8 The shoulder
Introduction
Upper extremity pain and, more specifically, shoulder pain is a common complaint in the general population1,2 and is a familiar presentation to any physician in primary care.2–4 The incidence of new episodes of shoulder pain is approximately 11 per 1000 presentations in general practice,2 making it responsible for 16% of all musculoskeletal complaints.1 The complex arrangements of soft tissue structures in the shoulder joint, as well as its proximity to significant neurovascular anatomy, renders it a difficult joint to assess, while the combination of the joint’s instability and mobility subject it to an increased probability of injury.5,6
A multitude of pain generators can be responsible for shoulder pain and these are not merely limited to local structures; referred pain from spinal structures is also a common cause of shoulder pain.7,8 This myriad of clinical factors requires the primary care physician to have an advanced understanding of shoulder joint anatomy and pathophysiology, as well as a more than cursory knowledge of appropriate physical examination and diagnostic imaging procedures to correctly diagnose an injury.
Evaluation of the shoulder joint typically includes plain film radiography; however, many common shoulder complaints involve soft tissue structures not detectable using radiographs. Magnetic resonance (MR) imaging offers unmatched anatomical detail, relative ease of assessment and high accuracy and allows multiplanar assessment.9,10 These attributes have made MR imaging the procedure of choice for evaluation of occult fractures, articular structures and soft tissues of the shoulder including tendons, ligaments, muscles and capsulolabral structures11 despite its relatively high cost and occasional limited availability in some regions.12
History and examination
In assessing the painful shoulder, it is necessary to evaluate all possible pain generators and contributing conditions. While many shoulder disorders have their signature clinical presentations, many also tend to precipitate secondary conditions or are common comorbidities; it is relatively uncommon for an isolated condition to be the sole cause of shoulder pain in a patient.13
Of key importance to the diagnostic process is an accurate history of both the present complaint and previous episodes; occupational- and sports-related factors; epidemiological data; injury pathomechanics; exacerbating activities; and other diagnosed conditions that may (or may not) directly affect the shoulder joint. In most cases of shoulder pain, a careful, well-directed history will lead to a correct diagnosis.14,15
Physical examination procedures including specific provocative tests are vital to the diagnostic picture and play a large role in directing imaging and, consequently, management decisions. Both active and passive range of motion and muscle testing will provide important information to the clinician, although many traumatic injuries may limit the ability to perform them. It is important not to mistake muscle failure resulting from the pain induced by provocation testing with muscle weakness. Palpation will help to localize the site of pain as well as identify palpable deformities related to dislocations or separations. The differential diagnosis can be further refined by conducting special tests; these tests, their associated clinical findings and significance are discussed later in conjunction with the conditions to which they pertain in order to allow the physician to correlate their imaging findings with their investigative procedures.14
Assessment of shoulder pain also necessitates evaluation of the cervical spine owing to the frequency of complaints coexisting in both areas.16,17 Pain related to the majority of common shoulder conditions typically does not extend beyond the elbow; this finding should direct the clinician towards a cervical, brachial plexus or peripheral nerve lesion.8
Differential diagnosis
The range of common conditions that can mimic shoulder injury is detailed and discussed in Table 8.01.
Table 8.01 Differential diagnosis of shoulder conditions
| Condition | Effect on shoulder | Clinical features |
|---|---|---|
| Biliary disease | Right-sided pain | |
| Blood or gas in peritoneal cavity | Referred to side of diaphragmatic irritation | |
| Blood or gas in pleural cavity | Referred to side of diaphragmatic irritation | |
| Subphrenic abscess | Referred to side of diaphragmatic irritation | Concomitant abdominal symptoms |
| Cardiac disease | Left shoulder pain | |
| Splenic trauma | Left shoulder pain | |
| Polymyalgia rheumatica | Bilateral |
Clinical indications for diagnostic imaging
If the history and examination are sufficiently proficient, then often the diagnosis will be self-evident and no diagnostic imaging required. However, in the event of significant trauma; if the patient’s pain is uncontrolled or precludes adequate physical examination; or in the event that the patient fails to respond to conservative therapy, there is an occasionally confusing wealth of imaging possibilities available to the physician.18
Plain radiographs are often still the first step in diagnostic imaging and can reveal fractures, dislocation and neoplastic osseous lesions; pathology in the thoracic outlet/inlet; acromioclavicular joint changes; calcification of soft tissues; and degenerative joint disease. The most common protocol for the shoulder is anteroposterior views with the shoulder in internal and then external rotation and ‘baby arm’ (neutral abduction); these views may be supplemented by transaxillary, scapular outlet or ‘Y’ (Lamy) views if indicated by the clinical findings.19–21 The physician also must consider whether acromioclavicular, cervical spine or chest x-rays are required.
Ultrasound, as a diagnostic modality, has developed markedly over recent years to the point where it can rival MR imaging in its depiction of soft tissue pathology in certain instances; these include the principal shoulder tendons. Although it is unlikely to supplant MRI as the primary means of evaluating tendon pathology and is dependent on operator skill, ultrasound plays an important role in the evaluation of the rotator cuff and offers a number of obvious advantages, including lack of ionizing radiation, portability in the office setting, high patient acceptance, low cost, and lack of medical contraindications.22,23
MR imaging has become the gold standard for diagnostic imaging of the shoulder, particularly with regard to injuries of the soft tissues. It is non-invasive and offers a high degree of resolution, enabling the evaluation of multiple potential pathological processes. It should be considered by the clinician whenever further evaluation of non-osseous structures is required, or as a follow-up to inconclusive plain film radiographs.18
Techniques and protocols
MR imaging of the shoulder should enable visualization of the anatomy surrounding the glenohumeral and acromioclavicular joints in the axial, and oblique sagittal and coronal planes. Whilst the neurovascular bundle can be visualized on typical shoulder MR images, separate MR neurography studies are required to assess the brachial plexus.10 MR imaging of the shoulder customarily includes images in all three planes with T1-weighted, T2-weighted and proton density (PD) sequences. Fat saturation techniques are usually performed only upon request and are becoming more popular during faster acquisition sequences (fast spin echo and gradient echo); their utility will be discussed later.
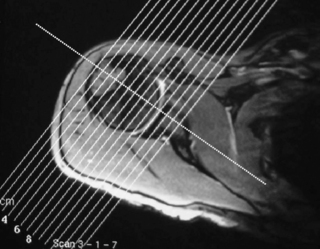
The localizer, or ‘scout’, is a single axial view through the glenohumeral joint, used to plan all the subsequent acquisitions (Figure 8.01). This view allows for the sagittal slices to be obtained parallel to the glenoid fossa; these are termed sagittal obliques, owing to their non-parallel relationship to the true anatomical plane. Based on the scout view, the coronal oblique slices are obtained perpendicular to the glenoid fossa, parallel to the supraspinatus tendon. The fibres of the supraspinatus tendon, as well as the glenohumeral joint, are slightly oblique to the true coronal plane, hence the images are orientated to reflect this, and the resultant images are termed coronal obliques. If true or direct coronal images were to be obtained, the supraspinatus muscle and tendon would appear discontinuous and shortened, mimicking tears.10,24,25
Patient placement and cooperation are critical during the procedure. The patient should lie supine with the involved arm at their side, supported by sponges, in neutral to slight external rotation. A surface coil will most likely be used to ensure greater image quality. Because the shoulder joint will be lateral to the isocentre of the magnet, the diagnostic area of the magnetic field will be inhomogeneous, which may lead to artifacts and lower-quality images without the use of a coil.10,25
Extreme rotation of the arm is not recommended, even if it allows good visualization of the glenoid labrum. This position is difficult to maintain for patients, causing pain, distorting the biceps tendon and increasing the chance for motion artifacts (figure motion artifact). In this position, the synovium can also become redundant and may mimic a soft tissue mass.24,25 If the arm is placed in internal rotation, the supraspinatus tendon curves anteriorly and leaves the oblique coronal plane and the capsule will appear lax.26 Increased overlap of supraspinatus and infraspinatus tendons, as well as signal changes at the infraspinatus insertion, may mimic tears. It is important to note that a small percentage of shoulders will demonstrate these findings when imaged in the neutral position as well,27 making it necessary to evaluate suspected findings in all planes and with all sequences.
Some authors have also suggested image acquisition during complete abduction and external rotation of the arm, termed the ABER manoeuvre (Figure 8.02). Studies have shown better visualization of partial cuff tears and labrum tears utilizing this position in conjunction with arthrography than images obtained with arthrography only.28–30 This position is, however, difficult to maintain for long periods of time, decreasing patient compliance and increasing pain level and motion artifacts.10,24,25 Even experienced technicians require additional time for patient placement, positioning and image acquisition, adding substantial time to an already time-consuming procedure. These images will usually be obtained during MR arthrography and are typically reserved for inconclusive findings on conventional MR or arthrography.31
As a general guide, T1-weighted sequences have the highest level of anatomical detail. Bone marrow and peri-articular fat both display high signal intensity. On T2-weighted images, soft tissue oedema or other fluid collections, such as that seen in bursitis, are depicted as high intensity zones. These sequences are also better suited for identification of pathologies and may help in the assessment of artifacts found on T1-weighted images, such as the ‘magic angle’ phenomenon: when a structure is oriented at 55° to the main magnetic field, it will appear as an area of hyperintensity on T1-weighted sequences, mimicking pathology.32 This angle has been termed the ‘magic’ angle and can appear in MR imaging of various body regions, including, in the shoulder, the supraspinatus tendon, glenoid labrum and biceps tendon. Muscle, ligaments and tendons will appear as areas of low signal intensity on both sequences. Proton density-weighted sequences use a relatively long relaxation time (TR) and short echo time (TE) and have shown a high sensitivity for detection of injury to the rotator cuff and glenoid labrum and capsular complex. Fast spin echo (FSE) sequences have more recently been used to decrease imaging time and improve signal-to-noise ratio. Fat will appear brighter with this technique, which may obscure small lesions adjacent to lipid structures, including subtle defects of the rotator cuff tendons and pathological bursal fluid.33 Fat saturation techniques can minimize these effects and help with the differentiation between fluid and fat at their interface; this can increase the sensitivity for detecting partial tears.34
Use of intra-articular contrast (arthrography) may enhance partial articular surface tears of the rotator cuff muscles or increase conspicuity of the capsulolabral anatomy;35–37 however, it is usually performed only on unresponsive patients or after an inconclusive non-contrast study. To perform the procedure, a needle is inserted into the glenohumeral joint under fluoroscopy. In order to verify intra-articular positioning, a small amount of iodinated contrast is injected and an image is taken to confirm correct placement. Following this, 10 to 16 ml of dilute gadopentetate dimeglumine is injected in to the intra-articular space, avoiding both the introduction of air and overdistension of the joint.38 An alternative procedure involves injection of saline solution followed by gentle shoulder mobilization (within patient tolerance) prior to the FSE MR imaging study.31 The use of local anaesthetic has the advantage of not masking the area if an aberrant injection is made.38 The procedure is typically painful to the patient and is associated with the typical risks of a mildly invasive procedure; expectations should be discussed prior to the procedure. Utilization of MR arthrography for specific conditions will be discussed individually throughout the chapter.
