Venous malformations and hemangiomas of the skeletal muscle are separate entities with different clinical presentation, histology, and imaging findings. Recent advances in the field of vascular anomalies and current efforts in the unification of terminology by the International Society for the Study of Vascular Anomalies are pivotal in understanding and differentiating intramuscular venous malformations and intramuscular capillary-type hemangioma. Fibroadipose vascular anomaly is another recently defined vascular anomaly affecting the skeletal muscle, with a distinct clinical presentation, histology, and imaging appearance. These 3 distinct vascular anomalies are reviewed and their histologic features, clinical presentation, imaging appearance, and treatment are discussed.
Key points
- •
Venous malformations (VM) and hemangiomas of the skeletal muscle are now recognized as 2 separate entities with different clinical presentation, histology, and imaging findings.
- •
Both entities have been lumped together in the literature based on the original description by Allen and Enzinger in 1972.
- •
Recent advances in the field of vascular anomalies and current efforts in the unification of terminology by the International Society for the Study of Vascular Anomalies are pivotal in the understanding and differentiation of these 2 distinct entities: intramuscular VM and intramuscular capillary-type hemangioma.
- •
Fibroadipose vascular anomaly is another recently defined vascular anomaly also affecting the skeletal muscle, particularly the calf muscles, with a distinct clinical presentation, histology, and imaging appearance.
- •
Confined to muscle, these 3 entities are less apparent at birth and more likely to be diagnosed during adolescence and early adulthood.
Introduction
According to the classification by the International Society for the Study of Vascular Anomalies (ISSVA), venous malformations (VMs) are not neoplasms but rather congenital structural anomalies resulting from an error in venous morphogenesis. VMs are categorized as slow-flow type, which also includes capillary and lymphatic malformations. Intramuscular VMs or VMs of the skeletal muscle (IMVMs) are a subset of VM confined to a muscle or muscle group with occasional minimal extension into the adjacent subcutaneous soft tissues. Conversely, hemangiomas are benign neoplasms, and as such undergo mitotic activity and increased endothelial cell turnover.
VMs have been classified by their morphology and drainage pattern on phlebography by Dubois and colleagues and Puig and colleagues , as spongiform, cavitary, or dysmorphic. Spongiform VMs consist of dilated blood-filled spaces with a compact, “masslike” arrangement and little to no in-line normal venous outflow to systemic veins ( Fig. 1 ). In contrast, the phlebectatic VMs are composed of dilated vascular lakes as well as tubular and tortuous veins arranged in a haphazard fashion. Purely IMVMs are mainly of the spongiform type and, therefore, are almost entirely isolated with almost no systemic venous drainage. , This morphologic classification that was originally described to assess the therapeutic outcomes of sclerotherapy is also useful for understanding certain aspects of the pathophysiology and imaging features of IMVMs on various modalities (ie, ultrasound and MR imaging). Due to this predominant spongiform morphology, IMVMs are often misdiagnosed on imaging as either benign or malignant neoplasms and are referred to our vascular anomaly clinic for biopsy.

In the literature, IMVMs have been lumped together with intramuscular hemangioma based on the seminal work by Allen and Enzinger almost 50 years ago. In 2002, Hein and colleagues introduced the term “VM of the skeletal muscle” based on the ISSVA classification. In the same study, the existence of a hemangioma of the skeletal muscle was suggested; a term that was adopted by Yilmaz and colleagues in 2014. An intramuscular capillary–type hemangioma (ICTH) is a true vascular neoplasm with unique imaging features that is considered in the provisionally unclassified category by ISSVA. , The use of different terminology in the literature has made an accurate calculation of IMVM incidence difficult. In a study by Vogel and colleagues that included 115 patients with VMs, 40% were found to be confined to the skeletal muscle. In 2014, Alomari and colleagues coined the term fibroadipose vascular anomaly (FAVA) to describe a new entity characterized by fibrofatty infiltration of the skeletal muscle most commonly in the calf, painful phlebectasia, and focal contracture that more frequently affects adolescent girls and young women. These lesions can potentially be confused with IMVM or even neoplasms and are currently in the provisionally unclassified category by ISSVA.
In this article, these 3 distinct vascular anomalies involving skeletal muscle, based on the terminology proposed by ISSVA, are reviewed, and their histologic features, clinical presentation, imaging appearance, and treatment are discussed for general radiologists.
Intramuscular venous malformations
IMVMs, like all VMs, exhibit a normal rate of endothelial cell turnover and do not involute but instead grow proportional to the patient. The suffix “oma” implies cellular proliferation and neoplasia; hence, the term hemangi“oma” of the skeletal muscle, which is commonly used in the literature to refer to IMVMs, should be avoided. , , Despite the effort pioneered by Mulliken and Glowasky, the loose and imprecise use of terminology in the medical literature still poses a challenge with regard to vascular anomalies, and IMVMs are not spared. ,
In accordance with the article by Hein and colleagues published in 2002 and adhering to the ISSVA classification, it is now felt that the large vessel hemangioma–type lesions described by Allen and Enzinger in 1972 represent IMVMs.
Histologic Appearance
Because IMVMs are low-flow vascular malformations, they appear clearly benign histologically. IMVMs are composed of a conglomerate of thin- to thick-walled vessels with variable amounts of smooth muscle and large gaping spaces that lack proliferative features infiltrating the skeletal muscle ( Fig. 2 ). The nuclei of the endothelial cells are flattened and small with no mitotic figures. Intravascular thrombi at various stages and hemosiderin deposition are common, a typical feature of all VMs ( Fig. 3 ). Fibroblastic proliferation with the concentric deposition of collagen and calcifications forming phleboliths are also seen ( Fig. 4 ). Fatty elements are almost always present and frequently abundant. , The endothelium of vessels in IMVMs is immuno-reactive to vascular markers, such as CD31 ( Fig. 5 ), CD34, and von Willebrand factor, but it is nonreactive to the glucose transporter protein (GLUT1), a marker associated with infantile hemangiomas, and D2-40, a marker associated with lymphatic vessels and lymphatic malformations. ,




By definition, VMs should not have cellular proliferation or mitosis unless perturbed. However, VMs can exhibit cellular proliferation in the form of intravascular papillary endothelial hyperplasia (also known as Masson phenomenon), complicating the distinction between neoplasm and malformation. Masson phenomenon is a reactive condition to thrombosis or trauma that represents an exuberant organization and recanalization of a thrombus ( Fig. 6 A). Masson phenomenon is confined to the vascular spaces and is characterized by multiple papillary structures covered by a single layer of flattened endothelium around cores of fibrous connective tissue. Thrombi of various stages of organization are nearly always present ( Fig. 6 B). Masson phenomenon has a striking similarity to the very rare angiosarcoma histologically and could potentially prompt a biopsy to the unfamiliar eye. Masson phenomenon is exclusively intravascular, whereas angiosarcoma is rarely confined to a vascular lumen. Masson phenomenon can be seen as a reactive change inside a preexisting vascular lesion, most frequently in a venous malformation and especially if the location is intramuscular.

Clinical Presentation
Most IMVMs are diagnosed in the first 3 decades, with most lesions discovered at birth. , , A female predominance has been reported with a female:male ratio of 2:1. , IMVMs have a wide anatomic distribution throughout the body, potentially involving any muscle. The head and neck were found to be the most common locations in the studies by Vogel and colleagues and Hein and colleagues. In the study by Hein and colleagues, the orbicularis oris and masseter were the most frequently involved muscles. A lower-extremity predominance was found by Allen and Enzinger, Wild and colleagues, and Wu and colleagues, with the most commonly involved muscle being the quadriceps. Based on the personal experience at our Vascular Anomaly Clinic, most IMVMs affect the lower extremities.
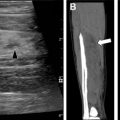
The most common symptoms associated with IMVMs are the presence of a mass ( Fig. 7 ); pain due to thrombosis; or intermittent, localized swelling, or muscle hypoplasia. IMVMs are more likely to present as a mass because of the predominant spongiform morphology and are more likely to be painful and to interfere more with physical activity than the superficial counterparts do. , , ,

A higher percentage of IMVMs are diagnosed later in life compared with the superficial counterpart. This late diagnosis of IMVMs is probably multifactorial. IMVMs are confined to a muscle or muscle group, lacking the skin discoloration of their superficial counterpart and therefore are less apparent on physical examination at an early age (see Fig. 7 ). In the study by Hein and colleagues, only 68% of IMVMs were diagnosed at birth, with the average age at presentation being 13 years. In a later study, Vogel and colleagues also found that when compared with VMs limited to the skin and subcutis, those restricted to the muscle compartment were less likely to present at birth (27% vs 53%) with a mean age of presentation of 6.7 ± 0.9 years. These results are echoed by the experience at our Vascular Anomaly Clinic. Furthermore, due to their location, IMVMs are subjected to additional compressive forces exerted by the surrounding muscle acting similarly to a compressive stocking, which may delay the development of symptoms.
Another reason for a potential late diagnosis of IMVMs is the hormonal influence on these lesions during puberty. IMVMs, like any other vascular malformation, grow proportionate to the patient and never involute. The pubertal hormonal surge causes a temporary accelerated growth of these spongiform lesions, making them more apparent and causing potential confusion with a soft tissue sarcoma. Likewise, the pubertal surge in estrogens, due to a prothrombotic effect, may trigger pain, thus bringing attention to deeply seated lesions. ,
IMVMs can also present with symptoms related to localized intravascular coagulopathy (LIC), such as thrombosis, hemorrhage, or thromboembolic events. The pathophysiology of LIC is explained by the stagnation of blood that occurs in these low-flow vascular malformations, causing the activation of the coagulation cascade, the consumption of coagulation factors, the generation of thrombin, and fibrin with the elevation of D-dimers and hypofibrogenemia that may progress to disseminated intravascular coagulopathy. The spongiform IMVMs are more associated with LIC than the other morphologic types due to the greater lesion capacitance, slower flow, and more blood isolation due to the fewer or no systemic venous connections. , , Therefore, spongiform VMs, especially in an intramuscular location, tend to develop painful intralesional thrombotic episodes that eventually lead to phlebolith formation. ,
Imaging Approach
The 2 main imaging modalities used to evaluate IMVMs (as well as ICTH and FAVA) are ultrasound and MR imaging, which are complementary and therefore usually used in conjunction. Each has its own advantages; however, neither modality uses ionizing radiation.
As most IMVMs are of the spongiform type, they tend to present as masses for which ultrasound is usually the initial imaging modality for their evaluation in the pediatric population. Ultrasound confirms the presence of a mass and characterizes the location (superficial vs deep), the nature of the lesion (cystic vs solid), and the vascularity. On the other hand, MR imaging is helpful in evaluating the extension of the lesion, the pattern of enhancement, and the relationship with adjacent vital structures, such as the neurovascular bundle. The MR imaging protocol must include T1-weighted images without fat suppression, fluid-sensitive sequences, either short-T1 inversion recovery or T2-weighted images with fat suppression, and T1-weighted images with fat suppression before and after intravenous contrast. Early and delayed postcontrast images are critical for assessing the characteristic slow yet progressive enhancement of the lesion ( Table 1 ). The initial MR imaging evaluation should include a dynamic contrast-enhanced MR arteriogram to exclude arterial supply to the lesion commonly seen in neoplasms but absent in IMVMs. Different from malignant neoplasms, IMVMs enhance on the delayed venous phases rather than on the early arterial phases (see Table 1 ). In younger, less cooperative children, MR imaging usually requires sedation to avoid motion artifact.
| STIR | Coronal |
|
| T1 | Axial or coronal |
|
| STIR/T2 FS | Axial |
|
| Precontrast T1 FS | Axial |
|
| Contrast enhaned MRA | Coronal |
|
| Early post contrast T1 FS | Axial |
|
| Delay post contrast T1 FS | Coronal or Sagittal |
|
| Extra delayed postcontrast T1 FS | Axial |
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree