Total Body Irradiation
Total body irradiation (TBI) with megavoltage photon beams is most commonly used as part of the conditioning regimen for bone marrow transplantation, which is used in the treatment of a variety of diseases such as leukemia, aplastic anemia, lymphoma, multiple myeloma, autoimmune diseases, and inborn errors of metabolism. The role of TBI is to destroy the recipient’s bone marrow and tumor cells, and to immunosuppress the patient sufficiently to avoid rejection of the donor bone marrow transplant. Usually the patient undergoes a chemotherapy conditioning program before the TBI and bone marrow transplant. Although chemotherapy alone can be used as a conditioning regimen, addition of TBI is considered beneficial for certain diseases and clinical conditions. For example, TBI allows the delivery of a homogeneous dose to the entire body including “sanctuary areas” for tumor cells where chemotherapy may not be effective. Also, selected parts of the body (e.g., lungs, kidneys, head) can be shielded from radiation, if desired.
18.1. TECHNIQUES AND EQUIPMENT
Numerous techniques have been used to deliver TBI. Details of some of the commonly used techniques and the associated dosimetry are discussed in the literature (1, 2, 3, 4, 5). The choice of a particular technique depends on the available equipment, photon beam energy, maximum possible field size, treatment distance, dose rate, patient dimensions, and the need to selectively shield certain body structures. An anteroposterior (AP)/posteroanterior (PA) technique generally provides a better dose uniformity along the longitudinal body axis, but the patient positioning, other than standing upright, may pose problems. Bilateral TBI (treating from the left and right side of the body) can be more comfortable to the patient if seated or lying down supine on a specially designed TBI couch, but presents greater variation in body thickness along the path of the beam. Compensators are, therefore, required to achieve dose uniformity along the body axis to within ±10%, although extremities and some noncritical structures may exceed this specification.
A. BEAM ENERGY
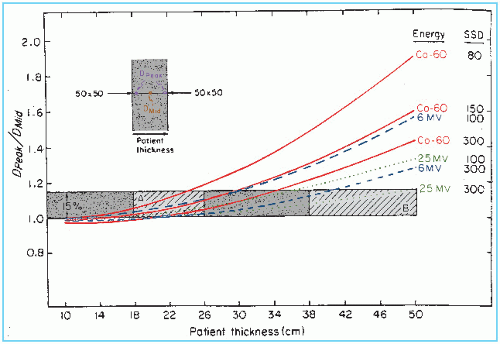
Cobalt-60 beams were used in the early days to deliver TBI, especially for protocols involving a low dose rate of 5 to 10 cGy/min. A review of these techniques and the modifications required to achieve large homogeneous fields with these machines is summarized in the American Association of Physicists in Medicine (AAPM) Report No. 17 (3). Because the linear accelerator is the most commonly used equipment for radiation therapy, current TBI techniques have been adopted for linacs. The choice of photon beam energy is dictated by patient thickness and the specification of dose homogeneity. In addition to the thickness variation along the axis of the patient, the patient thickness along the path of beam also affects dose uniformity, depending on beam energy. As discussed in Chapter 11, Section 11.5A, the thicker the patient, the higher is the beam energy required to produce acceptable dose uniformity for parallel opposed fields. Figure 18.1 shows that the ratio of the maximum dose to the midline dose is a function of energy and patient thickness when parallel opposed beams are used. Not considering the initial dose buildup effect, it is seen that the higher the beam energy, the greater is the dose uniformity for patients of any thickness. If the maximum thickness of the patient parallel to the beam central axis is less than 35 cm and the source to surface dose (SSD) is at least 300 cm, a 6-MV beam can be used for parallel opposed TBI fields without increasing the peripheral dose to greater than
110% of the midline dose. For patients of thickness greater than 35 cm, energies higher than 6 MV should be used to minimize the maximum dose (Dmax) to midplane dose ratio.
110% of the midline dose. For patients of thickness greater than 35 cm, energies higher than 6 MV should be used to minimize the maximum dose (Dmax) to midplane dose ratio.
B. INITIAL DOSE BUILDUP
Surface or skin dose in megavoltage beams is substantially less than the dose at the point of maximum dose (Dmax), as has been discussed in Chapter 13, Section 13.3. The dose buildup characteristics depend on many factors such as energy, field size, SSD, and beam angle relative to the surface. Dose buildup data obtained at normal SSDs (e.g., 100 cm) do not apply accurately at TBI distances (e.g., 400 cm) because of the longer distance and the intervening air (1). However, most TBI protocols do not require skin sparing. Instead, a bolus or a beam spoiler is specified to bring the surface dose to at least 90% of the prescribed TBI dose. A large spoiler screen of 1- to 2-cm-thick acrylic is sufficient to meet these requirements, provided the screen is placed as close as possible to the patient surface.
C. PATIENT SUPPORT/POSITIONING DEVICES
Patient support and positioning devices are designed to implement a given treatment technique. Important criteria include patient comfort, stability, and reproducibility of setup and treatment geometry that allows accurate calculation and delivery of dose in accordance with the TBI protocol. The following techniques are currently in use at the University of Minnesota and are presented here as examples. The associated equipment has been designed to meet various protocol criteria, based principally on two techniques: AP/PA and bilateral.
C.1. Bilateral Total Body Irradiation
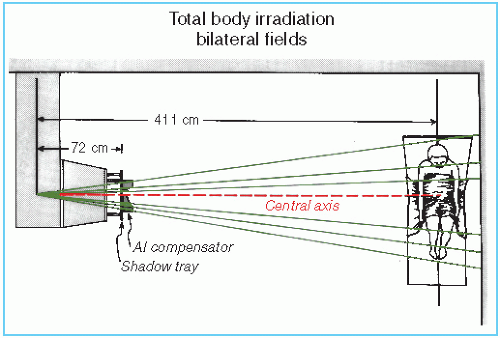
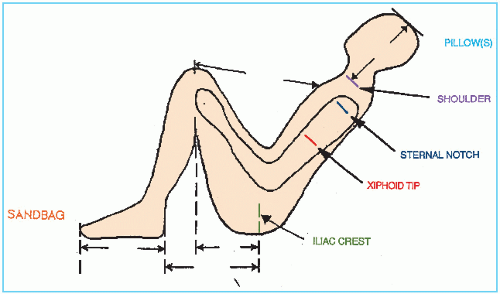
A technique involving left and right lateral opposing fields with the patient seated on a couch in a semifetal position was designed by Khan et al. (1). Basic treatment geometry is illustrated in Figure 18.2. A special TBI couch allows the patient to be seated comfortably with the back supported and legs semicollapsed as seen in Figure 18.3. The arms are positioned laterally to follow the body contour and placed in contact with the body at the mid-AP thickness level. Care is taken to ensure that the arms shadow the lungs instead of the spinal column located posteriorly. The patient setup is recorded in terms of distances measured between external bony landmarks as shown in Figure 18.4. The source to body axis distance is measured by a sagittal laser light installed in the ceiling to mark the TBI distance. The laser light also helps to position the patient’s sagittal axis at right angles to the beam’s central axis.
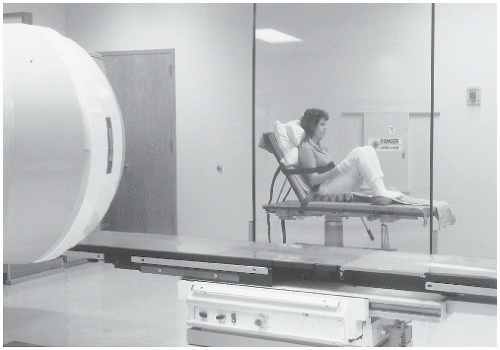 Figure 18.3. Photograph demonstrating patient setup on the total body irradiation couch for the bilateral technique. |
The lateral body thickness along the patient axis varies considerably in the bilateral TBI technique. To achieve dose uniformity within ±10% along the sagittal axis of the body, compensators are designed for head and neck, lungs (if needed), and legs. The reference thickness for compensation is the lateral diameter of the body at the level of the umbilicus (not including the arms), assuming that the protocol specifies dose prescription to be at the midpoint at the level of the umbilicus. Compensators can be designed out of any material, but at the University of Minnesota they are custom-made out of aluminum. A special tray and clamps are used to hold these compensators in place (Fig. 18.5). Field light is used to cast a shadow of the compensator onto the patient’s body. Alignment is checked using shadows of positioning pegs on the compensators and the patient’s reference bony landmarks.
C.2. AP/PA Total Body Irradiation
The patient is irradiated anteroposteriorly by parallel opposed fields while positioned in a standing upright position at the TBI distance. This technique was developed at the Memorial Sloan Kettering Hospital in New York (6




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree