Fig. 8.1
The earliest working prototype, dubbed “Gen-1” and referred to as the Spy-Scope

Fig. 8.2
The Pinpoint System was commercially launched in January 2012 as the Pinpoint “Gen-2”

Fig. 8.3
“Gen-3” (the model currently available on the market)
Starting in July 2011, Novadaq began integrating spy-imaging technology into the 3-D HD imaging system of the daVinci robot (Intuitive Surgical, Sunnyvale, CA). The robotic version of this technology is referred to as Firefly. The Firefly is identical to the Pinpoint, except for minor differences in the white light portion of the image. In the daVinci Firefly, the green fluorescent data is projected on a background of a black and white laparoscopic image rather than the full colored image of the Pinpoint. There is significant overlap between work done with the Pinpoint and Firefly since both are fundamentally endoscopic NIR systems but we will be limiting our discussion in this chapter to the Pinpoint.
Our group and others have mainly concentrated on the use of Pinpoint for the following four major indications and we will be dividing the following sections of this chapter into these four fields of interest. Firstly, will be a discussion regarding our work with the Pinpoint in colorectal perfusion and prevention of anastomotic leak. Secondly, we will discuss our experience using the Pinpoint for intraoperative cholangiography primarily during laparoscopic cholecystectomy. Thirdly, we will discuss our early experience using the pinpoint for sentinel lymph node dissection for colorectal and gastric malignancies. Lastly, we will discuss other uses and potential future directions of this technology.
Colorectal Evaluation of Perfusion
The influence of perfusion on colorectal anastomotic healing, and conversely the role of ischemia on anastomotic dehiscence has been thoroughly reported [5–7]. Anastomotic leak is a devastating complication in colorectal surgery and is especially prevalent in low rectal anastomoses with some reports describing a leak rate as high as 20 % [8]. Besides for the acute effects of sepsis, there is long-term morbidity including: stricture formation, bowel dysfunction, and an increased risk of locoregional cancer recurrence [9, 10]. Ischemia is the likely predisposing factor in the majority of cases. Anatomic variations of the vascular supply to the colon (especially the descending and sigmoid colon), atherosclerotic disease of the mesocolic vasculature, injury to the vasa recta by over-dissection, tension on the anastomosis, and mis-oriented bowel all affect the final blood supply to the anastomotic ring and hence impact healing and by extension can lead to leak.
In order to be useful, information regarding perfusion must be available intraoperatively when intervention is possible. However, the clinical incorporation of technologies capable of intraoperatively evaluating perfusion has been limited. This is primarily because these technologies are highly user-dependent, difficult to use and involve a steep learning curve and thus have never become commercially available [11]. We hypothesized that by using a visually based tool capable of being advanced under direct vision to the point of interest and then able to assess the entire area in question would resolve the problems experienced with these previous perfusion assessment tools. Furthermore, since mucosa is more susceptible than serosa to minor alterations in perfusion, transanal assessment of flow should be an especially sensitive test for bowel ischemia [12–14].
We evaluated the use of Pinpoint to transanally evaluate anastomotic perfusion in patients undergoing colorectal anastomoses [15]. The study was approved by the ethics review board of our institution. We enrolled seven patients undergoing LAR for benign or malignant disease of the sigmoid or rectum with anastomoses expected to lie within 25 cm of the anal verge. Prospectively, demographic data, indications for surgery, distance of the anastomosis from the anal verge, and other factors known to affect anastomotic healing were collected. After completion of the resection and the creation of an anastomosis using a double stapled, end-to-end technique, the doughnuts were checked for completeness and an air leak test was performed.
Although the Pinpoint was designed for laparoscopic use, visual inspection of the anastomosis and evaluation of the proximal and distal segments for viability was made possible by using a rigid procto-sigmoidoscope (Welch Allyn, Skaneateles Falls, NY) mated with a laparoscopic trocar to allow the use of the Pinpoint system transanally (Fig. 8.4) [16].


Fig. 8.4
Although the Pinpoint was designed for laparoscopic use, visual inspection of the anastomosis and evaluation of the proximal and distal segments for viability was made possible by using a rigid procto-sigmoidoscope (Welch Allyn, Skaneateles Falls, NY) mated with a laparoscopic trocar to allow the use of the Pinpoint system transanally
The Pinpoint scope was inserted into the rectum to the level of the anastomosis and the staple line and proximal and distal margins of the anastomosis were visualized. 1 ml (2.5 mg reconstituted) of ICG was injected via a peripheral IV catheter as a rapid bolus just prior to imaging. Fluorescence was evaluated subjectively by the surgeon as being hypo-, iso-, or hyperfluorescent as compared to surrounding bowel using the distal rectum as the benchmark of maximal fluorescence. An ICGA was considered normal if the distal colon, proximal rectum, and distal rectum were all iso-fluorescent (Fig. 8.5). A decision was then made regarding the need for revision and/or proximal diversion. All patients were followed up at least twice postoperatively, at 1 week and 1 month post discharge.
Fig. 8.5
An ICGA (indocyanine green) was considered normal if the distal colon, proximal rectum, and distal rectum were all iso-fluorescent
Five of seven patients were women. Mean age was 70.29 (+11.44, range 51–85) and operative time ranges from 173 to 296 min (mean 218.00 min, +43.11). Mean length of hospital stay was 4.71 days (+1.38, range 3–6). All anastomotic doughnuts were complete and none of the anastomoses leaked during air testing.
Normal, pink and healthy appearing mucosa and a complete anastomotic staple line were noted in all cases. The sequence of uptake (colon → rectum vs. rectum → colon) varied, but in all subjects both the proximal and distal margins of the anastomosis appeared iso-fluorescent.
None of the patients in this group experienced a clinically significant anastomotic leak and no adverse events were identified due to the use of the ICG or Pinpoint system. At the 1 month follow up, all were doing well.
We concluded that due to the devastating consequences of an anastomotic leak, there is a need for a modality that can accurately and consistently assess bowel perfusion in real time. The pinpoint system is the first system that allowed a transanal view of mucosal viability and evaluation of perfusion to the anastomotic ring.
Success in imaging these first seven patients and the outstanding images the Pinpoint generated encouraged us to open this study up to an additional 100 patients undergoing colorectal resections for benign and malignant disease.
This study was approved by the Ethics Review Board at our institution. Twenty consecutive patients undergoing LAR for benign or malignant disease were reviewed [17]. Patient demographics, indications for surgery, comorbid conditions, and other factors known to affect healing (steroid use, previous pelvic irradiation, smoking history) were entered prospectively into a database. All operations were performed laparoscopically using a standard double-stapled technique. Following completion of the anastomosis, the mucosa of the colon, rectum and anastomotic staple line were visually inspected with a standard rigid procto-sigmoidoscope. An air leak test was then performed and the decision to revise the anastomosis and/or divert the fecal stream with a loop ileostomy was based on clinical grounds.
Using a similar protocol, we injected 1 ml of ICG via a peripheral IV catheter as a single rapid bolus, NIR angiographic images were obtained transanally using the Pinpoint system. Uptake of ICG was evaluated subjectively by the operating surgeon and video recorded. Fluorescence was evaluated by employing a scoring system. A fluorescence score (FS) of 1–5 (1—no uptake, 5—maximal uptake) for each segment of the anastomosis and the staple line was assigned to each patient. Additional parameters including sequence of uptake and time to maximal excitation of all bowel segments were recorded. All patients were followed up postoperatively at 1 week and 1 month.
Of the 20 patients, 14 were women. The mean age was 67.2 (SD + 14.9). The indications for surgery included malignant disease of the colon or rectum and diverticular disease. The mean distance of the anastomosis from the anal verge was 11 (+3) cm, operative time ranged from 121 to 234 min (mean 170 + 33.4). Complete anastomotic doughnuts and a negative air leak test were achieved in all patients. Out of 20 patients, four exhibited abnormality of flow on ICG evaluation. Three exhibited a significant hypofluorescence (FS 3) and one had patchy fluorescence (FS 2). Uptake of colonic mucosa preceded the rectum in the majority of cases (17/22, 85 %) and the staple line fluoresced in only a minority of cases (1/20, 5 %). In two of the patients with hypofluorescence, the surgeon had already decided to perform a diverting loop ileostomy based on visual evaluation of the perfusion of the proximal bowel in one patient and the very low level of the anastomosis in the second patient. Both diverted patients did well postoperatively. The other two patients with low FS had adequate perfusion by clinical parameters, yet appeared to have inadequate uptake of ICG in the proximal colon on imaging. As an early feasibility study and as per protocol, no change in operative management was made based on the ICGA findings. Postoperatively, both patients experienced delayed return of bowel function and febrile episodes, and CT scans performed revealed peri-anastomotic collections consistent with minor anastomotic leaks. They were treated conservatively with antibiotics and subsequently showed clinical improvement and were discharged home on postoperative days 10 and 13. Follow-up imaging confirmed resolution of the collection in both cases. The remaining patients were discharged home with a mean hospital stay of 4.75 (+1.0) days. At 1-month follow-up, all 20 patients were doing well.
In light of the findings in these 20 patients plus an additional 19 patients accrued to that point, the IRB was petitioned to amend the study protocol to allow for intraoperative decision making based on ICGA findings (Video 8.1). The following 41 consecutive patients undergoing colectomy for benign or malignant disease were managed based on clinical and ICGA findings (Group B) and then compared retrospectively to the initial 39 patients managed by clinical parameters alone (Group A) (unpublished data). Patient demographics, indications for surgery, comorbid conditions, and other factors known to affect healing did not differ significantly between groups. In Group B, prior to ICG imaging clinical assessment of both the proximal and distal margins of resection were made and clips placed at the planned transection sites. In Group B, four changes in management were made based on ICGA findings (Video 8.2). All of these revisions manifested as more extensive resections of the proximal or distal colon due to hypo-fluorescence of these segments on ICG angiography. In each of these cases clinical assessment had failed to identify areas of hypo-perfusion and would have led to an anastomosis in these regions. In one of the cases requiring more extensive resection, an additional 12 in. of left colon was found to have been devascularized but had appeared normal by examination alone. No patients had diversions based on ICGA findings. Patients in each group were followed up at 1 week and 1 month postoperatively.
In Group A, two patients manifested minor leaks, requiring prolonged hospitalizations and antibiotic treatment (see above) while in Group B no leaks were identified.
These encouraging results have led to an expanded interest internationally in fluorescence for the assessment of colorectal anastomotic perfusion. Although the cause of anastomotic leak is most certainly multifactorial, our data indicate that eliminating hypo-perfusion can significantly impact outcomes. Further study in a multicenter and ultimately in a randomized control study termed the “perfusion assessment in laparoscopic left anterior resection” or PILLAR II and PILLAR III trials respectively will hopefully bear out these early findings.
Intraoperative Cholangiography
Intraoperative cholangiography (IOC) has been shown to be helpful in delineating biliary anatomy and may prevent main duct injury during laparoscopic cholecystectomy. A number of large population-based reports support this contention and indicate that routine IOC does appear to further reduce the incidence of BDI or at minimum allows for earlier recognition and repair of injuries [18–20]. Despite these benefits, the need for ionizing radiation and injection of a contrast agent directly into the biliary system has prevented IOC from becoming routine. Fluorescent cholangiography using an intravenously injected fluorophore and near infrared (NIR) imaging provides similar anatomical detail without the drawbacks of radiographic cholangiography (Video 8.3).
The Pinpoint system is ideal for this application since it provides NIR cholangiography mated with the standard high definition (HD) white light laparoscopic view producing an uninterrupted, augmented view of the anatomy (Fig. 8.6). The benefits of NIR cholangiography include:
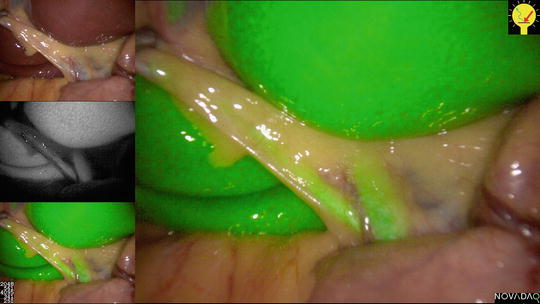
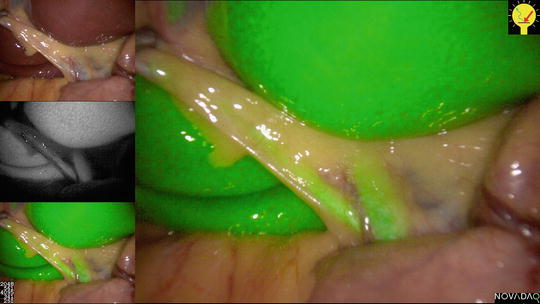
Fig. 8.6
The Pinpoint system provides near infra-red (NIR) cholangiography mated with the standard high definition (HD) white light laparoscopic view producing an uninterrupted, augmented view of the anatomy
Does not require puncture of the biliary system
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree