Active pancreatic bleeding
Pancreatic laceration or facture
Pancreatic contusion or hematoma
Focal or diffuse enlargement or edema of the gland
Low or heterogeneous pancreatic attenuation
Dilatation or discontinuity of the pancreatic duct
Edema and stranding of peripancreatic fat
Thickening of the anterior pararenal fascia
Fluid in the lesser sac, transverse mesocolon, and anterior and posterior pararenal spaces or surrounding the SMA
Pseudocyst or abscess
Fluid between the posterior pancreas and splenic vein
Injuries to adjacent structures
Free intraperitoneal fluid
SMA superior mesenteric artery
Conventionally, ERCP has been regarded as the gold standard in the evaluation of pancreatic duct. However, due to the invasive nature of ERCP, it is not widely accepted as an appropriate screening test for pancreatic trauma. MRCP has been reported as attractive alternative modality to evaluate the patency of pancreatic duct. Some investigators demonstrated that the use of secretin stimulation improved the delineation of ductal morphologic features on MRCP; therefore it could provide additional useful information about duct integrity. However, the exact usefulness of MRCP in acute pancreatic injury has not yet been established since most studies on the topic had limitations of small sample size and retrospective nature. More experience and studies are required to confirm the usefulness of MRCP in acute pancreatic injury.
21.1.1.1 Grading of Pancreatic Injury
Among various classification systems proposed for pancreatic injury, a grading scale proposed by the American Association for the Surgery of Trauma (AAST) is the most widely accepted (see Table 21.2). This scheme addresses the significance of more complex injuries to the pancreas according to the location of the injury and the integrity of the ampulla and main pancreatic duct. It also enables to correlate with other organ injury scales which allow the prediction of a patient’s prognosis.
Table 21.2
American Association for the Surgery of Trauma pancreatic injury scale
Gradea | Type of injury | Description of injury |
|---|---|---|
I | Hematoma | Minor contusion without duct injury |
Laceration | Superficial laceration without duct injury | |
II | Hematoma | Major contusion without duct injury or tissue loss |
Laceration | Major laceration without duct injury or tissue loss | |
III | Laceration | Distal transection or parenchymal injury with duct injury |
IV | Laceration | Proximal (to right of SMV) transection or parenchymal injury involving ampulla |
V | Laceration | Massive disruption of pancreatic head |
21.1.2 Differential Diagnosis: Pseudopancreatitis
Several studies have been published to report an abnormal CT finding of intra- and peripancreatic fluid in patients without clinical and laboratory evidence of pancreatic injury, pancreatitis, or pancreatic disease. The reported causes of this phenomenon comprise severe trauma of extremities, major burn injury, and hypovolemic shock. Although the exact mechanism of pseudopancreatitis was not well known, a hypothesis was proposed that it might be a consequence of mild ischemic pancreatic injury caused by hypovolemic shock and followed by overhydration.
21.2 Post-treatment Complication
21.2.1 Post-operative Complication
For the past two decades, with technical advances and centralization of care, pancreatic surgery has progressed into a safe procedure with mortality rates of less than 5 %. However, postoperative complication rate with reported range from 30 to 50 % is still considerable. Pancreatic surgery has similar complications which confront to other major abdominal surgery, e.g., anastomotic leakage, intra-abdominal abscess, wound infection/dehiscence, hemorrhage, and medical complications such as cardiac problems, cerebrovascular accidents, respiratory distress, and renal and hepatic dysfunction. Common and relatively specific complications that attend pancreatic surgery include pancreatic fistula and delayed gastric emptying.
Pancreatic fistula occurs in 5–30 % of patients undergoing pancreaticoduodenectomy. This wide range is probably due to different definitions used. Although most pancreatic fistula runs a benign course, it potentially leads to postoperative mortality if it results in retroperitoneal sepsis with abscess formation and/or destruction of the surrounding tissues and blood vessels. A fluid collection seen on CT around the pancreaticojejunostomy site and in the pancreatic bed and depiction of air bubbles in the fluid are known to be feasible findings for diagnosing pancreatic fistula. Since pancreatic leakage is basically a clinical diagnosis of persistent drainage of amylase-rich fluid, clinico-radiologic correlation should always be followed when there is a suspicion of pancreatic leakage.
Delayed gastric emptying is also a common complication of which incidence ranges from 20 to 60 % of patients. It is notable that delayed gastric emptying is closely associated with other postoperative pathologic conditions such as pancreatic fistula and postoperative acute pancreatitis. However, the radiologic evaluation of postoperative delayed gastric emptying has not been well established in the literature.
21.2.2 Post-procedural Complication
Several diagnostic and therapeutic procedures might cause complications in the pancreas. Acute pancreatitis is one of the most common complications of ERCP. Although ultrasonography-guided percutaneous or endoscopic biopsy has been established as a feasible and safe method to confirm the unresectable pancreatic cancer, it can also result in complications such as fever, hemorrhage, acute pancreatitis, and pseudocyst formation.
21.3 Summary
1.
Blunt traumatic pancreatic trauma is uncommon accounting for less than 2 % of all cases of blunt abdominal trauma.
2.
Since coexisting injuries can affect various organs adjacent to the pancreas, careful examination should be accompanied for injuries.
3.
The diagnostic performance of CT in detecting pancreatic trauma is still on debate.
4.
Repeated scan in 12–24 h should always be considered if there is a suspicion for pancreatic injury.
5.
ERCP is the gold standard in the evaluation of pancreatic duct.
6.
MRCP might be useful in the evaluation of acute pancreatic injury although more experience and studies are required.
7.
As various iatrogenic procedures might affect the pancreas, radiologists should always concern the possibility of the pancreatic injury in image interpretation.
21.4 Illustrations: Trauma and Post-treatment Complications of the Pancreas
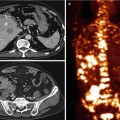
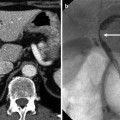
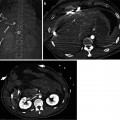
21.4.1 Pancreatic Contusion

Fig. 21.1
Pancreatic contusion in a 28-year-old male. (a) Contrast-enhanced axial CT shows hypoattenuating area (arrowheads) at the pancreas. (b




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree