Liver Transplantation: Surgical Techniques
Introduction
In order to understand the techniques of liver transplantation a clear appreciation of the segmental anatomy of the liver is essential. Classification according to the Couinaud nomenclature1,2 is now generally accepted and it is possible to define the segments on both ultrasound3 and CT examination.3 This chapter begins with an introduction to liver anatomy relevant to surgical and radiological practice, including the common variants of hepatic vascular anatomy. The standard technique of liver transplantation and its various modifications are then described.
Liver Anatomy
An imaginary plane, the principal plane of the liver, which runs between the inferior vena cava (IVC) posteriorly and the gallbladder anteroinferiorly, separates the right and left lobes of the liver. The two lobes are defined by their blood supplies, which are the right and left branches of the hepatic artery and portal vein.4 The segmental anatomy of the liver can be appreciated by consideration of the hepatic venous drainage. The major part of the venous drainage of the liver is via the right, middle, and left hepatic veins, which emerge from the posterosuperior aspect of the liver and drain into the IVC, the middle and left veins often having a confluent orifice.5 The posterior part of the liver that is in contact with the IVC (segment 1, the caudate lobe) drains via short caudate tributaries directly into the IVC.
The middle hepatic vein lies between the right and left lobes in the principal plane. The left hepatic vein lies along the line of the falciform ligament in a plane that separates the left lateral segment (segments 2 and 3) from the remainder of the left lobe (segment 1 and segment 4, the quadrate lobe). The right hepatic vein lies in a plane that divides the right lobe into segments 5 and 8 anteriorly and segments 6 and 7 posteriorly. The numbering of the segments runs roughly clockwise when the liver is viewed in the anatomical position (Fig. 8.1).
The portal vein lies in front of the IVC on the inferior surface of the liver.6 The portal vein is formed by the confluence of the superior mesenteric vein and the splenic vein behind the pancreas and divides into its main right and left branches at the hilum of the liver.

Fig. 8.1 Segmental liver anatomy based on the Couinaud classification (segments 1-8). The description is based on portal segments, with each segment having its own blood supply (arterial, portal, hepatic venous), lymphatics, and biliary drainage, allowing surgical resection of each segment. (From Couinaud 19571)
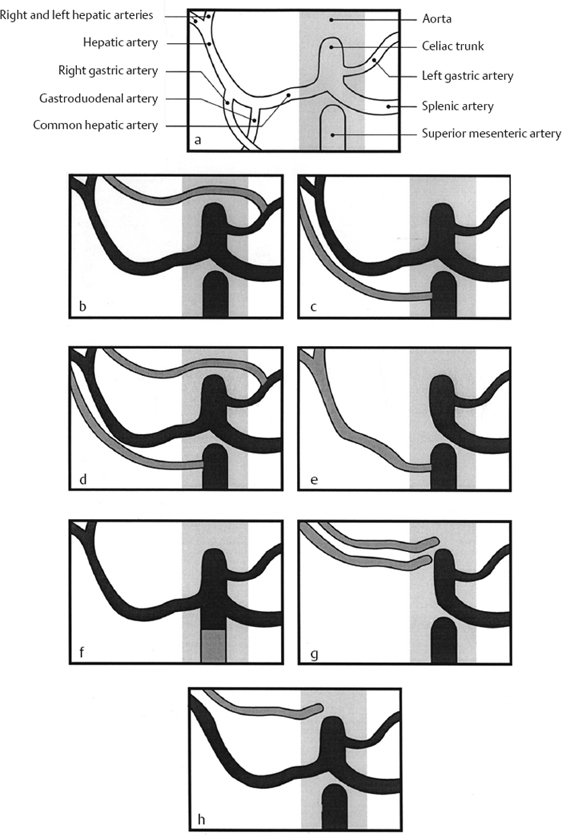
The arterial blood supply of the liver is via the celiac trunk and the common hepatic artery, which becomes the hepatic artery proper after giving off the gastroduodenal and right gastric arteries (Fig. 8.2a). The hepatic artery lies anterior to the left side of the portal vein and divides into right and left branches at the hilum.
Variations in the hepatic arterial anatomy are common (Fig. 8.2).7 There may be an accessory left hepatic artery arising from the left gastric artery and entering the liver through the lesser omentum (14% of individuals, Fig. 8.2b); in some cases this may completely replace the conventional left hepatic artery. There may be an accessory right hepatic artery arising from the superior mesenteric artery and entering the liver by passing behind the superior mesenteric vein and to the right of the portal vein (10 %, Fig. 8.2c); again, in some cases this may replace the conventional right hepatic artery. Both accessory/replaced left and right arteries may be present in the same individual (4%, Fig. 8.2d). Biliary radicals drain into the right and left hepatic ducts which then form the common hepatic duct.8–10
This becomes the common bile duct after the entry, at a variable level, of the cystic duct from the gallbladder. The common hepatic and common bile ducts lie anterior to the portal vein and to the right of the hepatic artery.
 Summary point:
Summary point:
- The principal plane of the liver, which runs between the inferior vena cava posteriorly and the gallbladder anteroinferiorly, separates the right and left lobes of the liver.
- Variations in the hepatic arterial anatomy are common.
Standard Orthotopic Cadaveric Liver Transplantation
The liver, unlike the kidney, is almost always transplanted in an orthotopic position, i.e., in its usual anatomical site: the diseased liver is removed and the transplanted organ takes its place.11 The firm attachment of the retrohepatic IVC to the liver by the caudate veins means that the most straightforward way to remove the liver is to take the retrohepatic IVC with it, having already divided the common bile duct, hepatic artery, and portal vein. A very similar operation will have previously been performed in the cadaveric organ donor.
There are therefore five structures which require anastomosis between the recipient and the graft: the suprahepatic IVC, the infrahepatic IVC, the portal vein, the hepatic artery, and the common bile duct12 (Fig. 8.3). The above vessels are clamped from the time that the diseased liver is removed until the vascular anastomoses to the graft are completed. Clamping of the infrahepatic (suprarenal) IVC results in congestion in the lower half of the body and the kidneys. Patients in poor condition may not tolerate the resultant diminished venous return to the heart, and venous congestion of the kidneys may also result in renal dysfunction in the early postoperative period.13 Similarly, clamping of the portal vein may result in worsening of portal hypertension, congestion of the bowel, and increased blood loss during the procedure. In order to minimize these problems, it is common practice to perform veno-venous bypass: cannulae are inserted into the portal vein and a common iliac vein (via the femoral vein), and blood is returned to the heart via a bypass pump connected to a cannula in the left axillary or internal jugular vein.
All anastomoses are performed in an end-to-end fashion (Fig. 8.3). A modification of end-to-end anastomosis is frequently used for the hepatic arterial anastomosis, which often has a small caliber.14 The diameter of the cut end of an artery can be increased if the vessel is divided at the origin of a branch. This produces a “branch patch”, the most commonly used being a gastroduodenal branch patch of the common hepatic artery. Branch patches may be used on both recipient and graft arteries and result in a slight increase in diameter of the arterial lumen at the point of anasto-mosis.15
The gallbladder is removed from the transplanted liver after implantation. This is in order to avoid potential post-transplantation gallbladder complications due to stasis in a denervated gallbladder. The common bile duct of the donor liver is usually anastomosed to the common bile duct of the recipient. This is referred to as a “duct-to-duct anastomosis.” A T tube may be placed across the anastomosis when there is a significant size discrepancy between the donor and the recipient ducts. As caliber differences are fairly common, the postoperative appearance of a graft bile duct larger in caliber than the recipient duct does not necessarily imply biliary obstruction.
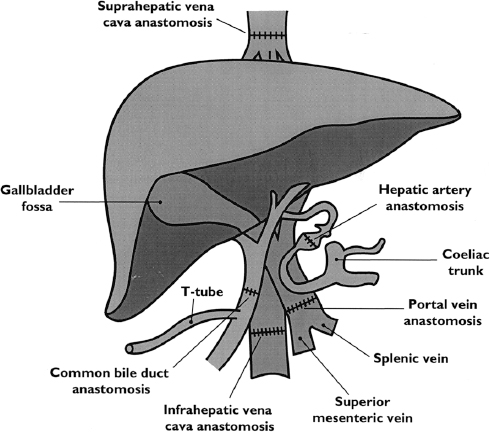
Fig. 8.3 Donor/recipient sites for vascular and biliary anastomoses
 Summary point:
Summary point: