Abstract
The sphenoid bone is located at the central skull base and is commonly considered the most complex bone in the human body. It forms the major boundary between the intra- and extracranial structures and is a conduit for several cranial nerves. The various sphenoid foramina extending to the orbits anteriorly and neck spaces inferiorly are also pathways for transmission of disease.
This chapter highlights the normal sphenoid bone anatomy and various disorders affecting the skull base, including nasopharyngeal carcinoma, infections, and meningioma. An understanding of the sphenoid bone anatomy enables the prediction of intra- and extracranial disease spread and presentation.
Keywords
Central skull base, Cranial nerves, Meningioma, Nasopharyngeal carcinoma, Orbit, Sphenoid bone
The sphenoid bone is located at the central skull base and is commonly considered the most complex bone in the human body. Although the sphenoid bone is often neglected in relation to the adjacent temporal bone, it forms the major boundary between the intra- and extracranial structures. The various sphenoid foramina to the orbits anteriorly and neck spaces inferiorly are pathways for transmission of disease.
This chapter highlights the normal sphenoid bone anatomy and various disorders affecting the skull base. Understanding the anatomy will enable clinicians to predict intra- and extracranial disease spread and presentation.
Normal Anatomy
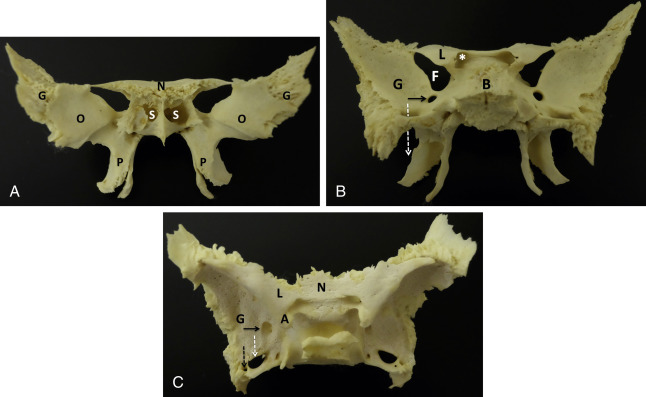
The sphenoid bone forms the central skull base and viewed anteriorly resembles a bird with its wings unfurled. It is a compound bone with a median body and paired lateral greater and lesser wings ( Fig. 3.1 ). At the ventral junction of the body and wings the paired pterygoid processes arise inferiorly, resembling the extended limbs of a bird.
Of interest, the Greek origin of sphenoid (sphen) is likely in reference to a wedge shape seen laterally, with pterygoid (pteron) referring to a fin- or wing-like shape. Another theory for the origin of “sphenoid” is the term os sphecoidale, meaning “bone resembling a wasp.” The term is apt given the resemblance to a winged creature. At some point a transcription error to “sphenoidale” may have occurred with loss of the true meaning.
Anteriorly the sphenoid bone articulates with the ethmoid and frontal bones, laterally with the temporal bones, and posteriorly with the basiocciput. Essentially, the sphenoid functions as an attachment site for the majority of the masticator musculature and serves as a key conduit for the passage of nerves and blood vessels of the head and neck. Major foramina and fissures include the optic canal, foramen rotundum, superior orbital fissure, and foramen ovale ( Figs. 3.2–3.5 ).
Sphenoid Body
The body of the sphenoid contains the sphenoid sinuses and the pituitary fossa (sella turcica), a deep saddle-shaped depression containing the pituitary gland (hypophysis). The anterior margin of the pituitary fossa (tuberculum sellae) continues anteriorly as the flat superior surface of the sphenoid, termed the planum sphenoidale. This forms the anterior roof of the sphenoid sinuses and articulates with the cribriform plate of the ethmoid bone, which transmits small fibers of the olfactory nerve.
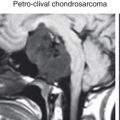
The posterior margin of the pituitary fossa (dorsum sellae) continues inferiorly as the basisphenoid, which articulates with the basiocciput forming the clivus (Latin for “slope”). The clivus continues posteroinferiorly to the foramen magnum, with the petroclival fissures forming the lateral borders. The inferior clivus forms the bony roof of the nasopharynx.
Anteroinferior to the sella turcica are the paired sphenoid sinuses. The thin anterior wall of the sinuses and face of the sphenoid body articulate with the nasal septum at the sphenoidal crest. At either side of the crest are the sphenoid sinus ostia allowing drainage of secretions into the sphenoethmoidal recesses and then into the superior nasal cavity. The lateral borders of the sphenoid bone/sinuses form the medial cavernous sinus walls and are commonly indented by the carotid arteries. The posterior walls of the sinuses are formed by the anterior clivus, which can be of variable thickness, depending on the extent of sinus pneumatization.
Lesser Wing
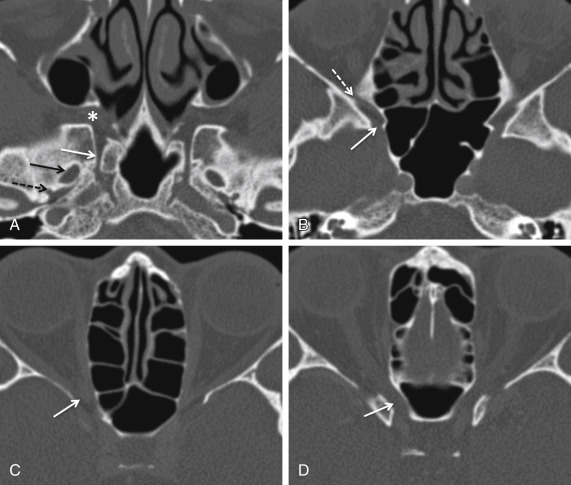
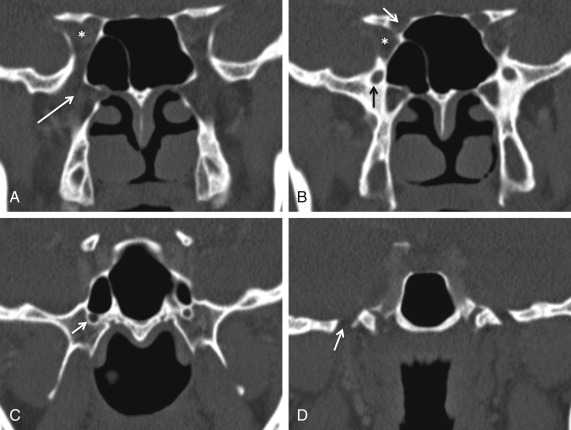
The lesser wings or orbitosphenoids are paired thin triangular plates that extend laterally from the planum sphenoidale. Medially they arise from the anterior and superior sphenoid body at two roots. These roots define the optic canal ( Figs. 3.2–3.5 ), which transmits the optic nerve and ophthalmic artery. It is the only canal passing through the lesser wing and is separated from the superior orbital fissure inferolaterally by the optic strut (lower root).
The superior orbital fissure ( Figs. 3.2–3.5 ) is a comma-shaped gap between the lesser and greater wings of the sphenoid bone appearing thin superolaterally and bulbous inferiorly. It transmits cranial nerves (CNs) III, IV and VI (oculomotor, trochlear, and abducens), branches of the ophthalmic division of the trigeminal nerve (CN V1), and several vessels including the ophthalmic veins. In addition, the annulus of Zinn, common tendinous origin of the four rectus muscles, straddles the superior orbital fissure centrally and encircles the optic canal.
The inferior surface of the lesser wing forms the upper boundary of the superior orbital fissure and the posterior orbital roof. The flat superior surface serves as a platform for the basifrontal lobe and posteromedial extensions form the anterior clinoid processes, which are the attachment sites of the tentorium cerebelli.
Greater Wing
The paired greater sphenoid wings, or alisphenoids, arise from the body of the sphenoid medially and curve superiorly and laterally. The greater wings contribute to the formation of the orbit and middle cranial fossa.
At the orbit, the medial margin of the greater wing forms the inferior margin of the superior orbital fissure and the posterolateral margin of the inferior orbital fissure ( Figs. 3.2 and 3.4 ), which transmits the zygomatic branch of the maxillary nerve (CN V2). The orbital portion of the greater wing also forms the posterolateral wall of the orbit.
The cerebral or superior surface of the greater wing forms the majority of the concave middle cranial fossa and has a number of foramina passing through it.
The foramen rotundum is a circular aperture seen at the base of the greater wing anteromedially, just inferior to the superior orbital fissure ( Figs. 3.2–3.5 ). It transmits the maxillary nerve (CN V2) from the middle cranial fossa to the pterygopalatine fossa.
The foramen ovale arises posterolateral to the rotundum and transmits the mandibular nerve (CN V3) from the middle cranial fossa to the masticator space ( Figs. 3.2–3.5 ). The size of the foramina ovale can differ from side to side. Asymmetry of up to 4 mm can be within normal limits.
The foramen spinosum ( Fig. 3.2 ) is located further posterolateral to the foramen ovale and transmits the middle meningeal artery and a recurrent branch of the mandibular nerve (CN V3). Posterior and medial to the foramen spinosum, each greater wing projects as a triangular process articulating with the squamous and petrous portions of the temporal bone. At the apex of this triangle is the inferiorly projected sphenoid spine (spina angularis). This serves as an attachment site of the tensor veli palatini muscle and the sphenomandibular ligament.
Posteromedially the greater wing forms the anterior margin of the foramen lacerum. This represents another potential conduit of disease spread from the nasopharynx. At the lateral temporal surface of the greater wing the muscles of mastication, including the temporalis (superiorly) and lateral pterygoid (inferiorly), attach.
Pterygoid Processes
The fin-like pterygoid processes extend inferiorly from the junction between the greater wing and body of the sphenoid. Each pterygoid process is formed of two plates, lateral and medial, which fuse superiorly and anteriorly. The site of fusion serves as the posterior wall of the pterygopalatine fossa, which separates the pterygoid processes from the maxillary sinus anteriorly. The pterygopalatine fossa is an important neurovascular crossroad of the head and neck, communicating with numerous foramina, including the inferior orbital fissure, foramen rotundum, and the vidian canal ( Figs. 3.2–3.5 ).
The vidian (pterygoid) canal is a communication through the medial plate of the pterygoid between the foramen lacerum posteriorly and the pterygopalatine fossa anteriorly ( Figs. 3.2–3.5 ). The canal lies inferomedial to the foramen rotundum and their intervening distance depends on the degree of sphenoid sinus pneumatization. The vidian artery, vein, and nerve (formed from the greater superficial petrosal nerve and deep petrosal nerve) pass through the canal.
Posteriorly the lateral and medial processes diverge, and enclosed between them is the V-shaped pterygoid fossa. This contains the tensor veli palatini and medial pterygoid muscles. The lateral pterygoid process serves as the site of origin for the medial and lateral pterygoid muscles of mastication. The tensor veil palatini arises superiorly at the base of the medial pterygoid plate at an oval depression termed the scaphoid fossa. As mentioned previously, the muscle also has an additional attachment site at the scaphoid spine.
Sphenoid Bone Disorders
Sphenoid Sinus
The paired sphenoid sinuses drain into the nasal cavity through the sphenoethmoidal recesses. The sinuses are lined by the respiratory epithelium, which secretes mucus, serving to protect against infection. Underlying the epithelium is the capillary-rich lamina propria, which is firmly attached to the periosteum of the adjacent sphenoid bone.
Compared with CT, MRI appearances of sinonasal secretions show a wide variation. In the normal state, the secretions are almost purely water with up to 5% proteinaceous content. These appear as hyperintense on T2-weighted (T2W) and hypointense on T1-weighted (T1W) images. Once a sinus is obstructed, the water content is reabsorbed with a corresponding increase in the protein content. This results in shortening of the T1W and T2W relaxation times, and at about 25%–30% protein content the secretions may reverse from the normal state, appearing hyperintense on T1W and hypointense on T2W images. At even higher protein contents (35%–40%), the T1W and T2W signals may appear hypointense, similar to any surrounding gas. Knowledge of these appearances is useful in the assessment of mucoceles, which are essentially “mucous tumors” following the same signal characteristics.
Mucoceles are defined as an opacified, expanded sinus resulting from obstruction at the sinus ostium. Mucoceles are most common at the frontal and ethmoid sinuses, with rare occurrences at the sphenoid sinus. They lead to smooth expansion of the bone and when large can impinge on adjacent neurovascular structures. At the sphenoid sinus, the risk of intracranial extension is the greatest, with potential for visual loss and cranial nerve palsies secondary to involvement of the orbital apex and cavernous sinus.
Sphenoid sinusitis is a common condition and mainly results from bacterial infections, although fungal etiologies are also implicated. Fungal infections include aspergillosis, which can produce central hyperdense secretions on CT in the affected sinuses secondary to inspissated mucus and the presence of heavy metals secreted by the fungus. On MRI these hyperdense secretions appear of low signal on T2W images and can mimic air.
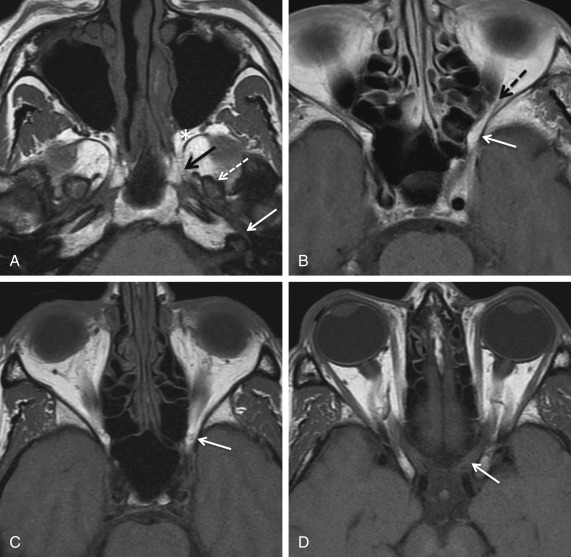
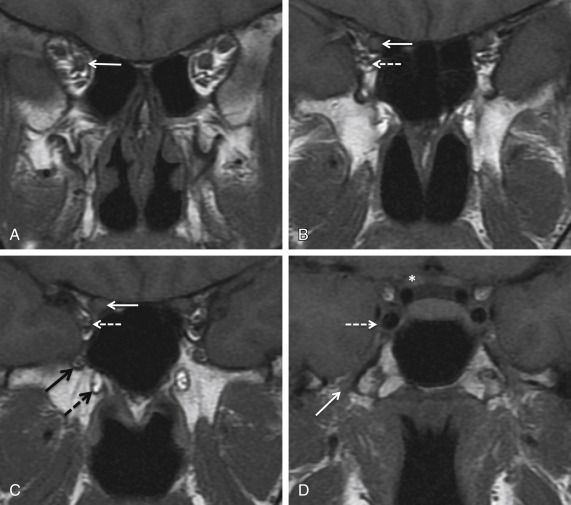
In the immunocompromised (e.g., diabetics) an invasive fungal sinusitis can occur with aggressive bony erosion and invasion of the adjacent cavernous sinuses, orbital apex, and the brain ( Fig. 3.6 ). Patients may present with headache or visual symptoms secondary to involvement of the traversing cranial nerves. Life-threatening vascular injury may also occur with cavernous sinus thrombosis and the development of pseudoaneurysms from the adjacent carotid arteries. Overall mortality is in the range of 50%–80%, although reversal of the predisposing condition, e.g., neutropenia, administration of antifungal therapy, and radical surgical debridement, can reduce mortality by up to 18%.
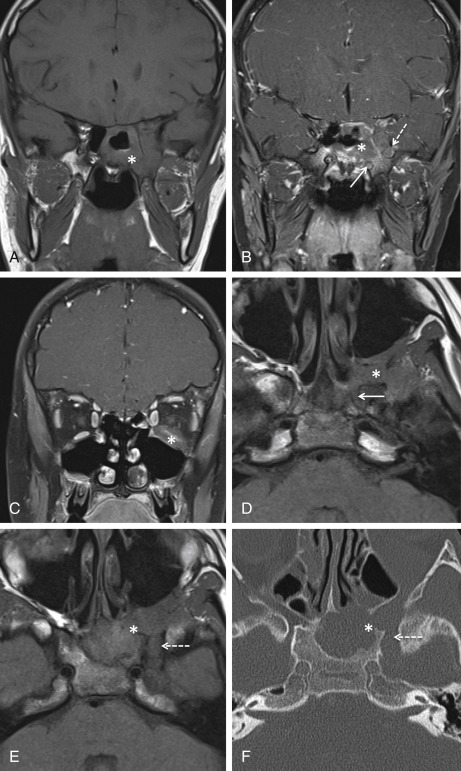
Paranasal sinus malignancies comprise only 0.2% of all malignancies, with 80% occurring in the maxillary sinuses. Primary sphenoid sinus neoplasms are extremely rare, accounting for only 1%–2% of paranasal sinus malignancies. Squamous cell carcinoma, sinonasal undifferentiated carcinoma, and adenoid cystic carcinoma may be encountered. As with infective processes, malignancies commonly present with cranial nerve neuropathies, which is a poor prognostic sign. MRI is useful to delineate the tumor extent from the underlying associated inflammatory changes and to access for intracranial extension. Unfortunately, surgery is rarely curative because of an advanced state of disease at presentation, and aggressive multidisciplinary management, including chemotherapy and radiotherapy, can maximize patient outcomes.
Foraminal Lesions
Orbital apex
The optic canal and superior orbital fissure form the bony orbital apex, which acts as the transition zone for numerous neurovascular structures entering the orbit from the cranium. Lesions at the orbital apex are clinically important, as they can adversely affect vision and lead to ophthalmoplegia. Orbital apex syndrome (Jacod syndrome) is the collective term for cranial nerve deficits associated with a mass lesion at the orbital apex.
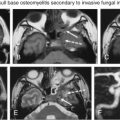
A broad range of lesions can occur at this site. Primary tumors are rare and in children include rhabdomyosarcoma. This lesion can be very large at presentation and leads to extensive bony destruction and intracranial involvement. Meningiomas may arise along the optic nerve sheath with classical tram track calcification on CT, although orbital extension of an intracranial meningioma is more common. Optic gliomas ( Fig. 3.7 ) and nerve sheath tumors such as schwannomas may also occur, with the former having a well-documented association with neurofibromatosis type 1. Optic gliomas occur in up to 30% of patients with neurofibromatosis type 1 and most commonly present in childhood. Primary lymphoma has been noted in this region, but is more commonly seen as part of a secondary generalized process.

Malignant spread to the orbital apex from the posterior nasal cavity and nasopharynx is well documented. This most commonly occurs secondary to nasopharyngeal carcinoma ( Fig. 3.8 ) and salivary gland neoplasms, including adenoid cystic carcinoma, which has a high propensity for perineural involvement (31%–96%). Malignant lesions initially gain access to the pterygopalatine fossa from the nasal cavity via the sphenopalatine foramen. Once at this important neurovascular crossroad, spread through the inferior orbital fissure and involvement of the orbit and orbital apex may occur ( Fig. 3.8 ). Obliteration of the normal fat in the pterygopalatine fossa is the earliest sign of malignant infiltration. This may be seen on both CT and MRI but is best demonstrated on MRI using high-resolution precontrasted axial T1W images.