Fig. 9a.1
Illustration of optimal ECG recordings. A clear R-wave and sinus rhythm are essential for reconstruction of the image data. Here, the red dot indicates identification of the R-wave. An incorrect R-wave can be removed by clicking on the red dot (ECG editing). In patients with arrhythmia, it may be helpful to add “virtual R-waves” by clicking on additional red dots or to remove incorrectly identified R-waves. The goal is to obtain a highly regular ECG in order to minimize image artifacts
9.1.2 Defining the Scan Range
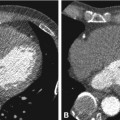
A low-dose planning scan (scanogram with 50 mA) is obtained on the Aquilion 64, Toshiba’s 64-row CT, to define the start and end of the spiral scan, identify the widest dimension of the heart, and place the SureStart (Figs. 9a.2, 9a.3, and 9a.4). The start position is placed just above the origins of the coronary arteries, using the left atrial appendage for orientation. The scan ends just below the heart, and can be stopped manually. The SureStart is placed at the start of the spiral scan, by positioning the active line exactly over the upper boundary of the scan as illustrated in Fig. 9a.2. The SureStart should not contain the coronary arteries or be placed too high (Fig. 9a.4). Careful planning of the scan is essential for achieving an optimal result while minimizing radiation exposure.
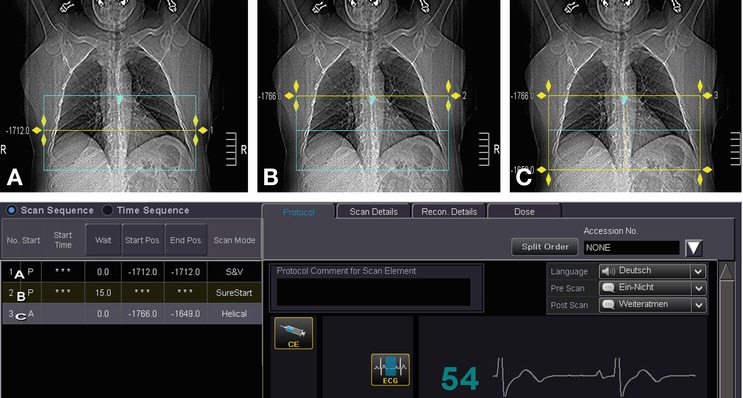
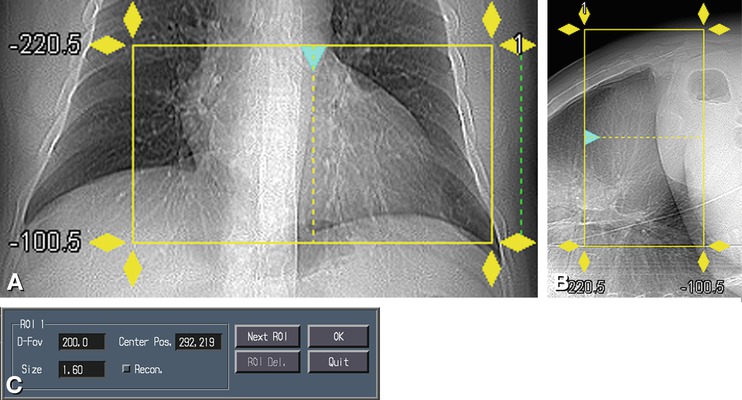
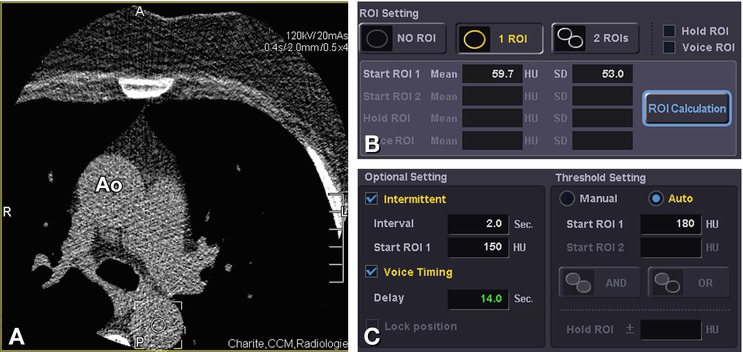
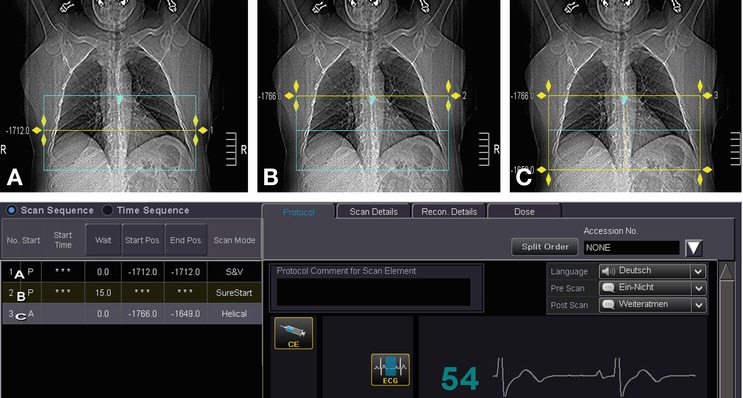
Fig. 9a.2
Planning the acquisition. A planning scan (scanogram) is acquired to identify the greatest circumference of the heart (Panel A), position the SureStart (Panel B), and define the scan length (Panel C) for the subsequent helical coronary examination. Yellow indicates the active area, while blue indicates inactive areas. As anatomical structures may be displaced as a result of respiratory motion, we recommend defining the start of the scan about 1 cm above the assumed coronary artery origins and the end of the scan about 1 cm below the heart base. Panel A shows the positioning of a single slice (low-dose scan, 50 mA) that defines the greatest circumference of the heart. Panel B shows the position of another low-dose single slice (50 mA) (Fig. 9a.4) that defines the SureStart, which serves to trigger the spiral scan once the desired density threshold has been reached. The scan is automatically started after 15 s. Panel C defines the scan length. The start of the spiral scan corresponds to the SureStart position. The tube current for the spiral scan is selected according to the patient’s weight and is higher in obese patients to ensure an adequate image quality
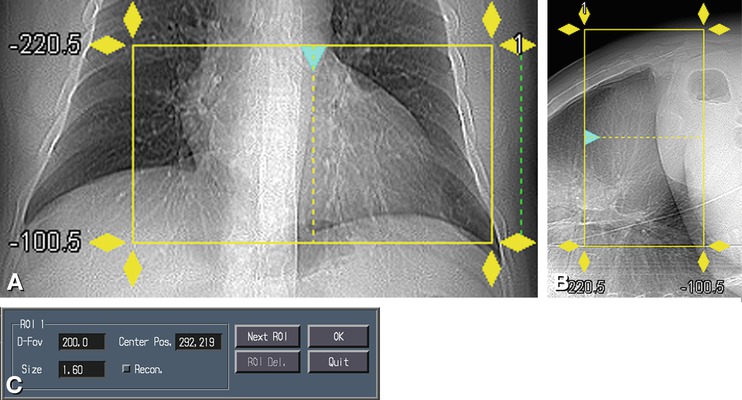
Fig. 9a.3
Defining the FoV. The scan depicting the greatest circumference of the heart seen on the anteroposterior and lateral scanogram (Panels A and B) is used to define the FoV according to individual heart size, ensuring good image quality at the highest possible spatial resolution. In the majority of patients, the FoV should be about 180 mm (Panel C)
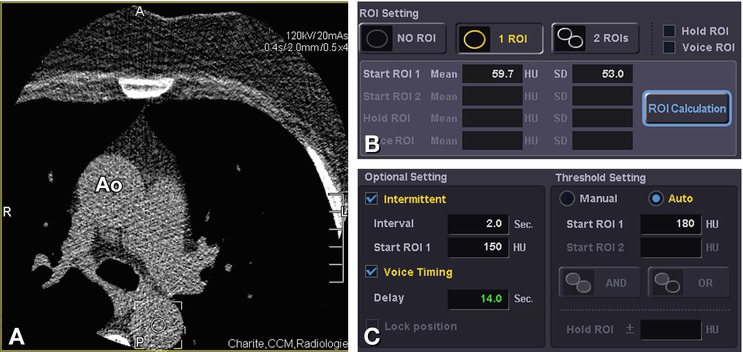
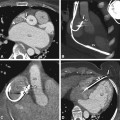
Fig. 9a.4
Planning of the SureStart. Using the SureStart (Fig. 9a.2), a ROI is identified in the descending aorta (circle in Panel A); this region should be neither too large nor too small to avoid mistriggering the spiral scan. The ROI is placed in the descending aorta because there are fewer motion artifacts than in the ascending aorta (Ao). In this way, it is possible to avoid mistriggering of the scan as a result of effects of the superior vena cava, which is opacified very early. Another safeguard is checking attenuation in the ROI (Panel A) by clicking on “ROI Calculation” (Panel B). An attenuation of about 40–60 HU is optimal. Next, the threshold of 180 HU for starting the scan is defined (Panel C), and “Auto” is selected from the menu as the start position. The scan is then automatically started once the 180 HU threshold has been reached. Alternatively, the scan can be started manually by the examiner, on the basis of visual identification of the time of optimal contrast enhancement. Starting the scan manually results in considerable variation in coronary opacification, since the start is influenced by various factors such as individual reaction time and the examiner’s level of experience
9.1.3 SureStart
Planning the individual scan delay on the Aquilion 64 using the SureStart bolus tracking tool is illustrated in Fig. 9a.4. The selected scan plane, just above the origin of the coronary arteries, is chosen to start the scan at the optimal time by monitoring the arrival of the contrast bolus in a region of interest (ROI) placed in the descending aorta (Fig. 9a.5). Important landmarks in this plane are the sternum anteriorly and the descending aorta posteriorly. Also seen in this plane are a segment of the pulmonary trunk and a portion of the anterolateral chest wall. The ROI in the descending aorta is used to monitor the increase in Hounsfield units (HU) after initiation of contrast injection.
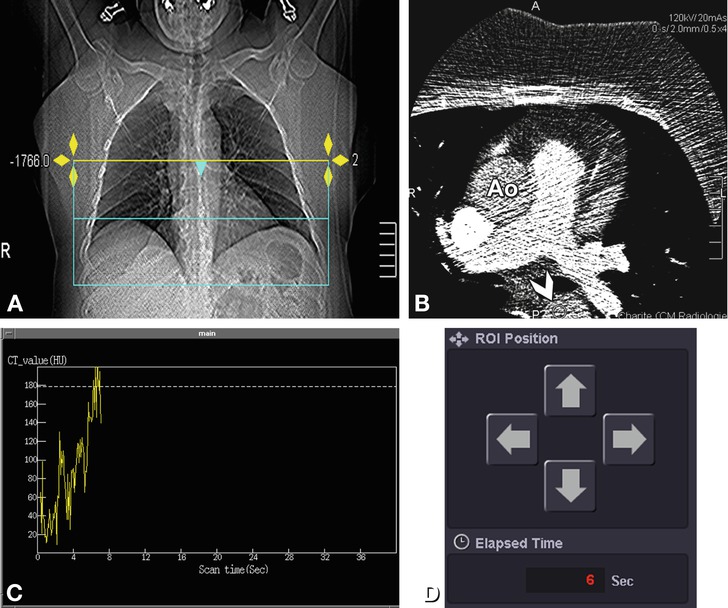
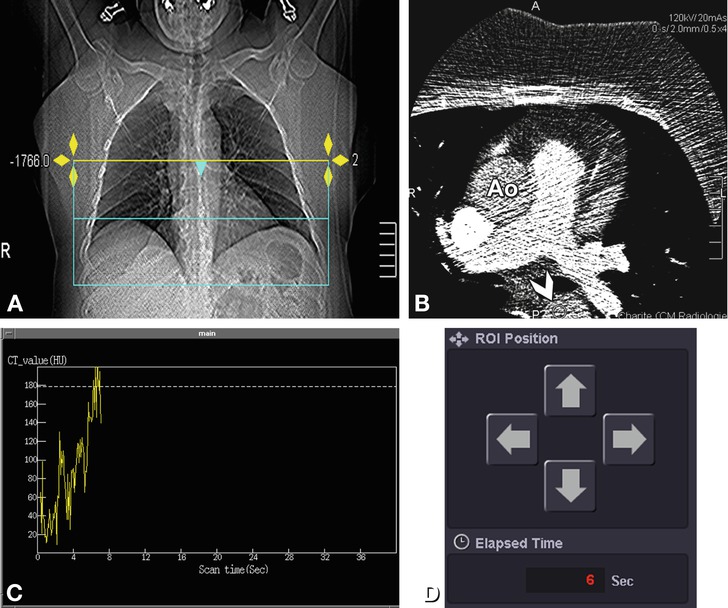
Fig. 9a.5
Start of the helical coronary examination. The position of the SureStart has been defined on the basis of the planning scan (Panel A). Next, a continuous low-dose scan (30–50 mA) is acquired at the level of the start of the spiral scan for triggering the spiral scan after IV contrast administration (Panel B). Contrast arrival can be tracked in real time. The continuous scan is started not earlier than 15 s after initiation of contrast administration for reasons of radiation protection and to ensure optimal opacification of the target vessels. Contrast arrival is measured in an ROI in the descending aorta (arrowhead and small circle in Panel B). The continuous increase in HU in the ROI over time is represented in Panel C in the form of a graph. The breathing command starts once the defined threshold of 180 HU has been reached. The scan then starts with a 3-s delay to allow the heart rate to normalize after inspiration. The arrows in Panel D represent cursor movements and can be clicked to correct the position of the ROI in the descending aorta if necessary and also displayed the elapsed time. Ao ascending aorta
The scan delay after contrast injection can be determined in one of the two ways: (1) by injection of a test bolus to determine the patient’s individual circulation time and optimize the spiral scan parameters accordingly, or (2) by bolus tracking, with automatic triggering of the scan once a predefined Hounsfield threshold has been reached (Figs. 9a.4 and 9a.5). Use of the test bolus method increases the total amount of contrast injected and may be inaccurate because the circulation time may vary. Contrast agent injection is usually followed by an automatic 40-ml intravenous saline flush administered at a flow rate of 4 ml s−1, which serves to wash out the right ventricle and improve coronary artery visualization.
Precontrast baseline attenuation is also measured in the descending aorta. In our experience, good results are achieved using a threshold of 180 HU when baseline attenuation is in the range of approximately 30–60 HU. On the basis of our experience, we recommend the use of the SureStart bolus tracking option because it consistently yields good-quality images.
9.1.4 Breath-Hold Training and Premedication
We recommend sublingual nitroglycerin administration (0.8–1.2 mg) before the breath-hold training. Nitroglycerin dilates the coronary arteries and improves the comparability of the CT findings with those of cardiac catheterization. The effect of nitroglycerin lasts for about 10–30 min. Although nitroglycerin is usually well tolerated, patients should be monitored for the occurrence of possible hemodynamic side effects (e.g., hypotension).
In our department, we use an automatic speech system for the breathing commands (“Please breathe in and hold your breath”). The required breath-hold period is about 6–30 s, depending on the scanner used and the scan volume. Breath-hold training is done without radiation exposure, and the physician or technician should stand next to the patient to verify that the patient can hold his/her breath in submaximal inspiration for the required period and also to check for possible ECG alterations during inspiration. Toshiba scanners have a special function for breath-hold training. Heart rate variability should be less than 10% to achieve good results (Fig. 9a.6). Breath-hold training can be repeated if the ECG is suboptimal. If intravenous beta blocker injection is deemed necessary, it can be done at this stage. Heart rate variability is determined for individual adjustment of scan parameters such as pitch and gantry rotation time. A consistent image quality is achieved in all patients if the tube current is adjusted according to body weight (Chap. 8).


Fig. 9a.6
Breath-hold examination. Breath-hold training is performed by selecting “Breath Ex.” from the Scan Details menu. As can be seen in Panel A, the default breath-hold time should be 10–12 s for scanning of the coronary arteries. When bypasses are scanned, longer breath-hold periods are needed according to the scan length. The test is started by clicking on “Breath Ex.”; the breathing commands that will also be used during the actual scan are then heard. The computer automatically calculates heart rate variability (which should be <10%), the optimal helical pitch (HP), and gantry rotation time. Panel B shows a case in which heart rate variability is in the upper normal range (80–92 beats per min). Panel C shows the results of a second test at a later time after intravenous beta blocker administration. The result is good, with a heart rate of 50–55 beats per min, and the examination can proceed. Panel D shows the results of the breath-hold test: a breath-hold time of 10.8 s, total scan time of 6.4 s, heart rate of 50–55 beats per min, and a recommended HP of 17.1. Other recommended scan parameters are shown in Panel E
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree