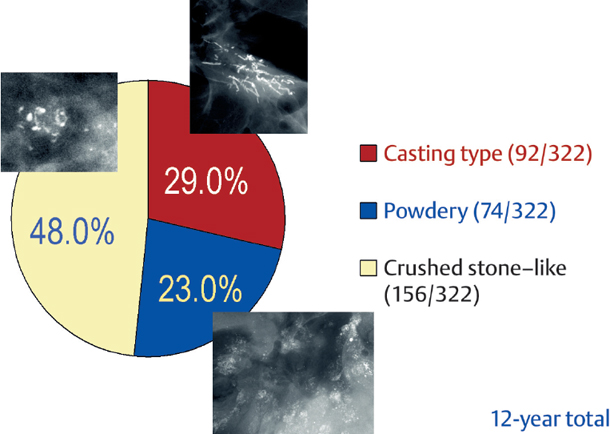
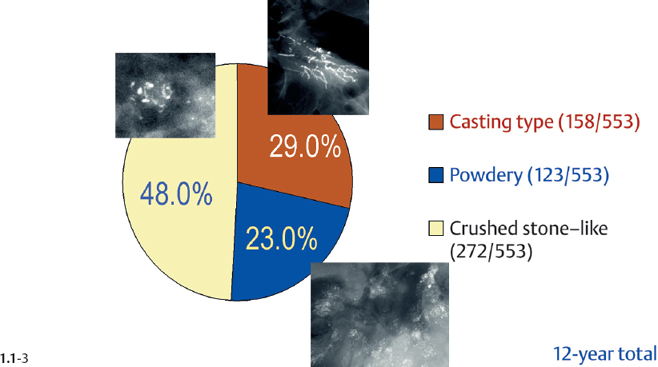
The relative frequencies of the casting type, crushed stone-like and powdery calcifications in malignant and benign breast diseases, with and without an associated tumor mass, are given in the following pie charts. The data originate from a prospective, consecutive series of patients referred to open surgical biopsy during a 12-year period at the Department of Mammography, Falun Central Hospital, Sweden.
Crushed stone-like calcifications account for about half of all calcification cases referred to open surgical biopsy, regardless of whether we consider the malignant type calcifications alone or in combination with the histologically verified benign cases (Figs. 1.1-1 & 3). The relative frequency of the three types of histologically proven malignant type calcifications remains virtually unchanged regardless of whether they are associated with a tumor mass or not (Figs. 1.1-2 & 3). The value of casting type calcifications in predicting malignancy is 96% without and 99% with an associated tumor mass (Figs. 1.1-4 & 5). This is not the case with crushed stone-like or powdery calcifications. As Figs. 1.1-4 to 9 demonstrate, crushed stone-like and powdery calcifications are less predictive of malignancy without an associated tumor mass. This uncertainty may cause considerable differential diagnostic problems.
Relative Frequency of Calcification Occurrence
Distribution of All Histologically Verified Malignant Type Calcifications
Malignancy Ratio of Casting Type Calcification Cases
Malignancy Ratio of Crushed Stone-like / Pleomorphic Calcification Cases
Malignancy Ratio of Powdery Calcification Cases
Crushed Stone-like and Powdery / Cotton Ball-like Calcifications on the Mammogram
The TDLU (Figs. 1.2-1 to 4) is the origin of many heterogeneous pathological processes, including in situ carcinoma of different grades. However, most abnormalities arising within the TDLUs are benign hyperplastic breast changes. These diseases may produce proliferating cells and/or an excessive amount of fluid, either of which will distend and distort the TDLUs by increasing the intraluminal pressure. In either case calcifications may be produced within and confined to preexisting TDLUs and may be detectable on the mammogram as single or multiple clusters. These resulting calcifications can be classified into two different categories:
- The individual calcifications are discernible, resembling crushed stones (Figs. 1.3-1 & 2

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree