9 The elbow
Introduction
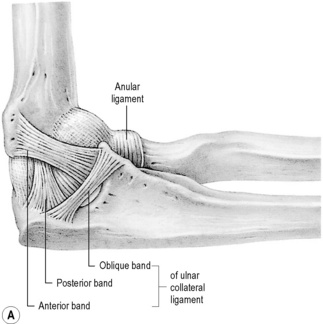
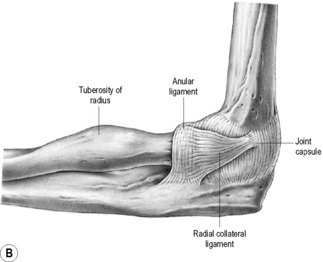
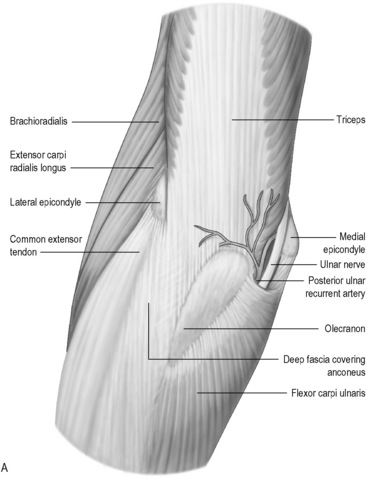
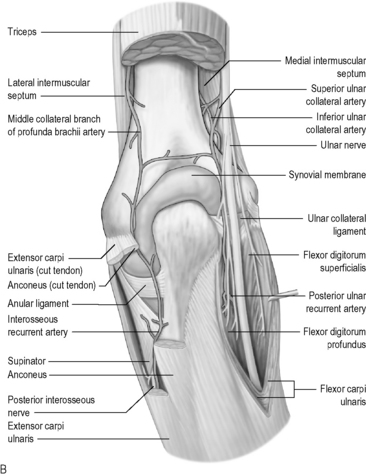
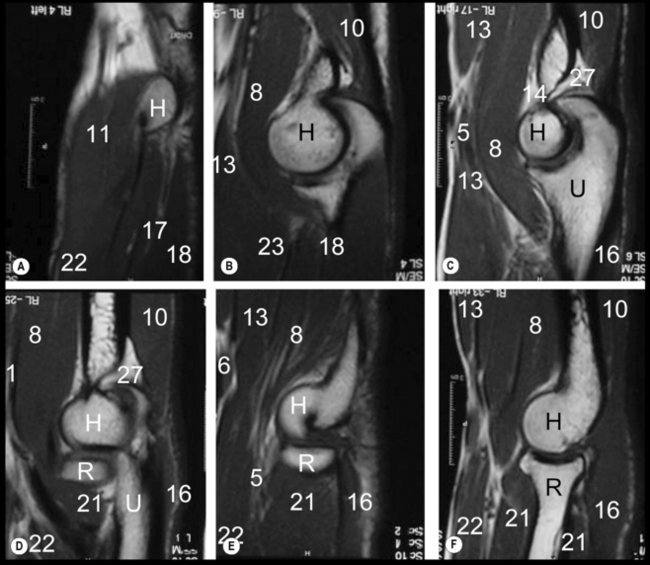
The elbow is a complex articulation in both structure and function1 and this demands from the clinician a detailed knowledge of the normal anatomical relationships, whether treating clinically or interpreting diagnostic imaging. It is worth reviewing these before proceeding further; this can be done by studying Figures 9.01 and 9.02.
However, diagnosis of elbow conditions does not begin with MR imaging. As with any other area of the body, an appropriate history and physical examination cannot be replaced by any diagnostic imaging modality. Not only do these establish a differential diagnosis that determines the necessity for and type of imaging required, but also it allows for clinical correlation of any pertinent findings.2
History and examination
Whenever the clinician is assessing a patient presenting with pain in or around the elbow, their evaluation should include the whole of the associated kinematic chain: hand, forearm, arm, shoulder and cervicothoracic spine. The contralateral elbow should also be considered for both comparison and evidence of compensation, which as well as indicating the level of disability can also determine the onset of adaptive injury.3
When taking the patient’s history, in addition to the customary questions, there are some key points that will help direct the physician to the most appropriate differential diagnoses. These are detailed in Box 9.01.
Box 9.01 Historical considerations for a patient presenting with elbow pain
Differential diagnosis
Mentally dividing the elbow into four regions is a valuable exercise, and assists both in constructing an initial differential diagnosis and in determining the imaging appearance. Each of the quadrants can be associated with specific pain-generators, pathologies and, to a certain extent, mechanisms of injury (Table 9.01); of course, disorders such as loose body formation or significant trauma may cause pain in any location.
Table 9.01 Structures and pathologies associated with different quadrants of the elbow
| Structures | Pathologies |
|---|---|
| Lateral quadrant | |
| Medial quadrant | |
| Anterior quadrant | |
| Posterior quadrant | |
Correlating the localization of the pain to the timing of the complaint may help to further refine the diagnostic list. For example, pain at the anterior aspect of the elbow during the early cocking phase of a throw may be consistent with biceps tendonitis.4,5 Likewise, a tendinopathy involving the flexors and pronator teres will most likely manifest as anterior-medial pain during the late acceleration phase of a throw where forearm pronation and wrist flexion are maximal.6
These examples are specific to sports such as baseball, rounders or cricket, which involve throwing. The structures of the elbow are also specifically solicited during sports such as tennis,7–12 badminton,12–14 golf,12,15–18 squash/racquetball12,19,20 and basketball.21,22 Occupational injuries at the elbow are also frequent: ask any construction worker, musician or computer enthusiast!23–28 In addition, the forearm also becomes very active in compensation for shoulder or core deficiencies.15,29,30
Clinical indications for diagnostic imaging
The initial imaging modality for the elbow remains plain film radiography: it is useful, widely available and inexpensive. Many projections are available and demonstrate the osseous anatomy well. The standard examination protocol involves an anteroposterior (AP) view with the forearm in supination and a lateral view, taken with the elbow in 90° of flexion and the forearm in neutral (i.e. without pronation or supination).31,32 A medial oblique view with the forearm in pronation is the most common supplementary view. Depending on the clinical question, projections specifically designed for the olecranon and the radial head are also commonly taken and can be very useful.31,32
Ultrasonographic evaluation of the elbow is becoming more and more popular. There is minimal bony interference in the elbow area, allowing for a good acoustic window. The tissues evaluated are also relatively superficial.33,34 Ultrasound examination can also be performed in real time and in a dynamic fashion with immediate patient feedback and localization of the region of complaint.35 The evaluation of the ulnar nerve in a patient with cubital tunnel syndrome, chronic epicondylitis or bursitis may be much more convenient and cost-effective with this modality than with MR imaging.36–42
Ultrasonography is also quite popular for the evaluation of the paediatric patient, since the use of MR imaging in young children can be quite problematic. In order to ensure compliance and decrease motion artifacts, it is often necessary to sedate children for the relatively lengthy MR image acquisition time. This process increases the invasiveness of the MR technique, and is why ultrasonography may be preferentially chosen as the imaging modality of choice in the paediatric population.43,44
Although radiographs and ultrasound may be used to determine the source of pain and functional deficit, MR imaging remains unsurpassable for many conditions because of the high soft tissue detail and bone marrow information it provides; however, this information may not always be necessary – many elbow conditions may be diagnosed clinically without any imaging and treated conservatively with great success. Approximately 90% of patients with an epicondylitis recover well without surgery.45 MR imaging or ultrasonography may only be appropriate for the remaining patients that do not respond to conservative care.46
Trauma
Trauma often necessitates MR imaging of the elbow in both the acute setting as well as the chronic situation such as the repetitive stresses experienced in sports activities, especially those involving a racquet.46,47 Chronic trauma may also arise from a complication of an acute incident where the patient continues to be affected by symptoms long after the precipitating event. Patients with persistent elbow symptoms related to sports may develop scar tissue, tendinous degeneration, partial or complete tears of the tendons, or articular changes, all of which can preclude a rapid or complete recovery.19,46
Those patients suffering from persistent elbow symptoms may be harbouring complications such as avascular necrosis or loose body formation resulting from an osteochondral injury. In such cases, MR imaging can determine the most appropriate clinical management of the patient, providing a wealth of information as to the size and position of the lesion and any associated fragment.48–51
In the acute trauma setting, there are also situations that may require planar imaging such as MR; in particular, dislocations and complex fractures. Patients sustaining posterior dislocations of the elbow are at risk of associated ligament and capsular tears, avulsion fractures and instability. In the case of fractures, MR imaging is not always needed for purposes of identification, but can be vital in determining the management and prognosis.52 When a simple radial head fracture is identified on plain film, the treatment plan is usually straightforward: initial immobilization and early rehabilitation to avoid capsular restriction, particularly into extension. No advanced imaging is normally performed; however, the management and prognosis of comminuted fractures is often based on the associated injuries as opposed to the fracture itself. In these instances, cross-sectional imaging becomes indicated.
MR imaging of the elbow may also provide important information regarding the neural elements that pass by the articulation during their course into the forearm and hand. The radial, median and ulnar nerves follow complicated pathways and are prone to entrapment in multiple locations by a wide variety of causes such as injury, mass compression or developmental variants.53–56 Surgery may also provoke scar tissue formation about the nerves, leading to adhesions, irritation, entrapment and, eventually, chronic denervation.57,58 In such syndromes, the use of MR imaging can be useful in determining the extent of any neuropathy and associated denervation and evaluating the potential for recovery. Clinical examination, electromyography and nerve conduction tests are also essential parts of the work-up, allowing for both the structure and function of the involved neural structures.
Techniques and protocols
Imaging of the elbow has benefited greatly from technological developments; in particular, high field strength magnets (1–3 T) and better surface coils have improved the speed and quality of the images.59 MR imaging of the elbow involves the patient lying in the supine position with the arm resting against the body. A surface coil, wrapped around the patient’s elbow, is used to improve the final image quality. With the patient in this position, motion artifacts are minimized.60
If there is clinical suspicion of a lesion to the distal biceps tendon or median nerve, the ‘FABS’ position (flexed elbow, abducted shoulder, supinated forearm) may be utilized to obtain a longitudinal view of the tendon and nerve. In this instance, the patient lies prone on the MR table with the involved arm overhead, the elbow flexed to 90° and the forearm supinated with the thumb pointing upwards. MR imaging can also be performed on a patient wearing a cast but, since the arm is sometimes fixated in an odd flexion position, it may cause difficulties in patient positioning. The cast also adds bulk, making the use of a standard elbow coil difficult.61
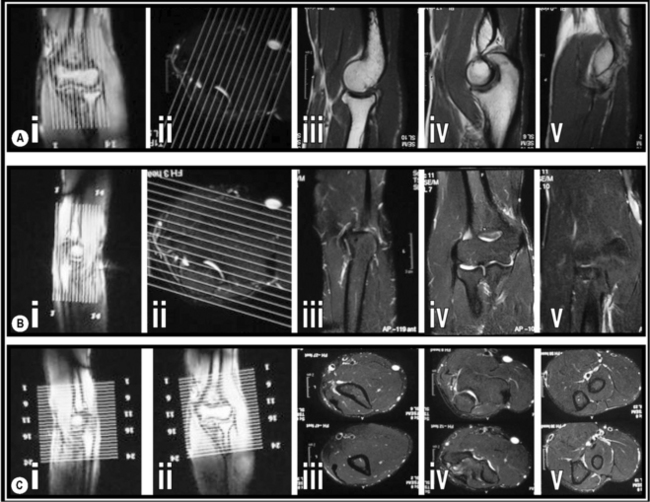
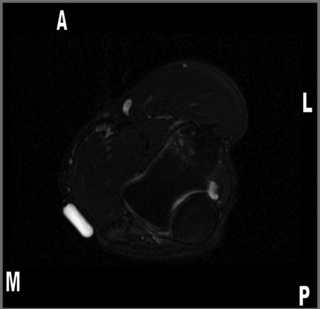
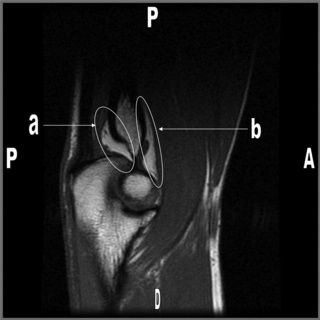
When possible, the three planes of interest are all included: axial, sagittal and coronal, maximizing the three-dimensional visualization of anatomical structures. The images are usually obtained with 4-mm slices and a 10% (0.4-mm) gap to prevent cross-talk (Figure 9.03). Since not all the aforementioned sequences are necessarily performed on a routine scan, it is always helpful to provide the radiographer and radiologist with the clinical findings and diagnostic suspicions, so that the appropriate parameters can be applied.62 Another useful trick that may be utilized when looking for a specific problem is to tape a capsule of vitamin E on the skin of the patient, adjacent to the area of complaint. This will serve as a marker to indicate the problematic region on the images and can be seen on the final image as a round, or oval, area of high signal focus lying on the patient’s skin (Figure 9.04).63
On occasion, intravenous contrast may be added, particularly if the clinical question involves the identification of a mass or the evaluation of an active, synovial-based disorder. MR arthrography is limited to assessing undersurface collateral tears or finding intra-articular loose fragments. The use of contrast carries risks and increases the invasiveness of the technique. The decision as to whether contrast is appropriate and, indeed, the most appropriate investigative protocol is based largely on the nature of the structure(s) under investigation (Table 9.02).64,65
Table 9.02 Optimum sequences for the visualization of different structures
| Bone and marrow | STIR in all three planes |
| Articular cartilage | STIR and gradient echo, Proton Density Fat Saturated coronal/sagittal planes |
| Ligaments | STIR in the coronal plane |
| Tendons | T1-weighted and STIR in all planes |
| Nerves | T1-weighted and STIR in the axial plane |
Normal imaging anatomy
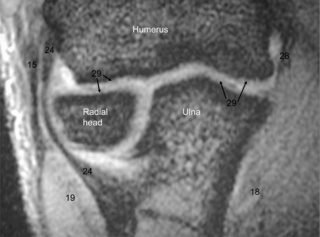
Osseous anatomy (Figures 9.05–9.07, Box 9.02)
The elbow is a compound, hinge-type synovial joint (ginglymus) composed of the distal humerus, proximal ulna and proximal radius (Figures 9.01, 9.02).66
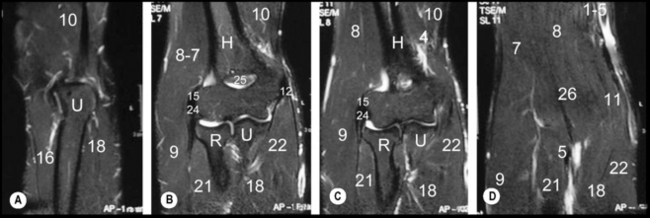
On the distal humerus, there are two prominent processes, the medial and lateral epicondyles. The distal articular surface of the humerus is wide and flat. The lateral third, the capitellum, articulates with the head of the radius, which has a disc-shaped articular surface. The medial third, the trochlea, articulates with the trochlear notch of the ulna.67
This notch, which is large and C-shaped, is also sometimes termed the semilunar notch. The projection forming its upper border is called the olecranon process. It articulates with the posteriorly situated olecranon fossa of the humerus and may be palpated as the angular ‘point’ of the elbow. The projection that forms the inferior border of the trochlear notch, the coronoid process, enters the coronoid fossa of the humerus when the elbow is flexed. This fossa is separated from the cubital fossa anteriorly by only a thin layer of bone.68
The lateral side of the coronoid process has a small, shallow notch or groove, called the radial notch. This articulates with the head of the radius, forming a synovial pivot (trochoid) joint, which allows supination and pronation of the forearm.69 On the medial aspect of the coronoid process, approximately 2 cm posterior to the coronoid tip, is the sublime tubercle, the site of insertion for the ulnar collateral ligament.70
Nerves
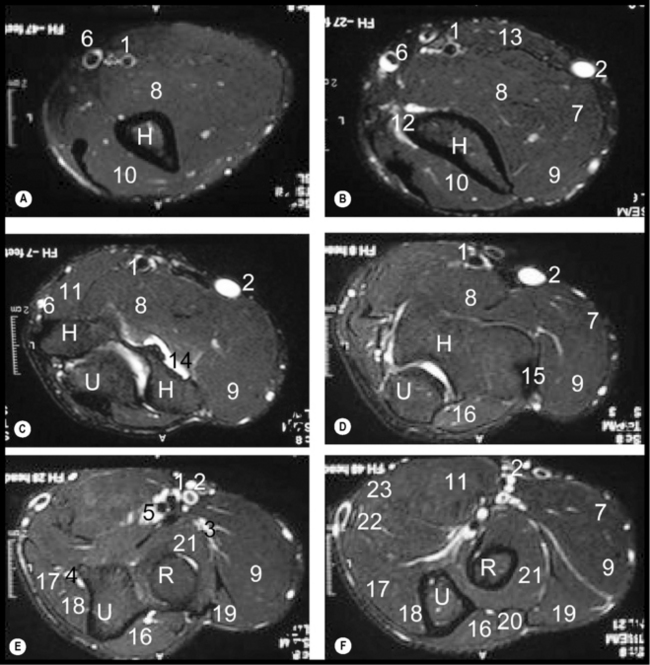
Nerves are distinguishable on MR imaging owing to their surrounding layer of fatty myelin. The median, radial and ulnar nerves are usually obvious on axial images of the elbow (Figure 9.05E); however, they can be difficult to identify owing to their size, variable anatomical relationships and low signal intensity. They have complex courses, running through multiple compartments.
Ulnar nerve
Of the three, the ulnar nerve is the most vulnerable to injury, probably because of the superficial position that the nerve takes as it passes through the joint. The elbow is also the most common site for traumatic injury to the ulnar nerve, particularly where it passes through the cubital tunnel.53,69 The tunnel floor is made from the posterior and transverse portion of the ulnar collateral ligament (or medial collateral ligament of the elbow) as well as the articular capsule. The aponeurosis of the flexor carpi ulnaris muscle and the cubital tunnel retinaculum create the roof of the tunnel. This retinaculum, sometimes called the arcuate ligament, runs from the olecranon to the medial epicondyle and is not present in everyone.1 In some individuals, it is replaced by an accessory muscle, the anconeus epitrochlearis, which offers an additional site of potential entrapment and compression of the ulnar nerve.71,72
Median nerve
The median nerve may be better identified if the patient’s forearm is placed in pronation during imaging.73 If there is a clinical question regarding this nerve, it is thus wise to impart this information to the radiologist.
In the region of the elbow, the median nerve travels between the bicipital aponeurosis and the brachialis muscle, through the cubital fossa. The median nerve gives off its anterior interosseous branch just after passing between the two origins of the pronator teres muscle, as they arise from the medial epicondyle and coronoid process, offering a potential site of entrapment. If this pathology occurs before the separation of the nerve into its distal branches, it is termed pronator syndrome. If the entrapment occurs after the separation, it is referred to as anterior interosseous nerve syndrome.69,74,75
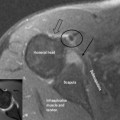
Radial nerve
The radial nerve can be found in the anterolateral portion of the elbow region, between the brachialis and brachioradialis muscles. It divides into two branches: the superficial sensory branch passes between the supinator and brachioradialis muscles, maintaining the title of the radial nerve, while the purely motor posterior interosseous nerve forms at the level of the capitellum and courses between the heads of the supinator muscle, in a fibrous tunnel named the arcade of Frohse.66,69,75
Muscles and bursae
Anterior
The group of muscles that contribute to the soft tissue structures anteriorly comprise the biceps brachii and brachialis. The two proximal heads of the biceps brachii unite to form a common tendon above the elbow that inserts on the radial tuberosity. The tendon anchors into the bicipital aponeurosis (or lacertus fibrosus). The brachialis muscle lies deep to the biceps brachii. It originates from the distal half of the anterior humerus and inserts onto the coronoid process.66,68 Both muscles are best seen on axial and sagittal images (Figures 9.05 and 9.07 respectively).
The bicipitoradial and interosseous bursae separate the extrasynovial, paratenon-wrapped distal tendon of the biceps from the anterior aspect of the radial tuberosity.68 The bursae are not normally visible on MR images, unless they have become inflamed and/or distended.
Posterior
The muscles contributing to the posterior elbow group are the anconeus and triceps muscles.76 The axial and sagittal sequences are the most useful to assess both these muscles (Figures 9.05 and 9.07 respectively). The anconeus is a small, triangular muscle that originates on the posterior aspect of the lateral epicondyle and inserts on the posterior superior surface of the ulna.76 Although it assists the (postero-) lateral ulnar collateral ligament (LUCL) in resisting varus stress, since it blends with the triceps distally, it is often considered as functionally part of this muscle.68 The triceps attaches to the posterior surface of the olecranon process and it is at this site that the tendon’s fibres become intertwined with fibrofatty slips that may be radiologically mistaken for a partial tear. This phenomenon will appear as an increased signal on both T1- and T2-weighted images. The olecranon bursa lies between the triceps tendon and the olecranon.69
Medial
The medial group of muscles consists of the pronator teres, the palmaris longus (when present) and the flexors of the hand (flexor digitorum superficialis and profundus; flexor carpi radialis, flexor carpi ulnaris and flexor pollicus longus).1 The pronator teres muscle is the most superficial of the group. It has two origins: from the medial condyle (the humeral head) and from the coronoid process of the ulna (the ulnar head). The pronator inserts onto the lateral surface of the mid-third of the radius. The remaining muscles unite in the common flexor tendon, which inserts into the medial epicondyle of the humerus.76 The ulnar (or medial) collateral ligament may also be identifiable along its course. It offers supports to the common flexor tendon in resisting valgus stresses. For best visualization, one should assess the axial and coronal images (Figures 9.05 and 9.06 respectively). Normal ligaments and tendons will be demonstrated as homogeneously low signal structures inserting onto the medial epicondyle.77
Lateral
The supinator and brachioradialis muscles, along with the extensor muscles of the hand, form the lateral group of elbow muscles.1 The supinator muscle is the deepest muscle, originating on the lateral epicondyle of the humerus and inserting onto the proximal third of the radius. It contributes to the floor of the cubital fossa whilst the brachioradialis serves as the lateral boundary of the cubital fossa.68 Originating at the supracondylar ridge of the humerus, the brachioradialis inserts onto the lateral surface of the distal radius.76 The extensor muscle group originates as the common extensor tendon from the lateral epicondyle. The tendon is common to extensor carpi radialis brevis and carpi ulnaris and to extensor digitorum and digiti minimi. The extensor carpi radialis longus is part of the lateral group but originates slightly more proximally on the lateral condyle of the humerus.69 The axial and coronal images are again the best to visualize the lateral compartment muscles (Figures 9.05 and 9.06 respectively).
Ligaments and capsule
The articular capsule of the elbow extends from the humerus, covering all the articular surfaces down to the radial neck and inferior aspect of the coronoid process of the ulna. It is weaker on its anterior and posterior aspects, the medial and lateral aspects being strengthened by the medial and lateral collateral ligament complexes.68 The anterior and posterior fat pads may be seen on lateral radiographs of the elbow joint as well as on MR imaging. Normally, with the elbow in a flexed position, the anterior fat pad is visible on radiographs as a relatively linear lucency in contact with the anterior aspect of the distal humerus. The posterior fat pad is not normally visible as it is hidden deep within the olecranon fossa. Articular oedema from effusion, haemarthrosis or synovitis will cause these fat pads to be displaced away from the humerus, resulting in radiographic visualization of the posterior fat pad and anterosuperior elevation of the anterior fat pad which adopts a curvilinear configuration.78 The fat pads are visible on MR imaging, particularly on T1-weighted or fat-sensitive sagittal sequences (Figure 9.08).
The ulnar collateral ligament (UCL) complex contributes to medial elbow stability (Figure 9.01A). It comprises three distinct bundles: the anterior, posterior and transverse portions.69 The anterior bundle extends from the medial epicondyle to the coronoid process and is best seen on coronal images (Figure 9.09).65,68 Its proximal aspect is flared and tapers distally; it is the principal restraint against valgus stress.79,80 The posterior fibres extend from the medial epicondyle to the olecranon. The transverse (or oblique) portion extends from the olecranon to the coronoid process and does not really contribute to stability of the joint. The posterior and transverse portions are not always present, but this is rarely an issue from a biomechanical or clinical standpoint.68 They are difficult to see on MR images; however, their presence is inferred as they form the floor of the cubital tunnel.81
The radial collateral ligament complex includes the lateral collateral ligament (LCL), the annular and accessory collateral ligaments and the LUCL (Figure 9.01B).68 It contributes to the lateral stability of the elbow and resists varus stress.82,83
The LCL extends from the anterior aspect of the lateral epicondyle and inserts into the annular ligament and supinator fascia. The posterior bundle, the LUCL, extends from the lateral epicondyle and inserts into the ulna (hence the name) at the crista supinatoris.68 The LUCL is the prime restraint against varus stress and its disruption will severely diminish the stability, leading to posterolateral rotatory instability of the elbow.83,84 This ligament is best seen on coronal images. The better-known annular ligament is the prime stabilizer for the proximal radioulnar joint69 and is best assessed on axial slices (Figure 9.05).65
Normal variants and diagnostic pitfalls
Osseous variants
Most commonly asymptomatic, the supracondylar spur (or process) and its associated ligament are found in approximately 1% of the population. The spur, which is located on the anteromedial surface of the humerus, 5–6 cm above the epicondyle, can be rudimentary and tubercle-like or quite large.85 The ligament of Struthers connects the bony outgrowth to the medial epicondyle, forming the supracondylar foramen or arcade of Struthers. The median nerve and branches of the brachial artery run through the foramen (Figure 9.10). In some cases, the arcade can be the site of an anomalous origin of the pronator teres muscle.86–88 These close anatomical relationships can account for the symptoms that may be experienced by some patients and will be addressed along with the other causes of median nerve entrapment.
This variant is easy to visualize on plain film radiographs, especially if the arm is in a slightly oblique position. The spur will point towards the elbow joint, as opposed to its principal differential diagnosis, the osteochondroma, which points away from the joint. Although location and appearance are key to distinguishing the two, MR imaging demonstrates the cartilaginous cap in a developing osteochondroma.86
Two accessory ossicles are known to occur about the elbow joint: the os supratrochleare and the patella cubiti. The os supratrochleare is a developmental ossicle believed to originate from an accessory ossification centre of the olecranon. When present, it is located within the joint capsule in the olecranon fossa. It may restrict extension or can be asymptomatic. Because of its intra-articular position, it may benefit from synovial nutrition and increase in size. Its shape may be altered by the battering received from the adjacent olecranon. It is most common in the dominant arm of males.89,90
The patella cubiti is a rare sesamoid bone found in the tendon of the triceps, mimicking the patella in the quadriceps tendon. It may also be asymptomatic or cause restriction in the extension range of motion.91