Fig. 43.1
(a) Transverse image from a pelvic ultrasound (US) shows a normal-appearing placenta (asterisk). (b) In a different patient, the US shows a focal hemorrhage (arrows) within the placenta due to focal abruption
Women with no apparent significant injury, without concerning physical examination findings such as vaginal bleeding or uterine tenderness, who have a normal 6 h CTM tracing without evidence of contractions or abnormal fetal heart rate variability, can be safely discharged from the hospital. An extended period of CTM for 24 h is required If:
any monitoring abnormality is identified during the initial monitoring
the mother requires admission for management of her injuries
the mother requires general anesthesia
the mother is clinically considered to be at high risk for fetal complications based on history or mechanism of injury.
Also, direct trauma to the uterus can cause release of decidual lysosomes and arachidonic acid metabolites that can result in uterine contractions and can induce premature labor and pre-term delivery.
Trauma Management in Pregnancy
Despite two individuals being at risk, the first and primary goal in treating a pregnant trauma victim is maternal stabilization. Achieving maternal wellbeing offers the best chance for preventing fetal morbidity and mortality. Simple measures like preventing hypotension through compression of the vena cava by placing pregnant patients greater than 20 weeks gestation in the left lateral decubitus position throughout resuscitation will help decrease potential fetal problems.
Early obstetric consultation should be obtained while initial resuscitation and assessment are occurring. A full obstetric history should be included along with the usual history and physical examination. An estimation of gestational age derived from the history and by accessing fundal height is an important factor in the decision regarding early delivery if needed. In addition to the trauma physical examination, a pelvic examination is required to rule out factors associated with fetal or placental injury, such as vaginal bleeding, ruptured membranes, or a bulging perineum.
Screening
Assault or interpersonal violence effects up to 20 % of all pregnant women sometime during gestation, though perhaps as few as 4–10 % of cases present for medical care. Such violence is commonly associated not with just a single event, but rather multiple episodes are the norm (Fig. 43.2). Violence occurs across all races and socioeconomic levels. Its been shown that abused mothers are twice as likely to begin their prenatal care in the third trimester. Women who report a history of abuse are at increased risk of poor fetal outcome. Interestingly, women who decline to be interviewed for interpersonal violence have even higher rates of fetal complications. Because a single trauma admission may be the only chance to pick up these types of events before a serious maternal or fetal injury may occur, screening using a validated three question questionnaire is currently recommended and included in advanced trauma life support (ATLS) recommendations (Table 43.1.) Interpersonal violence should be considered when:
the injuries appear to be inconsistent with the history,
the patient has a history of depression, substance abuse, self-abuse or suicide attempts,
the patient blames herself for the injuries,
the partner seems controlling and tries not allow the patient to be examined without him,
the patient has had frequent visits.
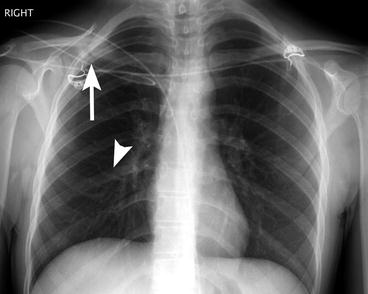
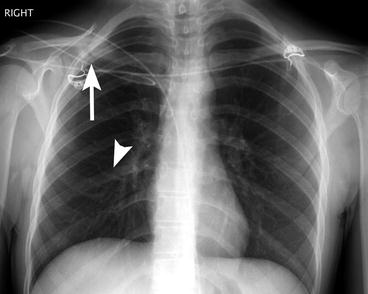
Fig. 43.2
Chest radiograph shows an acute, non-displaced rib fracture (arrowhead) and a healed clavicle fracture from possible prior domestic abuse
Table 43.1
Interpersonal violence screening questionnaire
Have you been kicked, hit, punched or otherwise hurt by someone within the past year? |
Do you feel safe in your current relationship? |
Is there are partner from a previous relationship who is making you feel unsafe now? |
Imaging Considerations for the Pregnant Patient
As in other trauma scenarios, imaging plays a major role in the diagnostic assessment of the pregnant trauma patient. Choosing the proper imaging examination to evaluate the pregnant patient can pose a dilemma for the clinician who is trying to facilitate prompt diagnosis while balancing radiation dose. Although imaging modalities that do not use ionizing radiation, such as US and magnetic resonance imaging (MRI), are strongly preferred when possible, their limitations can be substantial. The availability, speed and reliability of computed tomography (CT) are advantageous, but CT is associated with significant radiation exposure. Plain radiography and angiography are additional potential sources of ionizing radiation used in this setting. Although there are theoretical risks of fetal carcinogenesis, congenital malformations and mental retardation, there is no documented risk at current exposure levels commonly associated with diagnostic imaging. The risk of abnormality is considered to be negligible at 50 mGy or less. Practice guidelines for imaging the pregnant patient are based on the guiding principle that the mother’s health is the most important factor for fetal survival and favorable outcome. Therefore, concerns regarding fetal radiation dose exposure should not delay or preclude radiologic evaluation in trauma patients requiring accurate and prompt diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree