Tissue Harmonic Imaging
Technical Aspects
Fundamental frequency is the original frequency of the acoustic beam emitted from the transducer. Harmonic wave generation is an acoustic phenomenon. Harmonic waves are integer multiples of the fundamental frequency.
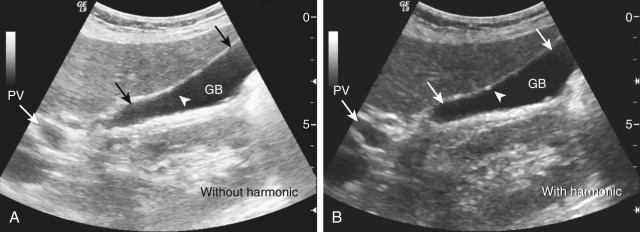
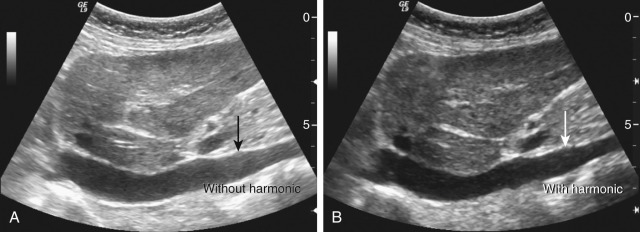
The second harmonic (twice the fundamental frequency) is currently used for tissue harmonic imaging (THI). With THI, the fundamental frequency is eliminated with image processing techniques. THI advantages include improved signal-to-noise ratio and artifact reduction.
Clinical Applications
THI improves image quality and conspicuity, and has been shown to be useful in multiple clinical scenarios, including (1) obesity, (2) hollow structures (e.g., cysts, gallbladder, urinary bladder) ( Figure 4-1 ), and (3) the deep-seated major vessels (inferior vena cava [IVC] and abdominal aorta) ( Figure 4-2 ).
Doppler Ultrasound Imaging
Doppler ultrasonography is a noninvasive technique that provides information about the condition of blood vessels and blood flow direction. It also measures flow velocity and can be used to evaluate the vascularity of mass lesions. Color and pulsed-wave Doppler imaging provide complementary information, including spatial orientation and a time velocity spectrum, respectively.
Technical Aspects
Doppler examination requires five technical parameters (5 Ps), as follows:
- •
Patient preparation: Fasting is required for a Doppler examination of the abdomen.
- •
Probes: Commonly used probes are the (1) curvilinear-array probes (low frequency, 3 to 5 MHz), (2) phased-array probes (low frequency, 2 MHz), and (3) linear-array probes (high frequency, 4 to 10 MHz).
- •
Person: The sonographer should have a considerable amount of expertise to perform a Doppler examination such as understanding of the normal anatomy, pathophysiology, and signature patterns of abdominal vessels.
- •
Picture quality (machine): To obtain good picture quality, the radiologist should consider the following operational parameters: (1) an appropriate anatomic window, (2) depth of field, (3) frame rate, (4) flow sensitivity with adjusted gain settings, (5) image vessel of interest at a Doppler angle of 30 to 60 degrees, and (6) low wall filter settings (if these are high, significant velocity information can be lost). The recorded color flow should occupy the full anteroposterior diameter or cross-sectional area of the vessel without color flow aliasing and noise in the surrounding tissues.
- •
Positioning: The various positions required for imaging every individual vessel.
Pros and Cons of Doppler Imaging
Pros
- •
Noninvasive
- •
Readily available and cost-effective
- •
Portability: Can be done by the bedside in sick or debilitated patients
- •
Differentiating vascular and nonvascular structures (e.g., porta hepatis) ( Figure 4-3 )
Figure 4-3
Transverse Doppler imaging centered at midclavicular line reveals multiple collateral vessels in the porta hepatis that mimic dilated intrahepatic biliary radicles.
- •
Provides information about the patency of blood vessels, direction of flow turbulence, phasicity, jet, impedance, and so on
- •
Quantification of stenosis and direct measurement of flow lumen reduction
- •
Tissue characterization of tumors
Cons
- •
Operator dependency.
- •
Doppler imaging is technically difficult to perform in obese patients and in those with overlying bowel gas or a distended abdomen, especially when desiring visualization of the mesenteric vessels, the portosplenic confluence, or renal artery origin; performing portosystemic collateral mapping; evaluating a shunt anastomosis; and so on.
- •
Good spectral analysis cannot be achieved in patients who cannot hold their breath (e.g., acutely ill patients).
- •
Graft surveillance at the level of the distal abdominal aorta and iliac arteries is difficult.
- •
Abdominal aortic calcifications can be an obstacle in visualization of renal artery origin.
Normal Anatomy of Abdominal Vessels
The normal appearance and signature pattern of abdominal vessels—the portal vein ( Figure 4-4 ), hepatic vessels, mesenteric vessels ( Figures 4-5, 4-6, and 4-7 ), renal vessels ( Figure 4-8 ), abdominal aorta ( Figure 4-9 ), and IVC—are summarized in ( Table 4-1 ). Portosystemic collateral vessels ( Figures 4-10 ) and splenorenal collateral vessels ( Figure 4-11 ) are explained in detail in Table 4-2 .
| Vessel | Identification | Normal Signature Pattern |
|---|---|---|
| Portal vein: normal caliber = 13 mm (quiet respiration) |
|
|
| Hepatic vein: normal caliber = 3 mm (measured 2 cm from inferior vena cava) |
|
|
| Hepatic artery: normal velocity = 30-60 cm/s | Vascular structure anterior to portal vein | Low-resistance flow with spectral broadening |
| Inferior vena cava: normal caliber = 2.5 cm |
|
|
| Abdominal aorta: Normal caliber = 2.3 cm (men), 1.9 cm (women) | Hypoechoic tubular pulsatile structure with echogenic walls best seen by longitudinal midline approach | High-resistance waveform pattern with a brief period of reversed flow (see Figure 4-9 ) |
| Mesenteric vessels: normal caliber <10 mm | Superior mesenteric artery is surrounded by a triangular mantle of fat. It is to the right of the superior mesenteric vein, which runs parallel to the superior mesenteric artery (see Figures 4-6 and 4-7 ) |
|
| Celiac artery | Best visualized in transverse plane, in which the T -shaped bifurcation of vessel into hepatic and splenic artery is characteristic | Low-resistance type of waveform |
| Renal artery and vein | Origin of artery is slightly caudad to superior mesenteric artery and best seen by transverse midline approach. Left renal vein is seen between superior mesenteric artery and aorta. Right renal vein can be traced from inferior vena cava |
|
| Site | Portosystemic | Appearance |
|---|---|---|
| Gastroesophageal junction. Normal coronary vein diameter <6 mm | Between coronary/short gastric veins and systemic esophageal veins | Coronary veins >7 mm are abnormal. Prominent cephalad-directed vessel arising from portal vein opposite superior mesenteric vein |
| Paraumblical vein (falciform ligament) Normal = 2 mm hepatopedal flow | Between left portal vein and systemic epigastric veins near umbilicus | Solitary vein originating from left portal vein courses inferiorly through falciform ligament and anterior abdominal wall to umbilicus, demonstrating hepatofugal flow |
| Gastroepiploic (see Figure 4-6 ) | Between gastroepiploic and esophageal/paraesophageal veins | Cephalad directed vessel along the inferior border of the left lobe |
| Splenorenal and gastrorenal (splenic and renal hilum) | Between splenic, coronary, short gastric, and left adrenal or renal veins | Splenorenal (see Figure 4-11 ). Tortuous, inferiorly directed vessels between spleen and upper pole of left kidney |
| Intestinal | Veins of ascending/descending colon, duodenum, pancreas, liver anastomosis with renal, phrenic and lumbar veins (systemic tributaries) | Collateral pathways identification on ultrasonography depends on the amount of air in the bowel at the time of study |
| Hemorrhoidal (perianal region) | Superior rectal vein anastomoses with systemic middle and inferior rectal veins | Rectal/pararectal varices can be detected with transvaginal or transrectal ultrasonography, cannot be visualized on transabdominal ultrasonography |
Doppler Ultrasound Imaging
Doppler ultrasonography is a noninvasive technique that provides information about the condition of blood vessels and blood flow direction. It also measures flow velocity and can be used to evaluate the vascularity of mass lesions. Color and pulsed-wave Doppler imaging provide complementary information, including spatial orientation and a time velocity spectrum, respectively.
Technical Aspects
Doppler examination requires five technical parameters (5 Ps), as follows:
- •
Patient preparation: Fasting is required for a Doppler examination of the abdomen.
- •
Probes: Commonly used probes are the (1) curvilinear-array probes (low frequency, 3 to 5 MHz), (2) phased-array probes (low frequency, 2 MHz), and (3) linear-array probes (high frequency, 4 to 10 MHz).
- •
Person: The sonographer should have a considerable amount of expertise to perform a Doppler examination such as understanding of the normal anatomy, pathophysiology, and signature patterns of abdominal vessels.
- •
Picture quality (machine): To obtain good picture quality, the radiologist should consider the following operational parameters: (1) an appropriate anatomic window, (2) depth of field, (3) frame rate, (4) flow sensitivity with adjusted gain settings, (5) image vessel of interest at a Doppler angle of 30 to 60 degrees, and (6) low wall filter settings (if these are high, significant velocity information can be lost). The recorded color flow should occupy the full anteroposterior diameter or cross-sectional area of the vessel without color flow aliasing and noise in the surrounding tissues.
- •
Positioning: The various positions required for imaging every individual vessel.
Pros and Cons of Doppler Imaging
Pros
- •
Noninvasive
- •
Readily available and cost-effective
- •
Portability: Can be done by the bedside in sick or debilitated patients
- •
Differentiating vascular and nonvascular structures (e.g., porta hepatis) ( Figure 4-3 )
Figure 4-3
Transverse Doppler imaging centered at midclavicular line reveals multiple collateral vessels in the porta hepatis that mimic dilated intrahepatic biliary radicles.
- •
Provides information about the patency of blood vessels, direction of flow turbulence, phasicity, jet, impedance, and so on
- •
Quantification of stenosis and direct measurement of flow lumen reduction
- •
Tissue characterization of tumors
Cons
- •
Operator dependency.
- •
Doppler imaging is technically difficult to perform in obese patients and in those with overlying bowel gas or a distended abdomen, especially when desiring visualization of the mesenteric vessels, the portosplenic confluence, or renal artery origin; performing portosystemic collateral mapping; evaluating a shunt anastomosis; and so on.
- •
Good spectral analysis cannot be achieved in patients who cannot hold their breath (e.g., acutely ill patients).
- •
Graft surveillance at the level of the distal abdominal aorta and iliac arteries is difficult.
- •
Abdominal aortic calcifications can be an obstacle in visualization of renal artery origin.
Normal Anatomy of Abdominal Vessels
The normal appearance and signature pattern of abdominal vessels—the portal vein ( Figure 4-4 ), hepatic vessels, mesenteric vessels ( Figures 4-5, 4-6, and 4-7 ), renal vessels ( Figure 4-8 ), abdominal aorta ( Figure 4-9 ), and IVC—are summarized in ( Table 4-1 ). Portosystemic collateral vessels ( Figures 4-10 ) and splenorenal collateral vessels ( Figure 4-11 ) are explained in detail in Table 4-2 .