The first question that a radiologist should consider when interpreting any study is, “Is this an adequate study?” That topic encompasses many points in breast imaging:
- •
Is this the correct patient?
- •
Is this the correct study for this patient?
- •
Is the positioning adequate?
- •
Are any images blurry?
- •
Do the images have any correctable artifacts?
Correct Patient/Correct Study
A quick check of patient name and an additional identifier such as date of birth or medical record number ensures that the correct patient is being reviewed. Checking the study date also confirms that the current study is being read (and not last year’s study!). Another good check is to glance at the charge code and the study performed to ensure that they match. Finally, checking the number of images in the study will help make sure none are skipped during your review.
Knowing the indication for the study and the patient history are also important. Occasionally women may have completed a screening mammogram before informing the technologist about a palpable lump or other newly discovered clinical finding. These findings should be described in your report and diagnostic imaging should be recommended. If the patient referred for screening shares clinical complaints prior to the examination, she should optimally be rescheduled for diagnostic imaging.
- •
Screening mammography typically consists of two views of each breast: the craniocaudal (CC) and mediolateral oblique (MLO) views. Screening is performed for women with no symptoms of breast cancer, so they should not have any new breast lumps, palpable thickening, or worrisome nipple discharge. Screening mammography can be performed for women with a prior lumpectomy for breast cancer if their mammograms have shown benign findings for a number of years (typically 2 to 5 years after diagnosis in our practices). Screening performed at multiple sites in the community provides easy access for women. Direct supervision by a radiologist is not required (i.e., a radiologist does not have to be present).
- •
Diagnostic mammography is performed to evaluate a breast symptom that may be due to breast cancer (e.g., palpable lump or breast thickening) or to evaluate an abnormal screening mammogram. Women with recent breast cancer typically undergo diagnostic mammography. Ultrasound is often performed in conjunction with diagnostic mammography. Diagnostic mammography is nearly always performed under the direct supervision and interpretation of a radiologist on site.
Positioning
A poorly performed mammogram is a significant disservice to the patient. Radiologists may fear that a report stating that the examination is technically inadequate will hurt a technologist’s feelings or that referring physicians will think poorly of the facility. However, everyone has a bad day now and then. No technologist is perfect. Every technologist occasionally will have patients who are just not positioned well. If feedback is given in a kind and supportive manner, it is often appreciated. If there is a trend of individual technologists having a high technical recall rate, focused feedback and training are helpful. Likewise, a facility often gains respect from referring health care providers if they understand that the radiologists expect the highest quality care for all patients. In our experience, consistent recall to repeat technically inadequate mammograms with feedback to the technologist is vital in creating and maintaining excellence.
An important point in understanding positioning for mammograms is that the upper inner quadrants of each breast (the cleavage area) are relatively fixed in position, whereas the inferior and lateral aspects of the breast are very mobile. This is why the technologist raises the image or film receptor when performing the CC view. There are cartoons jesting at why women have to stand on their toes for a mammogram. Now you know why! If you have never had a mammogram or seen one performed, ask a technologist if you can observe a screening mammogram. A good technologist is highly skilled at positioning even the most difficult patient. Ask her how she deals with women with very small breasts or who have a large abdomen. Watch how she works with the patient to obtain optimal compression. Your understanding (and respect for technologists) will be considerably elevated.
The Mediolateral Oblique View
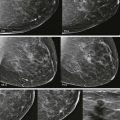
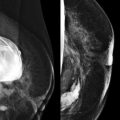
The MLO view is positioned with the image receptor parallel to the pectoralis major muscle (typically between a 60- and 45-degree angle) and extends into the axilla. The pectoralis major muscle should be seen to at least the level of the posterior nipple line ( Fig. 1-1 ).

Ideally, the inframammary fold should be visualized ( Fig. 1-2 ). The last maneuver of the technologist in positioning the MLO view is to move the breast “up and out” (see Fig. 1-2 ). This means that the breast is pulled up and away from the pectoralis muscle, which allows for optimal compression of the breast. If the breast is not pulled up and out, the breast may droop with a “camel nose” appearance.

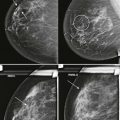
When the pectoralis muscle is thick, it may be difficult to obtain good compression of the front of the breast, particularly in large-breasted women. Some manufacturers address this issue by offering compression paddles that angle to allow compression of the anterior and posterior portions of the breast. Another approach is to obtain separate MLO views of the front of the breast, without the pectoralis muscle (front compression MLO views), to improve compression of the anterior breast ( Fig. 1-3 ). It is helpful to get patients to relax their shoulders to get the pectoralis muscle (and breast tissue) into the MLO view ( Box 1-1 ; Fig. 1-4 ).

If you do this simple exercise, you will forever understand how your best technologists get great muscle and why others do not. Hang your arm relaxed down by your side. Now, grab your pectoralis muscle at the top of your axilla. See how the muscle is nice and soft and fat? Next, raise your shoulder. Feel how the muscle becomes concave? The best technologists get patients to relax their shoulders down, pushing the pectoralis muscle (and breast tissue) into the mediolateral oblique (MLO) view. Technologists who are nervous or don’t get the patient to relax will struggle with MLO positioning ( Fig. 1-4 ).

When to Use a Lateral Medial Oblique View
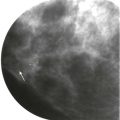
The LMO (lateral medial oblique) view is obtained in the same projection as the MLO except that the machine is flipped over so that the image receptor is in the cleavage and the tube head is nearer the floor. In certain situations the LMO view may be preferable to the MLO view. The smaller size of the image receptor near the patient’s head makes the LMO view useful for women with kyphosis or pectus excavatum ( Fig. 1-5 ). An LMO view may also require less manipulation of hardware when internal devices such as a pacemaker or port are present in the cleavage area.

The Craniocaudal View
The CC view is typically performed horizontal to the floor, though the receptor may be rotated about 5 degrees toward the axilla if needed. Again, the receptor should be elevated in order to mobilize the inferior breast and image the superior breast. The nipple should be centered in the image and not pointing toward the lateral corner of the image. The cleavage of the contralateral breast should remain on the receptor; if it is pushed back, then medial tissue from the breast of interest will also be pushed off the receptor.
The pectoralis muscle should be visualized on at least 30% of CC views (see Fig. 1-2 ). Obviously the image is positioned far enough back if the pectoralis muscle is seen. So how can one tell if a CC view is positioned well if the pectoralis muscle is not present? Let’s go back to the MLO view. The measured posterior nipple line should equal or be within at least 1 cm of the same line on the CC view (see Fig. 1-1 ). If it is not, then the CC view should be repeated.
For women who are very kyphotic, the CC from below (CCFB) view may improve visualization of the posterior breast tissue. This view is obtained by flipping the entire gantry upside down. The receptor (which is much smaller) is then in the area of the patient’s face, rather than the tube head.
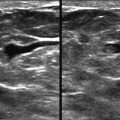
Nipple in Profile
The nipple should be in profile in one of the two views if possible. Sometimes the nipple can be mistaken for a mass and converging ducts as architectural distortion if it is not in profile ( Fig. 1-6 ). In addition, subareolar cancers can be difficult to visualize when the nipple is not in profile.