Pancreas Transplantation
Introduction
Diabetes mellitus (DM) is a very common disease, which affects approximately 2-6% of the general population; the overall incidence is increasing worldwide. It is currently the third most common disease and the fourth leading cause of death by disease in the USA. It is estimated that, by 2010, the number of people with DM will exceed 350 million. About 10% of DM patients have insulin-dependent diabetes mellitus (IDDM). The syndrome of IDDM includes abnormal glucose metabolism and specific microvascular complications that include retinopathy, nephropathy, and neuropathy. Intensive insulin therapy will improve glucose control; nevertheless, most patients will eventually develop some or all of these secondary complications.
DM is currently the leading cause of kidney failure and blindness in adults, the commonest cause of amputations and impotence, and one of the leading chronic diseases of childhood. Apart from the latest report on a small number of patients by the Edmonton group on consecutive successful allogenic islet cell transplantations,1 vascularized pancreas transplantation is the only available treatment of IDDM that can establish insulin independence, with normoglycemia and normal glycosylated hemoglobin levels for as long as the graft functions.
Unlike other organ transplantation, pancreatic transplantation is not considered a life-saving operation, and the recipients are subject to life-long immunosuppression. The Diabetes Control and Complications Trial (DCCT), showed the importance of euglycemia in preventing and controlling the progression of complications.2–4 Nevertheless, completely normal glycosylated hemoglobin can only be obtained by a pancreas transplant.
The first pancreatic transplant was performed by Kelly and Lillihei at the University of Minnesota in 1966. In the 1980s, developments in immunosuppression therapy and surgical management of pancreatic exocrine secretions combined with careful candidate selection resulted in dramatic improvements in both patient and graft survival. In the 1990s, the incorporation of additional new antirejection agents into the immunosuppression protocols resulted in a further decrease in the incidence of acute rejection.
Patient Selection
Patient selection for pancreatic transplantation involves a comprehensive multidisciplinary pretransplant evaluation with additional work-up tailored to the individual patient. Overall, the evaluation confirms the diagnosis of IDDM, determines the patient’s ability to withstand a major operation, establishes the absence of any exclusion criteria, and documents end-organ complications to study the effect of pancreas transplantation on the secondary complications of diabetes.
 Summary points:
Summary points:
Patient selection for pancreas transplants should include the following:
- Objective measures to exclude irreversible cardiac ischemia
- Exclusion of irreversible severe peripheral vascular disease
- Consideration that previous stroke and transient ischemic attacks increase postoperative risk
- As routine, ECG, stress thallium scan, coronary angiograms, Doppler examination of limbs
- Exclusion of chronic sepsis
Technical Aspects of Pancreas Transplantation
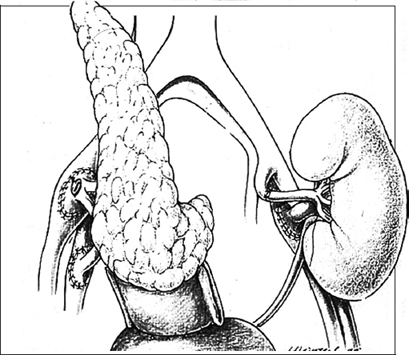
Advances in organ retrieval and preservation technology have played an important role in the improving results of pancreas transplantation. Most North American transplant centers have chosen vascularized pancreas transplantation with the duodenal segment method of bladder drainage as the procedure of choice, but an increasing number of centers have switched to exocrine drainage into the bowel to avoid the metabolic and urological complications of bladder drainage. The majority of pancreas transplants are performed in conjunction with a simultaneous renal transplant from the same donor through a midline intraperitoneal approach. The operation usually lasts from three to five hours, depending on whether the patient is having a pancreas alone or combined simultaneous kidney and pancreatic transplant (SKPT). Most pancreas transplants have been performed using the standard technique of endocrine drainage into the systemic venous circulation (iliac vein) and exocrine drainage into the urinary bladder (Fig. 13.1). A new technique of draining the endocrine secretion into the portal venous system in combination with enteric drainage of the exocrine secretions is gradually replacing the standard technique. The recipient’s native pancreas and kidneys are not removed.
Following operation, the patient usually spends two to three days in the intensive care unit and two to three weeks in the hospital. SKPT is associated with a greater morbidity than a kidney transplant alone, mainly due to reoperation, pancreas-specific morbidity, increased rejection episodes, and infections.5,6
Long-Term Outcome After Pancreas Transplantation
With newer immunosuppressive regimens and an optimized safe, standardized surgical procedure that has minimized technical complications related to exocrine secretions and graft thrombosis, the results of vascularized pancreas transplantation have improved significantly in the past decade. The one-year patient survival rate for all categories—SKPT, PAKT (pancreas after kidney transplant), and PTA (pancreas transplant alone)—is 95%, with an 85% one-year survival rate of pancreas graft after SKPT, 74% after PAKT, and 69% after PTA. The one-year kidney graft survival rate after SKPT is 91 %. Rejection accounts for 18 % of graft failures in the first year following pancreatic transplantation. The overall average pancreas graft survival rates for combined kidney-pancreas transplants at one, three, and five years are 83.6%, 72.9%, and 65.5% respectively. Results of pancreatic transplants are frequently updated and can be found on www.insulin-free.org./article/inp.htm.
Complications
Early Complications
Complications can arise shortly following pancreas transplantation, they include surgical complications such as vascular thrombosis, urinary leak, graft rejection, allograft pancreatitis, and intra-abdominal infection. Kidney allograft rejection can be used to guide treatment in SKPT patients as kidney graft rejection is believed to precede or parallel pancreatic rejection. The bladder drainage technique has allowed direct monitoring of pancreatic exocrine function, and urine amylase and cytology have both been used as noninvasive markers of early rejection.
Vascular thrombosis is the most common complication associated with pancreatic transplantation, with an overall rate of approximately 12%, of which 5% are arte-rialand7%venousinorigin(Fig. 13.2). Several donor risk factors for thrombosis have been identified, including old age and cardio-cerebrovascular diseases. Surgical related risk factors are left-sided implantation, arterial reconstruction, and portal vein extension. Surgical complications related to exocrine pancreatic drainage and allograft pancreatitis are usually due to technical errors (leak or fistula) or infection leading to fluid collections, pseudocysts, or abscesses surrounding the pancreatic graft. Reflux graft pancreatitis, hematuria, and bleeding are alsoquite common complications. Perioperativeantibacterial prophylaxis with imipenem-cilastatin alone or in combination with vancomycin, or with antibiotics chosen according to the results of duodenal culture, and antifungal and antiviral prophylaxis with fluconazole, nystatin, or clotrimazole, and aciclovir or ganciclovir, are recommended and have been shown to reduce the incidence of infective complications. The repeat laparotomy rate following pancreatic transplantation is 24-32 % in the USA. This is commonly for intra-abdominal infections, vascular thrombosis, and anastomotic leaks. Uncommon complications after pancreas transplantation have been reported, such as mesenteric arteriovenous fistula, iliac artery-bladder fistula, arterial mycotic aneurysm and rupture, urethral diverticula, and cytomegalovirus pancreatitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree