TRACHEA: INFECTIOUS AND NONINFECTIOUS INFLAMMATORY DISEASES
KEY POINTS
- Computed tomography can provide a safe and rapid assessment of the airway in a patient who is stable, under the control of the treating physician for airway management decisions, and wishes to avoid endoscopy.
- Imaging is occasionally useful in the differentiating croup from epiglottitis/supraglottitis and other acute pyogenic laryngeal infections.
- Imaging in inflammatory laryngotracheal diseases, except relapsing polychondritis, is generally nonspecific for diagnosis purposes.
- Atypical clinical and imaging features of tracheal pathology should raise the possibility of an inflammatory process.
A variety of infectious and noninfectious inflammatory disorders may affect the trachea most typically as a combination of laryngeal and tracheal airway disease. Since most of these diseases are shared in common with the larynx, and since the tracheal component is typically lesser than that seen in the larynx, the reader should review this chapter and Chapter 204 together when appropriate. This chapter will emphasize those inflammatory conditions that dominantly involve or arise in the trachea.
The vast majority of these inflammatory diseases never come to imaging. Many that do really do not require imaging, but the imaging study is obtained because the etiology of the disease is uncertain, and it is thought that imaging might help with the diagnostic process (Fig. 211.1). This may occur in diseases that can mimic cancer, as may several diseases in this category. Others come to imaging for a noninvasive assessment of the static airway dimensions when it is felt that this might be less risky and/or sufficient to decide on the proper course of airway management (Fig. 211.2).
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
A thorough knowledge of tracheal anatomy and anatomic variations in each of the following areas is required for the evaluation of tracheal inflammatory diseases. This anatomy is presented in detail with the introductory material on the larynx, hypopharynx, cervical esophagus, and infrahyoid neck in general:
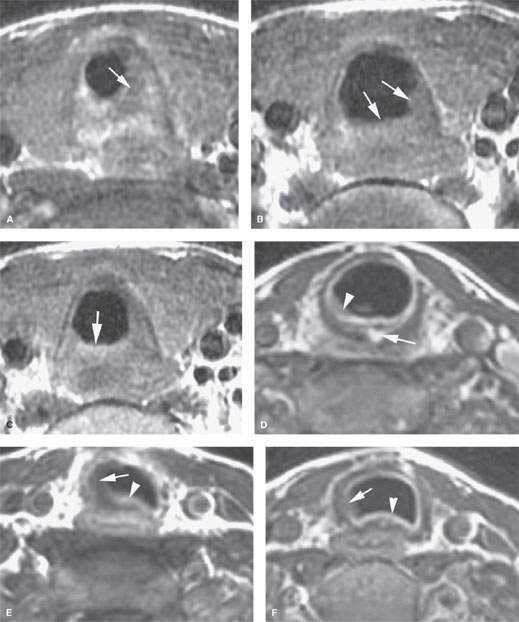
FIGURE 211.1. Two patients with noninfectious inflammatory diseases involving the trachea. A–C: Patient 1. Contrast-enhanced T1-weighted (T1W) images of a patient with amyloidosis involving the larynx and trachea. In (A), through the low subglottic region, the partially enhancing and partially nonenhancing amyloid deposits narrow the airway considerably (arrow). In the trachea in (B) and (C), the degree of airway narrowing is less, and the enhancement of the deposited material is still variable. Such findings are nonspecific. (NOTE: In general, this type of nonspecific appearance is typical of the noninfectious inflammatory diseases that affect the larynx and trachea. More examples of these diseases are shown in Chapter 204.) D–F: Patient 2. Contrast-enhanced T1W images of a patient with autoimmune disease involving the larynx and trachea. Additional images through the subglottic larynx are shown in Figure 204.16. In (D), there is mucosal enhancement (arrowhead) and an area of enhancement within the posterior aspect of the cricoid cartilage (arrow). Sections through the larynx not shown here demonstrated a fistula between the subglottis and postcricoid portion of the hypopharynx. In (E), there is mucosal enhancement (arrowhead) and mucosal edema as well as additional low signal intensity extending the full thickness of the tracheal cartilage (arrow). In (F), that trend continues with mucosal enhancement and full thickness involvement of the cartilage of the trachea.
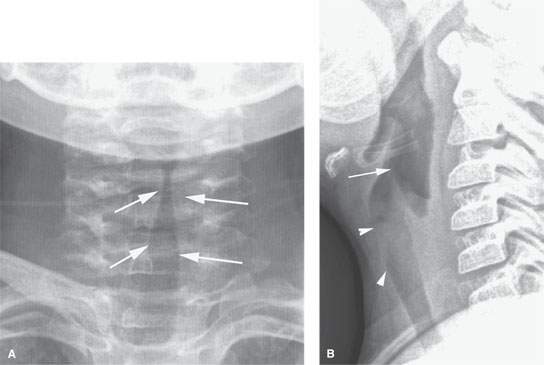
FIGURE 211.2. A young child with croup. Plain film anteroposterior and lateral views show narrowing of the subglottic and upper tracheal airway (arrows in A). In (B), the narrowing of the subglottic and upper tracheal area is less clear, although there is some increased density overlying the subglottis and upper trachea reflecting the airway compromise (arrowheads). The distention of the pharynx and laryngeal vestibule is typical since the airway is obstructed at the subglottic level, creating back pressure.
Evaluation of Tracheal and Related Structures Frequently Involved with Contiguous Disease in these Conditions should Include the Following
- Trachea (Chapter 209)
- Larynx, including the laryngeal skeleton, deep tissues spaces within the larynx, mucosal landmarks, and functional structures within the larynx (Chapter 201)
- Hypopharynx (Chapter 215)
- Cervical esophagus and its junction with the postcricoid portion of the hypopharynx (Chapter 221)
Evaluation of Spread Beyond the Trachea
- Visceral compartment of the neck and related fasciae (Chapter 149)
IMAGING APPROACH
Techniques and Relevant Aspects
The trachea is studied in essentially the same manner for inflammatory abnormalities and other benign laryngeal conditions of known or uncertain etiology as it is for the evaluation of known or suspected laryngeal cancer. If only the airway dimensions and length of involvement are of interest, intravenous contrast may not be necessary.
Magnetic resonance (MR) studies should be done with receiver coils that are custom designed to study the neck. Posteriorly placed receiver coils meant to study the spine are not adequate.
The use of intravenous paramagnetic contrast is individualized, but generally it is used. The principles of using these studies are reviewed in Chapter 201. Specific problem-driven protocols for computed tomography (CT) and magnetic resonance imaging (MRI) of the trachea and larynx are presented in Appendixes A and B, respectively.
Pros and Cons
Evaluation of Diseases of Uncertain Etiology
Inflammatory disease limited to the trachea could but usually will not mimic the initial presentation of cancer. Any condition, regardless of etiology, that is suspicious for deep infiltration or cancer should be studied primarily with CT if imaging is desired as part of the evaluation.
MRI might be useful in inflammatory conditions of the trachea; however, a significant proportion of MR studies will be of poor quality owing to motion artifacts, and such limited studies are less likely to add information that might alter medical decision making especially with regard to the tracheal and laryngeal skeleton. Supplemental MR study, in the limited situations where it might add meaningful incremental data, is best directed by CT findings to a localized area of interest where its strengths related to better soft tissue contrast resolution may be exploited.
CT and MRI of the diseased trachea must be evaluated not only for the effect of disease on the airway but also to determine the extent of spread beyond the trachea; cartilage involvement; and spread to adjacent structures including the hypopharynx, larynx, and esophagus. CT or MR images provide better information than the endoscopic examination about such tracheal wall involvement and spread beyond the trachea and even the airway itself when it is completely or nearly completely occluded.
Integrity of the Airway
Any imaging study of the trachea for a disease condition must be evaluated for its effect on the airway (Figs. 211.3 and 211.4). This is frequently the initial and main indication in the case of infectious and noninfectious inflammatory conditions, with the etiology being already known or at least highly suspected. The anatomic status of the airway, as well as the risk of any acute adverse complication, such as the potential for rapidly progressive airway obstruction or the potential for collapse, should be reported.
SPECIFIC DISEASE/CONDITION
Acute Viral Infections: Croup
Etiology
Croup is a viral laryngotracheitis and must be clinically differentiated from epiglottitis in children.
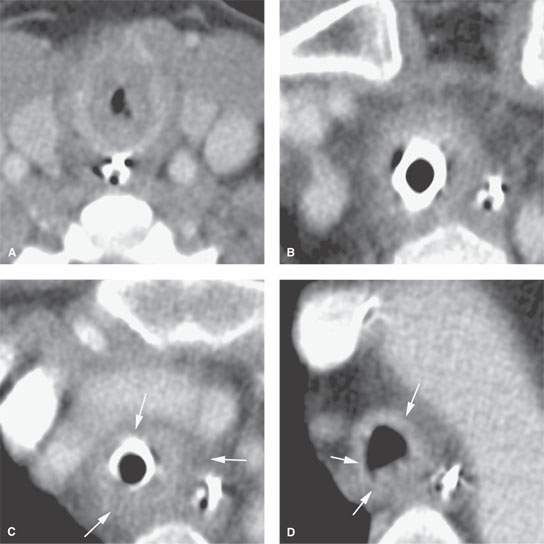
FIGURE 211.3. Computed tomography (CT) with contrast of a patient presenting with upper airway obstructive symptoms. The patient suffered from a predominately tracheal chondritis, the etiology of which was never established. The patient was treated for both infectious etiologies and possible autoimmune type disease. In (A), there is nearly complete obliteration of the subglottic airway. Suitable endoscopic examination was not possible, which led to this study. The additional CT sections in (B) and (C) show that the distal cervical trachea is abnormal. Both the endoluminal soft tissues and tracheal wall are swollen, and there is abnormal infiltration circumferentially around the trachea in the surrounding soft tissues that continues into the mediastinum in (C) (arrows). The trachea begins to return to normal in (D) just a few centimeters above the carina, but there is still abnormal thickening of its wall (arrows).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








