Abstract
Objective
To investigate the relationship between the rim-like enhancement pattern on pre-ablation contrast-enhanced ultrasound (CEUS) of colorectal liver metastasis (CRLM) and the therapeutic efficacy of percutaneous microwave ablation (MWA).
Methods
Patients with CRLM underwent MWA and were evaluated using CEUS before ablation in our hospital between February 2020 and February 2023 were enrolled in this retrospective study. The enhancement patterns of CRLM were assessed by two radiologists and classified as rim-like enhancement and non-rim-like enhancement patterns. The therapeutic outcomes, including cumulative intrahepatic progression rate and early intrahepatic progression rate, were followed up and analyzed.
Results
Overall, 50 patients with 121 nodules were enrolled. Rim-like enhancement pattern was observed in 18 patients (18/50, 36.0%). The cumulative intrahepatic progression rate was significantly higher in the rim-like enhancement group than the rate in the non-rim-like enhancement group ( p = 0.022). The early intrahepatic progression rate in the rim-like enhancement group was also significantly higher than the rate in the non-rim-like enhancement group (12/17, 70.6% vs. 6/24, 25.0%, p = 0.005). The multivariable analysis demonstrated that the rim-like enhancement pattern of CRLM was a significant risk factor associated with early intrahepatic progression after MWA ( p = 0.013).
Conclusion
Rim-like enhancement pattern on pre-ablation CEUS of CRLM was associated with a higher risk of intrahepatic progression after MWA.
Introduction
Colorectal cancer is the third most common type of cancer in the world, and up to 50% of individuals with colorectal cancer present with liver metastases throughout the disease [ , ]. Although surgical resection is the first-line local treatment for colorectal liver metastasis (CRLM), approximately 80% of CRLM patients are unresectable due to extensive disease or concurrent medical conditions [ ]. Percutaneous thermal ablation is an important alternative local treatment for unresectable CRLM [ ]. However, a high early intrahepatic progression rate after the ablation treatment impedes the overall therapeutic efficacy [ ]. Thus, developing predictive markers to identify CRLM cases at high risk of early intrahepatic progression after thermal ablation is crucial and helpful for treatment decisions.
Contrast-enhanced ultrasound (CEUS) plays a critical role in localization, planning, guidance and evaluation of thermal ablation for liver tumors [ ]. It is worth noting that CEUS is also becoming a promising method for therapeutic response prediction of liver cancers [ , ]. Rim-like enhancement is a common contrast-enhanced imaging characteristic that refers to the tumor with a peripheral hyper-enhanced signal and a central hypo-enhanced signal in the arterial phase, frequently presented in malignant liver tumors [ ]. In practice, rim-like enhancement pattern was observed more often in CRLM than in other types of liver cancer. A previous study has reported that the rim-like enhancement pattern was more likely present in perineural invasion and RAS mutation colorectal cancer [ ]. However, the relationship between rim-like enhancement pattern and exact prognostic significance of thermal ablation treatment in CRLM has not been studied.
Therefore, this study was aimed at investigating the relationship between the rim-like enhancement pattern on pre-ablation CEUS of CRLM and the therapeutic efficacy of percutaneous microwave ablation (MWA).
Materials and methods
Patients
Between February 2020 and February 2023, consecutive patients with CRLM underwent MWA and evaluated using CEUS before the ablation in our hospital were enrolled. Patients with unresectable CRLM or those who refused surgical operation were referred for MWA following a multi-disciplinary team discussion. CRLM was confirmed by pathological biopsy results or typical radiological imaging with histology of primary colorectal cancer [ ]. Patients were excluded due to (i) multiple primary tumors, (ii) incomplete data of CEUS images and (iii) no available follow-up data.
This retrospective study has been approved by the Institutional Ethics Review Board of our hospital (Approval No. 2024-157-01).
Ultrasound examination and imaging evaluation
Two types of ultrasound machines (Logiq E9, GE Healthcare, Milwaukee, WI, USA) and Mindray R9 (Mindray Medical International, Shenzhen, China) were used for the ultrasound examination. All the ultrasonic examinations were performed by three radiologists (with more than 5 y of experience in liver CEUS). Conventional ultrasound examination was performed first to explore the entire liver and assess the location, size and echoic characteristics of the target nodule. A dose of 1.5 mL contrast agent (Sulphur Hexafluoride Microbubbles, SonoVue, Bracco Imaging, Milan, Italy) was quickly injected intravenously via the antecubital vein, followed by a flush of 5 mL normal saline promptly. The video of the whole CEUS procedure, including the arterial phase (from injection to 30 s), portal venous phase (30–120 s) and delay phase (120–300 s) was recorded for subsequent evaluation [ ].
All the ultrasound images were evaluated independently by two radiologists (with 2 and 5 y of experience in liver CEUS, respectively) blinded to patient identification and clinical information. For patients with multiple CRLMs, ultrasonic characteristics of the largest one were recorded. The initial results of ultrasonic characteristics from two radiologists were recorded respectively for the inter-observer agreement test. If the initial results between the two radiologists were discordant, consensus after discussion was used for final statistical analyses.
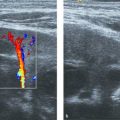
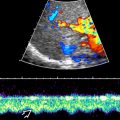
The enhancement patterns of CRLM on CEUS were defined as (i) rim-like enhancement pattern: peripheral high signal-enhanced area with central relatively low signal intensity in arterial phase; (ii) non-rim-like enhancement pattern: other enhancement characteristics including heterogeneous or homogeneous enhancement in arterial phase. Examples of CRLM with or without rim-like enhancement are shown in Figure 1 .

MWA procedure and follow-up
Under general anesthesia, all the MWA procedures were performed percutaneously by the same physician (with 15 y of experience in thermal ablation). Ultrasound fusion imaging was used for detection, guidance, monitoring and evaluation throughout the ablation procedures to achieve a sufficient ablative margin (≥5 mm) to the greatest extent possible by multiple overlapping ablations [ ]. For nodules located less than 5 mm from the liver capsule or vessels, the ablative margin was extended to be as close as possible to the capsule or vessel wall.
Following 10–15 min of the initial MWA procedure, patients underwent CEUS combined with ultrasound fusion imaging to evaluate technical success. Within 3 mo after the MWA procedure, patients underwent contrast-enhanced CT/MR to evaluate technique efficacy. After that, patients were followed up every 3 mo to assess any intrahepatic progression [ ]. Local tumor progression was defined as tumor recurrence at the edge of the ablation zone in adequate ablation cases during the subsequent follow-up. Intrahepatic progression included local tumor progression and new metastases in the liver after the ablation. Early intrahepatic progression was defined as 1-y disease progression in the liver after the ablation. Intrahepatic progression-free survival was calculated from the day of the ablation until the intrahepatic tumor progression detection or the last follow-up. Overall survival (OS) was calculated from the day of the ablation until the last follow-up or death [ ]. All patients were followed up until death, study dropout or data analysis time (October 2023).
Statistical analyses
Clinicopathological characteristics of patients were collected from medical records. The statistical analyses were performed using SPSS 26.0 (SPSS, Chicago, IL, USA) and GraphPad Prism 8.3.1 (GraphPad Software Inc., San Diego, CA, USA). Continuous variables were presented as mean (standard deviation) and analyzed by the Student’s t -test or Wilcoxon rank-sum test. Classified variables were presented as numbers (percentages) and analyzed by Fisher’s exact or Chi-square tests. The inter-observer agreement of enhancement patterns of CRLM between two radiologists was tested by Cohen’s kappa coefficient analysis. The cumulative intrahepatic progression rate and OS rate were performed using the Kaplan–Meier method, and the survival differences between subgroups were compared using the log-rank test. Risk factors for early intrahepatic progression were assessed using univariable and multivariable logistic regression analyses. A p value <0.05 was considered to be a significant difference.
Results
Baseline patient characteristics
From February 2020 to February 2023, 56 patients with CRLM who underwent CEUS examination within 1 wk before the MWA procedure in our hospital were initially included in this study. Six patients were excluded due to two primary cancers ( n = 2), incomplete CEUS data ( n = 1) and lost follow-up after ablation ( n = 3). Finally, 50 patients (age range, 30–83 y) with 121 nodules (size range, 9–55 mm) were enrolled. The median follow-up period was 19 mo (range, 5–39 mo). The primary tumors of all patients were treated by surgery before the ablation procedure or during the same period. Most patients (46/50, 92.0%) received post-operative adjuvant therapy. The clinical characteristics of the analyzed patients and nodules are summarized in Table 1 .
| Characteristics | Results |
|---|---|
| Patients | 50 |
| Age, y | 61.5 (12.7) |
| Male/female | 27 (54.0%)/23 (46.0%) |
| Synchronous Metastasis/metachronous | 34 (68.0%)/16 (32.0%) |
| Preoperative chemotherapy | 37 (74.0%) |
| Primary/recurrence | 37 (74.0%)/13 (26.0%) |
| Extrahepatic disease | 20 (40.0%) |
| CEA level >30 ng/mL | 11 (22.0%) |
| Post-operative adjuvant therapy | 46 (92.0%) |
| Maximum tumor diameter | 23.1 (11.2) |
| Maximum tumor size ≥30 mm | 14 (28.0%) |
| No. of liver metastasis | |
| 1 | 24 (48.0%) |
| 2–3 | 14 (28.0%) |
| >3 | 12 (24.0%) |
| Nodules, n | 121 |
| Tumor size ≥30 mm | 19 (15.7%) |
| Perivascular | 27 (22.3%) |
| Subcapsular | 68 (56.2%) |
In this study, all the enrolled nodules achieved the completed ablation confirmed by immediate US fusion imaging combined with CEUS and contrast-enhanced CT/MR after the ablation procedure. Three nodules (3/121, 2.5%) were detected in local tumor progression during the follow-up period. A total of 24 patients (24/50, 48.0%) experienced intrahepatic progression, and the median intrahepatic progression-free survival was 19 mo (95% CI [4.6, 33.4]). Nine patients died until the last follow-up, and the median OS had not been reached.
Clinical characteristics by rim-like enhancement status
Rim-like enhancement pattern was observed in 18 patients (18/50, 36.0%). The Cohen’s kappa coefficient for rim-like enhancement assessment from two radiologists was 0.87, manifesting a solid inter-observer agreement. No difference in clinical characteristics between the two enhancement pattern groups was observed ( Table 2 ).
| Characteristics | Rim-like ( n = 18) | Non-Rim-like ( n = 32) | p |
|---|---|---|---|
| Age, y | 62.7 (13.2) | 60.0 (12.0) | 0.461 |
| Male/female | 10 (55.6%)/8 (44.4%) | 17 (53.1%)/15 (46.9%) | 0.100 |
| Location of primary tumor | 0.594 | ||
| Right colon | 5 (27.8%) | 7 (21.9%) | |
| Left colon | 3 (16.7%) | 10 (31.3%) | |
| Rectal | 10 (55.6%) | 15 (46.9%) | |
| Primary/recurrence | 14 (77.8%)/4 (22.2%) | 23 (71.9%)/9 (28.1%) | 0.746 |
| Preoperative chemotherapy | 13 (72.2%) | 24 (75.0%) | 1.000 |
| PD during chemotherapy | 6 (33.3%) | 6 (18.8%) | 0.309 |
| Extrahepatic disease | 8 (44.4%) | 12 (37.5%) | 0.765 |
| CEA level >30 ng/mL | 4 (22.2%) | 7 (21.9%) | 1.000 |
| Post-operative adjuvant therapy | 15 (83.3%) | 31 (96.9%) | 0.127 |
| Maximum tumor size ≥30 mm | 6 (33.3%) | 8 (25.0%) | 0.744 |
| No. of liver metastasis | 0.551 | ||
| 1 | 8 (44.4%) | 16 (50.0%) | |
| 2–3 | 4 (22.2%) | 10 (31.3%) | |
| >3 | 6 (33.3%) | 6 (18.8%) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree