Trachea: Acute and Chronic Effects of Blunt and Penetrating Trauma and Mucosal Injury
KEY POINTS
- Computed tomography is the imaging examination of choice for evaluating blunt-force and penetrating trauma and complications of all forms of upper airway injury.
- Computed tomography is an ideal complement to clinical and endoscopic examinations.
- Swallowing studies are still sometimes useful.
- Acute injury must be diagnosed and treated within 3 to 7 days for optimal outcome.
- The status of the cricoid cartilage is a critical prognostic element.
- Tracheal and laryngeal injury is sometimes overlooked in multitrauma victims with more obviously life-threatening problems.
The trachea is commonly injured accidentally or iatrogenically. Iatrogenic trauma is discussed in conjunction with tracheal stenosis and tracheomalacia in Chapter 214. Blunt tracheal and laryngeal injuries are so intimately related that tracheal trauma should be studied in combination with the complete discussion of laryngeal injuries in Chapter 207.
The treatment principles for the injured trachea have been in place for decades and well before the advent of computed tomography (CT) and magnetic resonance imaging (MRI). Treatment has varied little since this earlier reported experience; however, triage, planning, and prognosis are now executed in a more informed context because of diagnostic imaging input that augments the mainstay of diagnosis, improved modern endoscopic techniques, and laser options.
The imaging appearance of an injured trachea depends directly on the mechanism of injury. Imaging, almost entirely done nowadays with CT, shows the extent of injury to the tracheal and laryngeal skeleton and related tissues. In the late 1970s and into the 1980s, CT significantly advanced our understanding of how the trachea and larynx respond to blunt and other forms of trauma.1–3 Imaging with CT, and occasionally other studies, takes its place alongside endoscopy on the critical path for triage of tracheal injuries to proper management plans.
ANATOMIC CONSIDERATIONS
Applied Anatomy
A thorough knowledge of the anatomy and anatomic variations of normal in each of the following areas is required for the evaluation of tracheal trauma. This anatomy is presented in detail with the introductory material on the trachea, larynx, hypopharynx, cervical esophagus, and infrahyoid neck in general:
Evaluation of Primary Tracheal, Laryngeal, and Hypopharyngeal Injury
- Trachea and larynx, including their skeleton, contained deep tissue spaces, normal mucosal variation and landmarks, and functional structures (Chapters 201 and 209)
- Hypopharynx (Chapter 215)
- Cervical esophagus, most importantly the esophageal verge junction with the postcricoid portion of the hypopharynx (Chapter 221)
Evaluation of Injuries to Extratracheal Structures
- Visceral compartment of the neck and related fasciae (Chapter 149)
Evaluation of Related Vocal Cord Dysfunction and Nerve Injury
- Knowledge of the entire course of the vagus and recurrent laryngeal nerves on both sides (Chapter 201)
IMAGING APPROACH
Techniques and Relevant Aspects
The trachea is studied in essentially the same manner for trauma as it is for the evaluation of known or suspected laryngeal trauma; however, study of the trachea should be continued to the carina so that the entire trachea is included.
The principles of using these studies are reviewed in Chapters 207 and 208 on laryngeal trauma. Specific problem-driven protocols for CT and MRI of tracheal and laryngeal trauma are presented in Appendixes A and B, respectively.
Intravenous contrast is used selectively, such as in acute trauma, to identify associated vascular injuries or in the subacute setting when a complicating infection is suspected. The studies are most typically done without contrast.
Pros and Cons
CT is the primary imaging examination for blunt, penetrating, and iatrogenic trauma as well as for retained foreign bodies. CT is a major advantage for the laryngologist in this regard. A patient with severe head and neck injuries presents no problem for safe and convenient tracheal imaging at the same time as the brain, face, and cervical spine, and multiple other systems are evaluated by multidetector CT at the initial intake. This is particularly important in multisystem trauma due to motor vehicle accidents since these a very common cause of blunt laryngotracheal trauma.
CT may be used to screen for associated false passages but cannot be used to exclude such mucosal injury. Swallowing studies are used to screen for false passages as suggested by endoscopic evaluation.
MRI is almost never used for the evaluation of acute trauma and is infrequently indicated in chronic conditions. It has been used very selectively for chronic traumatic conditions resulting in very unusual circumstances, mainly when the prevertebral space or neural elements might be injured or involved in a complication of the injury.
SPECIFIC DISEASE/CONDITION
Primary Mucosal Injuries
Mucosal tracheal injuries are a potential source of long-term airway disability. These may be due to blunt and penetrating trauma, intubation, burns, caustic aspiration, and inflammatory disease (Chapter 210). The common pathway of tracheal mucosal injury is the lining becoming denuded due to direct injury, pressure necrosis, or chronic irritation (Figs. 213.1–213.6). For instance, pressure necrosis occurs during prolonged intubation when the cuff pressure exceeds capillary perfusion pressure, causing a chain of events starting with mucosal ischemia and necrosis. This eventually leads to exposure of laryngeal cartilage, chondritis, and granulation tissue formation (Fig. 213.2). The end stage of this common pathogenesis is a final maturation into firm scar tissue (Chapters 208 and 214) that reduces the lumen of the airway (Figs. 208.1–208.6). The tracheal wall may weaken, and a dynamic component due to tracheomalacia may add to the airway compromise. Caustic aspiration (Fig. 213.5) and burns (Fig. 213.4) can lead to the same chain of events.
Extension of the inflammatory process may produce a fistula to the esophagus or brachiocephalic vessels (Fig. 213.3). Secondary infection, possibly resulting in infectious chondritis and/or deep neck abscess, is another possible complication (Fig. 213.4).
Granulation tissue in the subacute phase of an injury (10 to 30 days post trauma) looks the same as hemorrhage and edema in the acute phase (Figs. 207.8 and 213.2). Nearly complete tracheal airway occlusion by a fairly homogeneous soft tissue mass that appears to be of lower density than the nearby neck musculature has proven at surgery to be granulation tissue. The reasons for its lower density than muscle are not known. CT is normally done without contrast for trauma. Contrast-enhanced computed tomography (CECT) would likely show more enhancement in granulation tissue than muscle in this subacute phase. Such information has not been shown to be useful for medical decision making in this clinical setting.
Granulation tissue will organize and contract with time. During this evolution, it typically remains lower in density than normal muscle tissue (Fig. 207.9).
Soft tissue webs form from this tissue and may appear as sharply contoured thickening of the soft tissues within the airway. Fibrotic webs commonly occur at the anterior and posterior commissure. A circumferential rim of this tissue may narrow the subglottic airway. Subglottic tissue has sharp margins and is symmetric. It may be asymmetric and irregular. Herniations (false diverticuli) of the airway may extend into the separations between fragmented portions of the laryngeal cartilages (Fig. 207.9D).
CT demonstrates the cross-sectional area of the residual airway lumen (Fig. 208.2B and Chapter 214). This measured area is the best correlate for airway functional studies. As well, this area is a key factor in medical decision making. Reduction of airway luminal area leads to a proportionate decrease in airflow and worsening functional airway capacity of the patient. In adults, <25% reduction of airway cross-sectional area usually causes few symptoms. A 25% to 50% reduction causes dyspnea with fairly extreme exertion, while a 50% to 75% reduction might produce dyspnea with mild exertion. A <75% reduction may cause symptoms at rest and audile stridor. The time course of any airway obstruction is also critical. Acute airway obstruction is much more poorly tolerated than a more chronic, progressive process.
The long-term effects of these basic mechanisms of injury as they relate to the most common cause of structural tracheal airway dysfunction, postintubation, and posttracheostomy injury are discussed in Chapter 224.
Blunt and Penetrating Tracheal Trauma and Aspirated Foreign Bodies
Blunt laryngotracheal trauma mechanisms are discussed and illustrated in detail in Chapter 207. The injury most commonly is due to a force applied from anterior to posterior, perhaps somewhat obliquely or off the midline (Figs. 207.1–207.5), compressing the larynx between the offending force and the cervical spine. This type of injury poses the risk of separation at the cricotracheal junction or a crush injury of the trachea; both of these injuries do not come to imaging very often because they are typically immediately fatal (Figs. 207.13 and 213.6).
Penetrating injuries are most frequently related to stab and gunshot wounds (Fig. 207.15). These will usually be evaluated in conjunction with more potential serious injuries to the brachiocephalic vessels in penetrating neck injuries.
Very severe blunt trauma and crush injuries may lead to a combination of findings and considerations seen in both blunt and penetrating mechanisms (Fig. 207.7).
Clinical Presentation
Blunt-force and penetrating injuries of the trachea and larynx may compromise critical functions. Airway maintenance is always the primary concern. Once the airway is secured, therapy is focused on preserving other airway function, including a voice, and assuring swallowing without aspiration. Acute injuries require a rapid examination that is accurate and free of potential added morbidity.
Patterns of Disease as Seen on Imaging
Soft Tissue Injuries
Blunt laryngotracheal trauma results in blood and edema that spreads through the deep planes of the subglottis. The subglottic spread is directed circumferentially by the conus elasticus, causing soft tissue swelling between the inner border of the cricoid and the airway (Figs. 207.1 and 213.6). The subglottic bleeding and edema spreads inferiorly and across the cricotracheal junction to circumferentially narrow the tracheal airway. Limited membranous lesions may cause air leakage and substantial neck emphysema, without much effect on the airway (Fig. 207.12).
Axial CT shows the cross-sectional area of the airway (Figs. 207.1–207.8). This view of the airway is the most useful to compare with the clinical examination. Combined with multiplanar reconstructions, these images are superb for airway assessment. Three-dimensional and virtual endoscopic images are easily generated but in practice are not used routinely for clinical decision making. Swelling within the larynx may prevent a complete endoscopic examination of the airway; in these cases, airway appraisal by CT is even more critical.
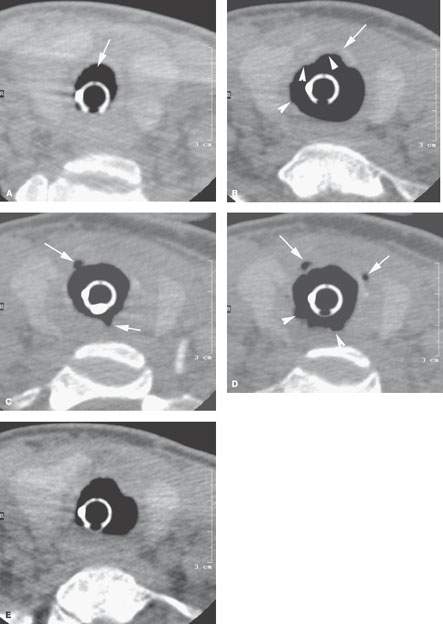
FIGURE 213.1. Non–contrast-enhanced computed tomography study of a patient who had overdistension of an endotracheal tube balloon at the junction of the cricoid cartilage and trachea including the first two tracheal segments. A: An image distal to the balloon showing the normal tracheal lumen along with the endotracheal tube for reference. B–E: Images made continuously from superior to inferior. In (B), the cricoid arch is seen anterior to the airway (arrow), indicating that the balloon was inflated both above and below the level of the cricotracheal junction. The balloon assumes a somewhat unusual shape anteriorly and shows slight irregularities along its margins (arrowheads) at this level, suggesting areas of disproportionate pressure distribution. In (C), gas can be seen beyond the balloon within the mucosa and submucosa of the trachea (arrows). In (D), the margins of the balloon interfacing with the tracheal wall are irregular, suggesting possible necrosis of the mucosal lining. This is further suggested by gas clearly deep to the trachea mucosa (arrows). In (E), the section is made at the bottom of the balloon, which asymmetrically conforms to the airway shape. (NOTE: This case is used to illustrate a pathophysiologic mechanism of injury to the trachea, namely mucosal pressure necrosis that is at least partially ischemic in nature. This necrosis of the mucosal lining may then allow secondary infection. If there is no infection, the necrosis begins the inflammatory response that will result in granulation tissue and then end-stage scar. If the process involves the cartilages, as it almost certainly does in this instance judging from the pockets of gas separate from the tracheal mucosa, then some degree of weakening of cartilage to produce chondromalacia would be expected as part of the end-stage changes.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








