Trachea: Benign and Malignant Tumors
KEY POINTS
- Computed tomography and magnetic resonance imaging are critical to the treatment planning for tracheal tumors.
- Magnetic resonance is superior to computed tomography for demonstrating the relationship of tumor to the tracheal wall, hypopharynx, esophagus, and thyroid gland.
- Computed tomography and magnetic resonance imaging can provide information about the initial airway status and possible cumulative risk of further airway compromise associated with manipulation and treatment of the tumor.
Intrinsic tracheal tumors (Figs. 212.1–212.3) are uncommon, and benign tumors are rare except for papillomas (Figs. 212.4 and 212.5). The trachea is far more commonly secondarily involved by spread of tumors from adjacent sites of origin— most commonly the larynx, hypopharynx, and thyroid gland—than a primary site (Figs. 212.6–212.12). Squamous cell carcinoma (SCCA) is the most common primary tracheal malignancy (Fig. 212.3) followed by adenoid cystic (carcinoid) (Fig. 212.2) and mucoepidermoid carcinoma (Fig. 212.1). Tracheal metastases occur rarely but virtually always occur in the setting of a known primary (Fig. 212.13). Approximately 10% of primary tracheal tumors are benign (Figs. 212.4 and 212.5). The most common benign tumor is by far the squamous papilloma associated with viral exposure (Fig. 212.4). Other benign tumors included pleomorphic adenoma, granular cell tumor, and those of cartilage origin.
Staging and medical decision-making procedures for tracheal tumors include endoscopy with biopsy, contrast-enhanced computed tomography (CECT) or contrast-enhanced magnetic resonance (CEMR) depending on the practice preference, and a chest x-ray. Imaging studies are an essential component of the clinical and diagnostic evaluation, providing unique and often pivotal information that complements the clinical examination. Imaging provides additional information concerning the deep extent and regional spread of disease. Chest computed tomography (CT) and fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) may provide additional information in selected cases.
This chapter describes the important role of diagnostic imaging in clinical decision making for primary tracheal tumors. Those arising from adjacent organs are summarized and illustrated for completeness but are discussed in dedicated chapters about tumors arising from those other primary sites.
APPLIED ANATOMY
A thorough knowledge of tracheal anatomy and anatomic variations in each of the following areas is required for the evaluation of tracheal tumors. This anatomy is presented in detail with the introductory chapters on the trachea, larynx, hypopharynx, cervical esophagus, and infrahyoid neck in general:
Evaluation of the Trachea and Closely Related Organs Frequently Involved with Contiguous Disease in these Tumors
- Trachea (Chapter 209)
- Larynx, including the laryngeal skeleton and deep tissues spaces, especially those of the subglottis (Chapter 201)
- Hypopharynx (Chapter 215)
- Cervical esophagus and its membranous wall in common with the trachea and both of their relationships to the postcricoid portion of the hypopharynx (Chapter 221)
Evaluation of Spread Beyond the Trachea
- Visceral compartment of the neck and related fasciae (Chapter 149)
Evaluation of Regional Lymph Node Disease
- Detailed knowledge of normal node and perinodal morphology and the common drainage pathways of tracheal cancer, which emphasizes node levels 4 through 6 and the mediastinal groups (Chapters 149 and 157)
Evaluation of Perivascular and Perineural Spread
- Knowledge of the entire course of the vagus and inferior laryngeal neurovascular bundle, including the recurrent laryngeal nerves on both sides (Chapter 201)
IMAGING APPROACH
Techniques and Relevant Aspects
The trachea is studied in essentially the same manner for tumors as it is for the evaluation of known or suspected laryngeal or thyroid cancer. Study of the trachea for tumors should be continued to the carina so that the entire trachea and contiguous mediastinal node groups are included.
The principles of using these studies are reviewed in Chapters 69, 172, 201, and 206. Specific problem-driven protocols for CT and magnetic resonance imaging (MRI) of the trachea, larynx, hypopharynx, and thyroid gland tumors are presented in Appendixes A and B, respectively.
There is little or no use for ultrasound in studying these tumors.
FDG-PET may be useful in selected cases once a diagnosis of malignancy is established by biopsy. In some cases, it might be used before biopsy or on the basis of anatomic imaging findings to establish a risk profile for malignancy.
Pros and Cons
Evaluation of Submucosal or Other Masses of Uncertain Etiology
Benign masses limited to the trachea and malignant tumors have essentially the same initial presentation. Any presentation, regardless of potential etiology, that is suspicious for a tracheal mass should eventually be studied with CT or MRI as the clinical evaluation directs the workup (Figs. 212.1–212.5 and 212.13). MRI can be used initially, if preferred, but is more likely to be degraded than CT studies and is sometimes rendered nondiagnostic due to motion artifacts. A preferred approach might be to use a supplemental magnetic resonance (MR) study in a localized area of interest, where it might add meaningful incremental data as directed by findings on an initial CT. In this way, the strengths of MRI related to better soft tissue contrast resolution may be exploited to optimally answer questions that aid precise surgical or alternative planning (Fig. 212.1).
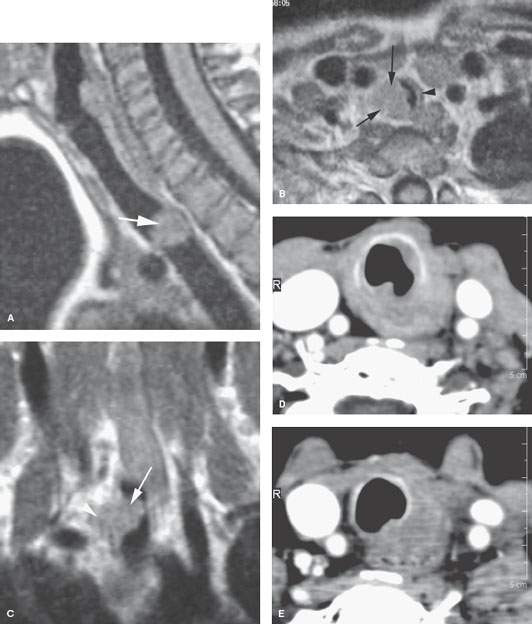
FIGURE 212.1. Two patients with mucoepidermoid carcinoma of the trachea. A–C: Pediatric Patient 1 presenting with stridor. Magnetic resonance imaging and biopsy suggested that this was due to a tracheal primary but subsequently proved to be a low-grade mucoepidermoid carcinoma. This magnetic resonance study was instrumental in planning the tracheal resection and reconstruction. Contrast-enhanced T1-weighted images show the well-circumscribed mass (arrows) arising from the right lateral wall of the trachea at the thoracic inlet (A, B). The tumor was restrained by the tracheal cartilages and connecting membranes at surgery. Its overall extent as seen on the coronal image in (C) dictated the number of tracheal rings that needed to be resected. The correlation of surgery was very precise, and the trachea was repaired primarily by use of combined soft tissue and cartilage rib tissue. The airway was restored, and the patient was cured. D, E: Patient 2 presenting with dysphagia and coughing. No masses were seen endoscopically. Contrast-enhanced computed tomography shows an infiltrating lesion at the junction of the trachea and esophagus. Primary sites considered were the esophagus, trachea, and thyroid. Sometimes it is difficult to be sure of the primary site even with precise anatomic imaging. This was eventually considered to be a primary tumor of the thyroid gland, although mucoepidermoid carcinoma of the thyroid gland is rare. From the imaging, either the wall of the trachea or esophagus would be the likely primary site.
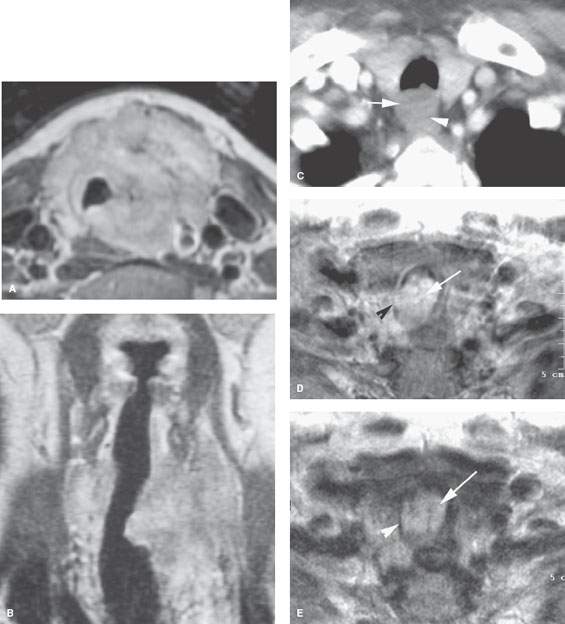
FIGURE 212.2. Three patients with adenoid cystic carcinoma of the trachea, each with different manifestations. A, B: Patient 1. Contrast-enhanced T1-weighted (T1W) image showing what was a slow-growing mass surrounding the trachea and extending cephalocaudal as seen in the coronal section in (B). This patient had years of airway symptoms that were not evaluated with imaging until there was a palpable neck mass that revealed this primary adenoid cystic carcinoma. C: Patient 2. Contrast-enhanced computed tomography study of a patient presenting with dysphagia and cough. The adenoid cystic carcinoma that was arising from the membranous wall of the trachea (arrow) was difficult to tell on this study from a cervical esophageal primary, with the interface between the two (arrowhead) not being clear. D, E: Patient 3 presenting with airway obstruction and cough. The slightly degraded T1W image in (A) shows an enhancing and predominately endoluminal mass (arrow) invading the trachea wall. On the T2-weighted image in (E), the mass is homogeneously bright, which is consistent with it being a well-differentiated adenoid cystic carcinoma and composed of microcystic spaces (arrow). The invasion of the cartilage tracheal ring is visible (arrowhead) compared to the normal opposite side.
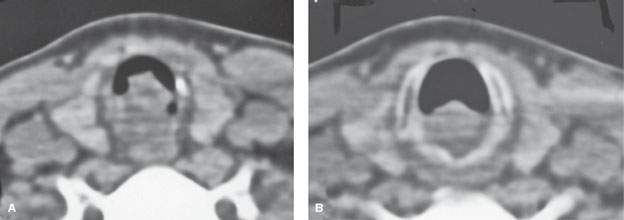
FIGURE 212.3. Squamous cell carcinoma (SCCA) is the most common histologic diagnosis for tracheal cancer. This patient presented with cough and external dyspnea. A non–contrast-enhanced computed tomography (CT) study was done and showed this primary tumor. At endoscopy, the mass was entirely submucosal and believed to arise from the subglottis. The CT study showed the mass to actually be arising from the upper trachea as seen in (A) and extending superiorly to involve the low subglottis as seen in (B). Submucosal SCCA was confirmed histologically. (NOTE: This patient indicates that substantial amounts of submucosal spread may not be appreciated on endoscopic examination.)
Integrity of the Airway
Any imaging study of a diseased trachea must be evaluated for the disease effect on the airway. The anatomic status of the airway, as well as the risk of any acute adverse complication, such as the potential for rapidly progressive airway obstruction either by the mass or a potential airway complication that might arise as a result of biopsy, should be reported (Figs. 212.7 and 212.10). For instance, biopsy of an unanticipated hypervascular mass could lead to an unfortunate amount of hemorrhage and aspiration of blood. More likely, a mass that nearly occludes the airway completely could swell with biopsy and complete the occlusion; imaging might help to anticipate the necessity for at least temporary airway control following the biopsy, so the patient will have an understanding of the odds of that happening (Figs. 212.7 and 212.10). Multiplanar and virtual endoscopic processing of images can help to obviate some endoscopic and bronchoscopy procedures (Fig. 212.4) for at least gross airway assessment, even though such virtual anatomic studies lack dynamic information and only provide indirect functional information, with the latter based on the degree of reduction of airway cross-sectional area.
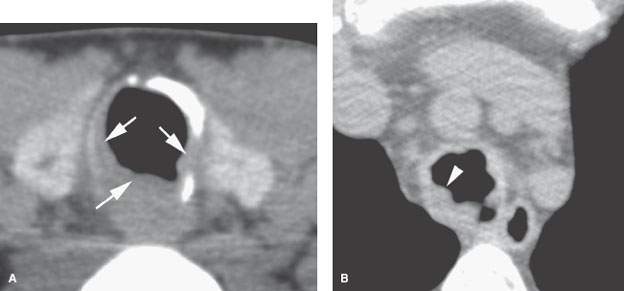
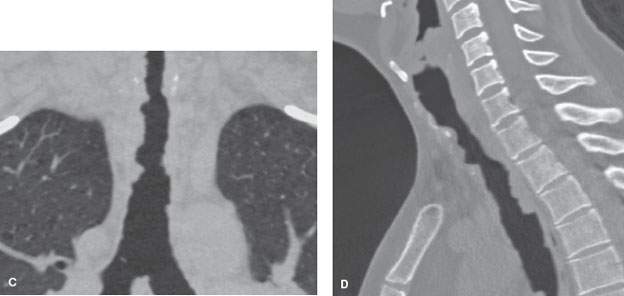
FIGURE 212.4. A young patient with laryngeal and tracheal papillomatosis. Non–contrast-enhanced computed tomography was done. This study was done to supplement the endoscopic examination to determine the overall extent of disease and to create a baseline for follow-up of conservative management. In (A), the section through the first tracheal ring shows the dystrophic calcification of the ring due to prior laser excisions and multiple areas of mucosal thickening related to polyps. Just beyond the thoracic inlet in (B), the papillary nature of the polyps is visible, circumferentially involving the lumen of the trachea (arrowhead). The overall extent of disease was documented for follow-up purposes on the coronal and sagittal reformatted images seen in (C) and (D).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