Normal anatomy
Osseous structures
Biomechanically, the shoulder is the most complicated articulation in the body. It comprises the glenohumeral, acromioclavicular and sternoclavicular joints, which, together with the articulation between the scapula and the true ribs, form a closed-loop kinematic chain.39–41 The shoulder has multitudinous muscle attachments, supporting ligaments and bursae, many of which demonstrate interrelated comorbidities when the shoulder is affected by internal derangements.5,6 The major advantage of MR imaging, as compared with plain film radiography, is the visualization of these soft tissue structures and their pathoanatomical interrelationships, the most common source of pain when addressing shoulder complaints.2,42
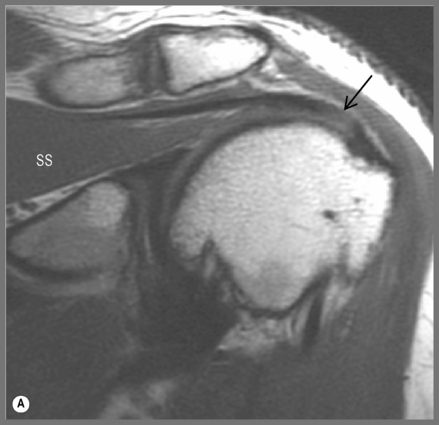
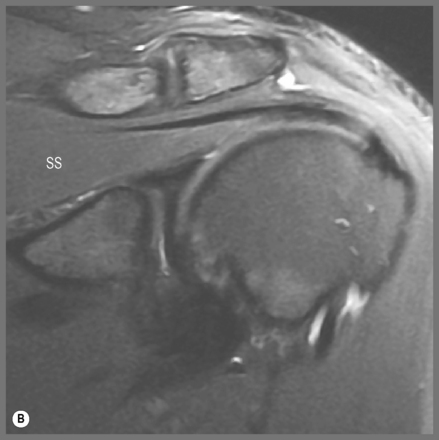
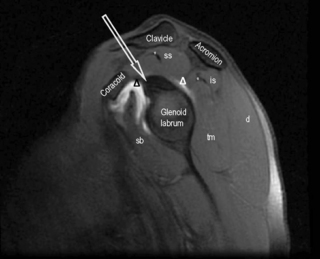
The sternoclavicular joint is a synovial ‘saddle’ joint (sellaris) and represents the only point of contact between the pectoral girdle and axial skeleton.6,41 The glenohumeral joint is a ‘ball and socket’ (spheroidal) synovial joint, allowing three degrees of freedom.6,41 It occurs between the glenoid fossa of the scapula, which is shallow and lined with hyaline cartilage, as is the reciprocal articulating surface of the humeral head. Hyaline cartilage, unlike fibrocartilage, will show up as an area of intermediate signal intensity on both T1- and T2-weighted sequences. The fossa is rimmed by a fibrocartilaginous disc known as the glenoid labrum (Figures 8.03, 8.04), which will show up as a low intensity area on most sequences. Six labral variants have been noted, with more variability in the anterior labrum (Table 8.02).
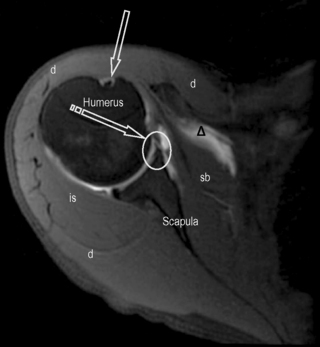
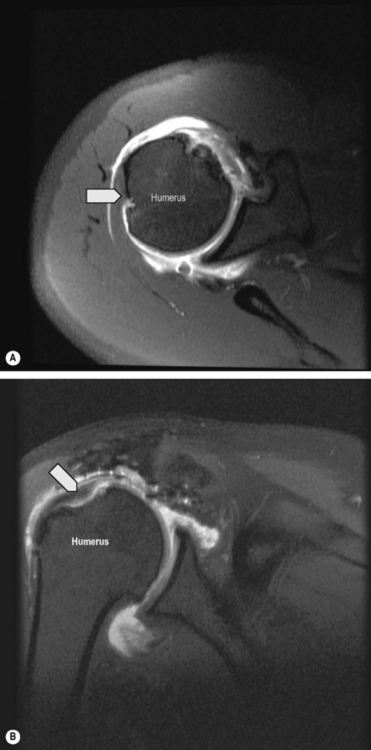
Figure 8.03 • Axial, T2-weighted, fat-suppressed MR image through the mid-portion of the glenohumeral joint, below the supraspinatus muscle. The biceps tendon is well seen, outlined by the fluid-filled synovial sheath (arrow). The subscapularis bursa is visible and identified by the delta symbol ( ). It is of high signal intensity, or fluid-filled, due to its continuity with the articular capsule. Only the subscapularis and infraspinatus bursae should be visualized in a non-inflamed shoulder. A small cleft is visible between the glenoid labrum and the scapula, representing a normal variant, often mistaken for glenoid tears (striped arrow and oval). The key to the legend is detailed in Box 8.01.
). It is of high signal intensity, or fluid-filled, due to its continuity with the articular capsule. Only the subscapularis and infraspinatus bursae should be visualized in a non-inflamed shoulder. A small cleft is visible between the glenoid labrum and the scapula, representing a normal variant, often mistaken for glenoid tears (striped arrow and oval). The key to the legend is detailed in Box 8.01.
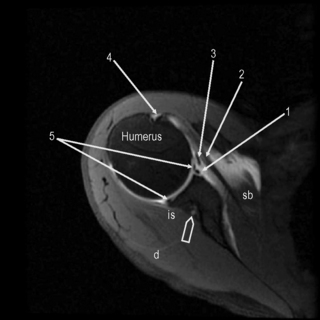
Figure 8.04 • An axial, T2-weighted, fat-suppressed MR image through the glenohumeral joint (slightly superior to Figure 8.03) through the plane of the subscapularis tendon. The suprascapular neurovascular bundle is demonstrated by the arrowhead. 1 = anterior capsular reflection; 2 = subscapularis tendon; 3 = middle glenohumeral ligament; 4 = bicipital tendon and synovial sheath; 5 = anterior and posterior glenoid labrum.
Table 8.02 The glenoid labrum: congenital variants43
| Variant | Frequency anterior | Frequency posterior |
|---|---|---|
| Triangular | 45% | 71% |
| Round | 19% | 12% |
| Cleft | 15% | 0% |
| Notched | 8% | 0% |
| Flat | 7% | 6% |
| Absent | 6% | 8% |
It is important to note these variations so as not to confuse them with pathology and to be aware of the lack of variability in the posterior labrum, where cleaved or notched patterns should raise suspicion of a tear. Of additional note is posterosuperior labral absence, which is considered a normal variant.43 The labrum is the site of the fibrous attachment of the glenohumeral ligaments and the joint capsule to the scapula. In most patients, the hyaline cartilage of the glenoid fossa will extend beneath the labrum, creating an area of increased intensity (referred to by some as undercutting) that may be confused with a tear.25,44,45 Increased signal intensity has been identified in both the posterosuperior and anteroinferior labrum without a tear, owing to the ‘magic angle’ phenomenon.46 It is useful to be aware that posterosuperior labrum tears are more common in athletes involved in throwing and there should be increased clinical suspicion in the physician diagnosing this population.47
The articular capsule extends from the glenoid labrum to the humeral head. Three proximal capsular attachment variants have been described and can occur at the anterior labrum. Type I capsules insert at the tip or base of the labrum, whilst type II insert no more than 1 cm medial to the labrum. Both will appear with approximately the same frequency at the anterior labrum. Type III capsules occur in about 4% of shoulders, insert more than 1 cm medially and are usually indistinguishable from congenital synovial pouches or capsular stripping. If type II or III capsules are found posteriorly, this should raise clinical suspicion of injury.43 The synovial lining of the capsule extends to form a sheath around the proximal aspect of the long head of the biceps muscle.41
The coracohumeral and the three glenohumeral ligaments may be difficult to evaluate separately from the capsule; indeed, they are usually regarded as capsular folds or thickenings.10,24,48,49 Of these, the inferior glenohumeral ligament is the largest and most important; it forms the axillary recess of the capsule. The superior glenohumeral ligament is the smallest and its function is not well understood; in 3–10% of the population, it is congenitally absent.24 In many of these instances, the medial glenohumeral ligament is thickened and cord-like and attaches directly to the superior labrum at the base of the biceps tendon. The combination of the two anomalies is referred to as the Buford complex and has been reported to occur in 1.5% of the population.50
Another variation of the capsular-ligamentous complex is a labrum foramen, a hole in which a small detachment of the anterosuperior corner of the labrum is present; this occurs in 12% of the population.51 In as many as three-quarters of the population, a sublabral recess/sulcus may form between the bicipito-labral complex and the superior portion of the glenoid fossa by a synovial reflection.52 All three of these variants can easily be mistaken for labral tears.
Anatomical variants in bone marrow may be confused with pathologies on MR. On T1-weighted MR sequences, red (haematopoietic) marrow appears as an area of hypointensity, whilst yellow (fatty) marrow appears as an area of hyperintensity. As individuals age, red marrow is converted to yellow marrow, starting distally and moving towards the appendicular skeleton. Adult marrow patterns are typically realized by the age of 18–21 years, although residual red marrow is a common finding. It is important to note that an area of hypointensity, usually visualized as a subcortical curvilinear distribution in the medial humeral head, is a typical location for residual or reconverted marrow.53,54 This should not be mistaken for marrow disease and will occur in the absence of soft tissue mass, cortical destruction or medullary expansion.31 The finding will be relatively symmetrical and imaging of the contralateral shoulder may help with differentiation.
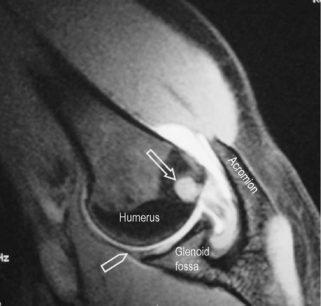
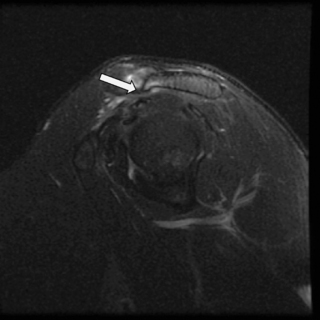
The head of the humerus has a normal anatomical flattening that occurs underneath the path of the teres minor muscle as it inserts on the lateral portion of the humeral head. It is important to differentiate this normal finding from a Hill–Sachs impaction fracture (Figure 8.05). Differentiation on individual axial images cannot be made with confidence by either the size of the indentation or its location in the axial plane. The most accurate way to distinguish the two entities is by their position on the long axis of the humerus. Hill–Sachs lesions will be visible within the superior 5 mm of the humeral head and typically extend up to 18 mm from the top of the humeral head. They should be visible within the first two transaxial sections. In contrast, normal flattening occurs 20 mm or more caudal to the humeral head.55
Whilst it may be possible for lesions to extend further caudally and overlap the normal groove, they can be differentiated by viewing the more cephalic slices. In addition, in a new or recent Hill–Sachs lesion, associated bone marrow oedema will be noted surrounding the depression of the superolateral aspect of the humeral head. Often, the Hill–Sachs lesion is associated with additional lesions, particularly the Bankart lesion (either cartilaginous or osteocartilaginous).56,57
The acromioclavicular joint is regarded as a ‘gliding’ (plane) synovial joint although in reality a number of variations exist that can affect either articular surface, though in a reciprocal manner.41 Acromial morphology was first categorized by Bigliani58 into three shapes:
The last two, non-planar variations are associated with a higher predisposition to degenerative change.59 A fourth acromial configuration, with a convex undersurface, has since been identified60 but it is considered uncommon and no correlation has been made between this shape and impingement.31 The prevalence of each acromial type in the general population and in subjects with painful shoulders remains uncertain.58,61,62
Both joint surfaces are covered by fibrocartilage, sometimes mixed with the hyaline cartilage more typically associated with synovial articulations.41,63 The joint contains a disc, which is highly variable: true discs are relatively rare but, when present, can divide the joint in two; more commonly, the disc is a meniscus, whose fibrocartilage structure can be difficult to differentiate from the articular surfaces of the joint. The disc is frequently degenerate and can be congenitally absent.63,64
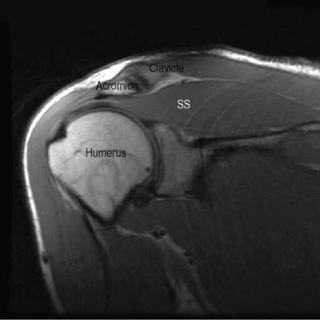
When viewing the acromion in the coronal oblique plane, a common finding is an area of hypointensity projecting inferolaterally from the lateral aspect of the acromion, termed a ‘pseudospur’; this is the normal inferior tendon slip of the deltoid insertion on the acromion and should not be confused with a spur.45 If any doubt exists, correlation with findings on other imaging planes or plain film radiography will be helpful (Figure 8.07).
Muscles
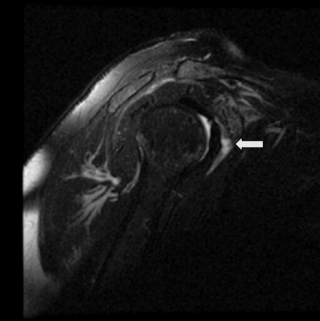
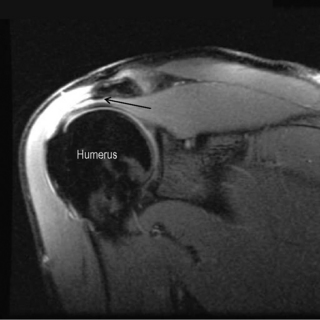
MR imaging also allows for a good assessment of the major muscle groups of the shoulder and their tendons, in particular the rotator cuff group, the biceps and deltoid muscles. Muscle and tendon should appear hypointense on T1- and T2-weighted sequences (Figures 8.03, 8.04, 8.08–8.12; Box 8.01). When observing the supraspinatus tendon on T1-weighted sequences, any areas of increased signal intensity must be correlated with T2-weighted images to avoid misdiagnosis due to the magic angle phenomenon (Figure 8.13).30 This most commonly occurs at the critical zone, where the tendon angles anteriorly and where tendon pathology is most commonly located.45
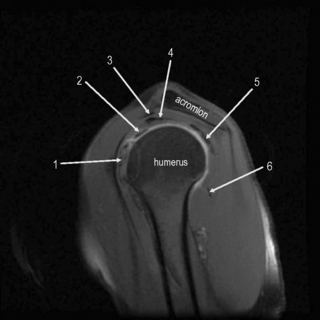
Figure 8.11 • Sagittal oblique, T2-weighted, fat-suppressed MR image through the middle of the humerus, several slices lateral to Figure 8.10. This slice allows for visualization of the tendons of the main muscle groups. These structures are most at risk for impingement, owing to their proximity to the undersurface of the coracoacromial arch. 1 = subscapularis tendon and muscle; 2 = long head of the biceps; 3 = coracoacromial ligament; 4 = supraspinatus tendon; 5 = infraspinatus tendon; 6 = teres minor muscle and tendon.
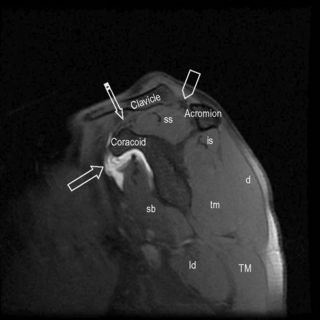
Figure 8.12 • Sagittal oblique, T2-weighted, fat-suppressed MR image though the medial scapula demonstrating the coracoacromial arch and main muscle groups. This image is slightly medial to Figure 8.05. The high intensity zone adjacent to the coracoid process represents the subscapularis bursa (arrow). Note the position of the supraspinatus muscle and tendon, occupying the entire space between the clavicle and scapula. The coracoclavicular ligament is shown by the striped arrow and the acromioclavicular ligament by the arrowhead.
On axial slices, the biceps tendon is well visualized within the bicipital groove; it is maintained there in part by the transverse ligament of the humerus, an expansion of fibres contributed by the subscapularis tendon. Because the biceps tendon sheath communicates with the glenohumeral joint space, a small amount of fluid in the sheath is normal and should be located posterior to the tendon (Figure 8.03). A round, focal fluid collection just lateral to the biceps tendon may also be noted; anatomical studies have identified this as the anterolateral branch of the anterior circumflex humeral vessels, and not fluid collection within the sheath. In normal shoulders, fluid should not encircle the tendon and such a finding indicates tendon injury, inflammation or a glenohumeral joint effusion.45
Bursae
The subscapular bursa is the only bursa communicating directly with the glenohumeral joint and represents an extension of the capsular synovial sheath. Communication occurs mainly between the superior and middle glenohumeral ligaments. It is considered that the purpose of this bursa is to protect the subscapularis tendon as it travels beneath the coracoid process and over the scapular neck.65
The most clinically important bursal structures are the subdeltoid and subacromial bursae. They do not communicate with the joint; however, in most individuals, they are contiguous structures although are variable in size and configuration. Superiorly, the bursae are bordered by the acromion and inferiorly by the rotator cuff muscles and tendons. The medial border stretches medially beyond the acromioclavicular joint, and the lateral portion to the greater tuberosity. Anteriorly, the bursa covers portions of the bicipital groove and posteriorly it lies between the deltoid and rotator cuff muscles. This ensures proper gliding motion between the rotator cuff and coracoacromial arch. Inflammation of these bursae can be related to impingement or rotator cuff diseases.65,66
A subcoracoid bursa is common and does not communicate with the glenohumeral joint but has been reported to communicate with the subdeltoid–subacromial bursa in anywhere from 11% to 55% of subjects.67 Both calcific and non-calcific subcoracoid bursitis is an infrequent cause of isolated anterior shoulder pain.68
The MR imaging appearance of all bursae should be isointense to muscle. If increased signal is observed on T2-weighted sequences, it should be considered a sign of effusion. Fluid should only be observed in the joint space as a fine line between the two articular surfaces, in communicating bursae or surrounding the long head of the biceps tendon. Increased signal intensity in the bursa can be due to a rotator cuff tear, inflammation or inadvertent injection into the bursa on arthrography (Figure 8.14).66

 ).
).