Thyroid Cancer
Todd M. Blodgett, MD
Alex Ryan, MD
Marios Papachristou, MD
Key Facts
Terminology
Well-differentiated thyroid cancer (WDTC)
Medullary thyroid carcinoma (MTC)
Anaplastic thyroid carcinoma
Imaging Findings
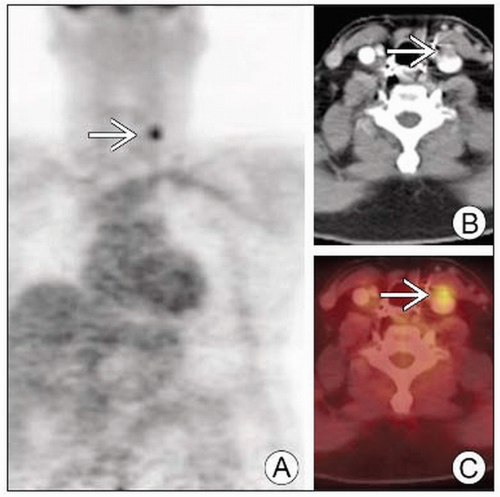
WDTC: Focal asymmetrically increased uptake on FDG PET (not due to normal structure or inflammatory condition)
MTC: Solid lesions in thyroid gland with nodal metastases; ± calcifications
I-123 or I-131 whole body scan when tumor is iodine avid
FDG PET scan for non-iodine-avid tumor
Considerations for IV contrast for PET/CT; need to know if patient will be treated with radioactive iodine
Top Differential Diagnoses
Benign Thyroid Conditions
Other Cancers of Head and Neck
Normal/Benign Extrathyroidal Structures
Multinodular Goiter (MNG)
Follicular Adenoma
Reactive Lymph Nodes
Thyroid Non-Hodgkin Lymphoma (NHL)
Diagnostic Checklist
Perform FDG PET and PET/CT in all patients with
History of WDTC
Status post thyroidectomy
Negative I-131 study
Rising thyroglobulin
FDG uptake may be modest (SUV 2-3) in recurrent/residual thyroid cancer
TERMINOLOGY
Abbreviations and Synonyms
Well-differentiated thyroid cancer (WDTC)
Medullary thyroid carcinoma (MTC)
Anaplastic thyroid carcinoma
Definitions
WDTC: Carcinoma of the thyroid arising from papillary &/or follicular cell origin
MTC: Uncommon malignant neuroendocrine neoplasm arising from thyroid parafollicular “C cells”
Anaplastic: Aggressive form of mostly undifferentiated cells
IMAGING FINDINGS
General Features
Best diagnostic clue
WDTC
Non-physiologic, focal, asymmetric uptake of FDG
However, many WDTC may not be FDG avid when iodine avid
MTC
Solid, low attenuating, discrete thyroid masses with punctate calcification and nodal mets
Anaplastic
Diffuse, intense FDG activity correlating with an infiltrative thyroid mass
Location
WDTC
Primary and recurrent disease arise mostly in the parenchyma and bed of the thyroid gland
Metastatic disease travels to cervical/mediastinal lymph nodes and then to bone, lungs, and mediastinum
Papillary: Lymphatic invasion and spread to multifocal nodal regions
Follicular: Hematogenous spread to lung and bone
MTC
Intraglandular
Often multifocal and bilateral (2/3 sporadic, almost 100% familial)
Lymph nodes: Level VI and superior mediastinal; also retropharyngeal and levels III & IV
Anaplastic
Size
WDTC
Often diffuse microscopic disease
Lymph node and pulmonary metastases may be below limits of detection
Metastases to bone, in contrast, may grow very large
MTC
Up to 2.5 cm
Anaplastic
Bulky
Morphology
WDTC
Typical lymph node findings of roundedness and calcification may be absent
Differentiate from typical thymus morphology (variable by age)
Skeletal metastases typically lytic
MTC
Solid, nonencapsulated mass
Calcification in larger tumors
May be infiltrative in familial forms
Imaging Recommendations
Best imaging tool
Ultrasound for initial evaluation of all thyroid masses with fine needle aspiration
WDTC
For iodine-avid disease: Diagnosis, staging, and follow-up best performed with I-123 or I-131 whole body scan
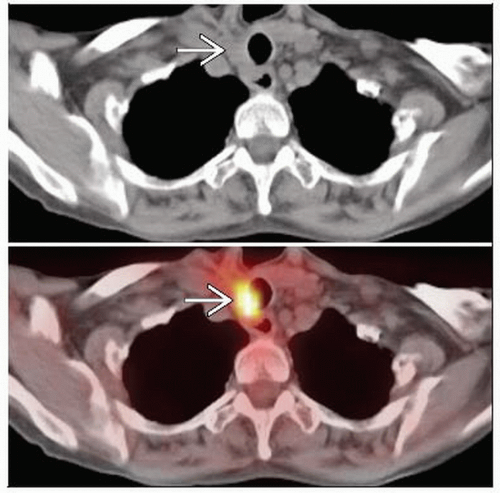
For non-iodine-avid tumor, FDG PET/CT is superior
MTC
Consider FDG PET/CT for staging and restaging
Current insurance coverage restrictions for MTC
Anaplastic
Most are intensely FDG avid, but there are current insurance coverage limitations
Protocol advice
General
Iodine scan: Withdrawal or thyrogen-stimulated
Mediastinal lymph nodes near heart may be blurred due to motion, leading to false negatives
FDG PET
Thyroid-stimulating hormone (TSH) elevation/administration improves performance
Considerations for IV contrast for PET/CT; need to know if patient will be treated with radioactive iodine
Increased thyrocyte metabolism, glucose transport, hexokinase I levels, and overall glycolysis contribute to specific FDG uptake
Hormone withdrawal and administration of recombinant TSH (rhTSH = thyrogen)
Thyrogen dosage schedule not established, but Medicare pays for two injections
Recommended dosing: 0.9 g IM on day 1 and day 2, and FDG PET on day 3, 4, or 5
Correlative tests
Thyroglobulin measurement also best with elevated TSH
Serum thyroglobulin (Tg)
Correlate with radioiodine scan
Insensitive in presence of anti-Tg antibodies
Elevated levels post-therapy indicate residual thyroid tissue (> 2.0 ng/mL)
CT Findings
WDTC
Normal thyroid findings include
Cystic changes (hypodense)
Calcifications (hyperdense)
Well-defined borders
Primary tumor
Typically highly variable morphology
May mimic normal gland
Low attenuation nodule within gland
May have dystrophic calcifications
Signs of more aggressive tumor
Large size
Diffuse infiltration
Ill-defined, heterogeneous morphology
Extension to surrounding tissues
Lymph node appearance also highly variable
Large to small (may appear as benign reactive nodes)
Solid to heterogeneous/hemorrhagic to cystic
Variable calcification
Isolated retropharyngeal nodal metastasis may occur
MTC
Solid, low density, well-circumscribed mass in thyroid
Multifocality more common in familial types
Calcification in tumor and involved lymph nodes may be fine and punctate
Bone metastases typically lytic
Anaplastic
Large infiltrative mass
Nuclear Medicine Findings
WDTC
No current indication for pre-operative PET or PET/CT staging of WDTC
Consider in patients with anaplastic thyroid carcinoma for staging, although not covered by Medicare
Currently covered by Medicare for patients with
Documented history of follicular origin WDTC
Status post-thyroidectomy
Radioactive I-131 therapy
Current elevation in serum thyroglobulin
Negative I-131 whole-body scan
Consider performing FDG PET or PET/CT in all patients with these parameters
WDTC normally demonstrates mild to moderate FDG uptake (mean SUV ˜ 2.5 at 60 min)
When iodine avid, may not have any FDG uptake
Elevated TSH may result in double the SUV of WDTC vs. suppressed state
Best with stimulated thyroglobulin > 10 mU/L
Invaluable for identifying recurrence and metastases in soft tissue, lymph nodes, liver, lungs, and bone
Many of these lesions not visible or detected prospectively by CT
FDG PET can follow a negative I-131 or I-123 whole-body scan in patients with elevated thyroglobulin (Tg)
15-20% of patients with WDTC and high serum thyroglobulin have negative diagnostic I-131 whole-body scans
I-131 or I-123 whole-body scan should be performed prior to injection of FDG if both scans are performed on same day
Small deposits may produce false negatives on I-131 scan
Metastases tend to become more aggressive and FDG avid as they dedifferentiate and lose ability to concentrate I-131
15% of these patients have persistent, recurrent, or metastatic disease
Generally 75% or better sensitivities for local recurrences and distant metastases
PET/CT imaging has diagnostic value regardless of thyroglobulin level
Use of TSH to increase uptake by thyroid tissue is controversial, but has been shown to be effective in some studies
Non-iodine-avid recurrence: FDG PET may help identify areas amenable to surgical removal
MTC
MTC has low avidity for iodine, making radioiodine imaging and therapy ineffective
FDG PET effective for detection of disease
FDG PET improves detection of suspected recurrent disease undetectable by CT/MR
Elevated tumor markers, but no gross disease on cross-sectional imaging
Sensitivity 70-100%, specificity 79-90%
Poorer sensitivity for liver and lung foci, especially when < 1 cm
Controversy exists as to whether PET can reliably assess recurrent, persistent MTC
May be significant overlap of serum calcitonin levels between positive and negative FDG PET scans
Elevated calcitonin not specific; can be elevated in conditions such as CRI
I-123-PET/CT combined with FDG PET/CT allows localization of both foci of highly specific I-123 uptake and iodine-negative tumors
Other Modality Findings
I-123 or I-131 whole-body scan
Tumors may become less well differentiated and lose iodine avidity
Whole-body scan may appear normal despite extensive metastatic disease
I-123 scans miss metastases in bone, lungs, and lymph nodes
I-131 scintigraphy and serial thyroglobulin measurements
Used after near/total thyroidectomy and ablation
Standard method to detect differentiated thyroid cancer recurrence
Thyroglobulin threshold of 10 ng/mL commonly used as cutoff for suspicion of recurrence
Anti-thyroglobulin antibodies may lead to falsely low levels of measured serum thyroglobulin
Surveillance imaging following I-131 typically performed with high resolution US
FNA can be performed at time of exam
FDG PET for suspicion of recurrence in sites inaccessible by US
DIFFERENTIAL DIAGNOSIS
Benign Thyroid Conditions
50% of FDG-avid nodules are benign (usually follicular adenoma [FA])
FA: Solitary mass without adenopathy or evidence of invasion
Incidentally identified FDG-avid nodules should be biopsied, as 50% are malignant
Multinodular goiter: Diffusely enlarged gland with multiple nodules and coarse calcifications
Thyroid Non-Hodgkin Lymphoma (NHL)
Infiltrating mass associated with diffuse enlargement of gland
Calcification in mass or LN rare
Parathyroid Adenoma
May present with similar features to thyroid carcinoma on FDG PET
Usually extrathyroidal
Other Cancers of Head and Neck
Anaplastic thyroid cancer
Thyroid lymphoma
Squamous cell carcinoma
Neuroendocrine tumors
Metastatic disease
Normal/Benign Extrathyroidal Structures
Asymmetrical muscle uptake
Minimize activity and agitation (benzodiazepine useful)
Reschedule examination in hyperglycemic patients (> 200 mg/dL)
Provide comfortable support of head/neck
Vocal cords and cricoarytenoids
Minimize talking, activity, and agitation during FDG uptake period
Unilateral vocal cord paralysis (surgery, invasion) can cause asymmetric uptake
Tonsillar and adenoid tissue
FDG uptake observed due to inflammatory activity
Obtain careful history of recent illness and allergies
Reactive lymph nodes
Correlate with presence of enhanced tonsillar FDG uptake, recent illness
Salivary glands
Treatment with I-131 may lead to asymmetric salivary gland uptake
Accessory sites of salivary tissue may be difficult to distinguish from lymph nodes
Cervical spine arthritis
Due to degeneration or rheumatic disease
Focal uptake in facet joints may mimic metastatic disease
Tracheostomy sites
PATHOLOGY
General Features
General path comments
WDTC
Follicular thyroid cancer characterized by purely follicular or trabecular growth without papillary structures
Has fibrous capsule, known to invade blood vessels (differentiating it from adenoma)
Lymphatic spread less common but distant metastases more frequent
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree