Gradea
Injury type
Injury description
AISb-90
I
Hematoma
Subcapsular, <10 % surface area
2
Laceration
Capsular tear, <1 cm parenchymal depth
2
II
Hematoma
Subcapsular, 10–50 % surface area; intraparenchymal, <10 cm in diameter
2
Laceration
Capsular tear, 1–3 cm parenchymal depth, <10 cm in length
2
III
Hematoma
Subcapsular, >50 % surface area or expanding; ruptured subcapsular or parenchymal hematoma; intraparenchymal hematoma >10 cm or expanding
3
Laceration
>3 cm parenchymal depth
3
IV
Laceration
Parenchymal disruption involving 25–75 % of a hepatic lobe or 1–3 Couinaud’s segments within a single lobe
4
V
Laceration
Parenchymal disruption involving >75 % of a hepatic lobe or >3 Couinaud’s segments within a single lobe
5
Vascular
Juxtahepatic venous injuries (i.e., retrohepatic vena cava or central major hepatic veins)
5
VI
Vascular
Hepatic avulsion
6
10.1.5 Delayed Complications in Blunt Liver Trauma
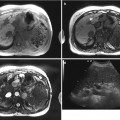
With the growing trend toward nonoperative management of complex hepatic injuries, the frequency of delayed complications has increased up to 10–25 %. Thus, follow-up CT is recommended for monitoring of any conservative management of major hepatic injury to detect and treat delayed complications. Most delayed complications can be managed with interventional procedures.
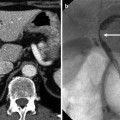
10.1.5.1 Delayed Hemorrhage
Delayed hemorrhage is the most common complication of nonoperatively managed blunt hepatic injury. Hemorrhage may occur due to an increase in the extent of the laceration or rupture of the pseudoaneurysm of the hepatic artery or portal vein. Asymptomatic arterial pseudoaneurysms should be treated as soon as possible due to the high possibility of rupture. Bleeding should be suspected in patients with new-onset right upper quadrant pain or decreasing levels of hemoglobin.
10.1.5.2 Abscess
Hepatic abscess is the most common complication of operative treatment and can occur in patients with high-grade injuries. It appears as focal fluid attenuation with newly developed gas bubbles or an air-fluid level in the injured liver parenchyma, which may demonstrate an enhancing rim. Subcapsular and intraparenchymal hematoma can also be infected. Percutaneous catheter drainage has now become the treatment of choice.
10.1.5.3 Biloma
Bile leakage from a hepatic laceration is common but mostly limited and transient without sequelae. Bilomas, on the other hand, are an uncommon complication. A well-circumscribed, low-attenuating fluid collection in the intraparenchymal or perihepatic space with progressive growth strongly suggests biloma. Most traumatic bilomas resolve spontaneously. Complicated bilomas that increase in size and cause symptoms or become infected can also be successfully treated with percutaneous catheter drainage.
10.1.6 Penetrating Injury of the Liver
The liver is the most frequently injured intra-abdominal solid organ from penetrating trauma. Knife stabbings usually cause superficial lacerations, whereas gunshots generally cause injury from capsule to capsule with irregular lacerations and parenchymal damage.
10.1.7 Iatrogenic Injury of the Liver
Diagnostic and therapeutic interventional procedures can produce various complications including hepatic capsular tear, subcapsular or intraparenchymal hematoma, hepatic arteriovenous fistula, bile leaks, hemobilia, and hemoperitoneum.
10.2 Postoperative Changes of the Liver
10.2.1 Terminology of Liver Resection
Liver resections are grossly divided into anatomical and nonanatomical resections. Anatomical resections indicate the removal of functional liver units or segments. The standardized terminology for anatomical liver resections was presented by the terminology committee of the international hepato-pancreato-biliary association (The Brisbane 2000 terminology of liver anatomy and resections). This system divided the liver into two hemilivers, four sections, and eight segments, assigned anatomical terms to divisional anatomy, and named surgical resection according to anatomical terms (see Table 10.2 and Fig. 10.21). Nonanatomical resections are mostly smaller local wedge resections performed to remove a hepatic focal lesion, usually a superficial one. Anatomical and nonanatomical resections are often used in combination.
Table 10.2
Nomenclature for hepatic anatomy and resections
Anatomical term | Couinaud segments | Term for surgical resection | |
|---|---|---|---|
First-order division anatomy | Right hemiliver or right liver | Sa5–8 (+/− S1) | Right hepatectomy or right hemihepatectomy |
Left hemiliver or left liver | S2–4 (+/− S1) | Left hepatectomy or left hemihepatectomy | |
Second-order division anatomy | Right anterior section | S5, 8 | Right anterior sectionectomy |
Right posterior section | S6, 7 | Right posterior sectionectomy | |
Left medial section | S4 | Left medial sectionectomy or segmentectomy 4 | |
Left lateral section | S2, 3 | Left lateral sectionectomy or bisegmentectomy 2,3 | |
Right hemiliver plus left medial section | S4, 5–8 (+/− S1) | Right trisectionectomy or extended right hepatectomy or extended right hemihepatectomy | |
Left hemiliver plus right anterior section | S2–4, 5, 8 (+/− S1) | Left trisectionectomy or extended left hepatectomy or extended left hemihepatectomy | |
Third-order division anatomy | Segments 1–8 | Any one of S1 to S8 | Segmentectomy |
2 contiguous segments | Any two of S1 to S8 in continuity | Bisegmentectomy | |
10.2.2 Normal Postoperative Findings
10.2.2.1 Early Postoperative Period
Small fluid collections and transient accumulation of hematoma or bile along the resection margin are common findings and usually regress over time. Pleural effusions, particularly on the right side, are also common. A small area of low attenuation around the resection plane may be seen on contrast-enhanced CT, which presumably represents the sequelae of local trauma, and gradually regresses. Metallic surgical clips may be seen along the resection margins. Drain tubes are marked with radiopaque lines. Artificial hemostatic agents applied in the resection site appear as areas of high or mixed attenuation with or without punctate air bubbles mimicking abscess or complicated hematoma; thus, appropriate operative history should be sought.
10.2.2.2 Late Postoperative Period
The remnant liver after major hepatic resection undergoes regeneration. An approximately 60 % volume increase of the remaining left hemiliver occurs in the first postoperative week. In case of the cirrhotic liver, enlargement may not be seen. After right hemihepatectomy, the left lobe is elliptically enlarged with displacement of the falciform ligament to the right. The caudate lobe may also show mild hypertrophy. The bowel and omentum fill the space of the resected right lobe and the right kidney can be elevated. After left hemihepatectomy, the right lobe enlarges roundly with displacement of the porta hepatis. The stomach and colon occupies the left hepatic fossa and the right kidney can be displaced inferiorly. Preexisting focal lesions may change in configuration according to parenchymal hypertrophy. The spleen may also increase in size due to altered portal venous hemodynamics.
10.2.3 Imaging of Postoperative Surgical Complications After Hepatic Resection
General postoperative complications after abdominal surgery include intra-abdominal infection, wound complications, bleeding, or hematoma. In cases of partial hepatectomy, the complex biliary and vascular anatomy of the liver adds the following complications.
10.2.3.1 Biliary Complications
The main biliary complications associated with hepatic resection are bile leaks and biliary obstruction. Common sites of bile leaks include the bile duct stump, the biliary-enteric anastomosis, common hepatic ducts, and T-tube insertion sites. Bilomas, or extrabiliary bile collections, are seen as well-defined low-attenuating fluid collections around the resection margin or porta hepatis. If the leaked bile drains effectively, fluid collections cannot be observed. Bile in the drain tube, percutaneous aspiration of bile content, or visualization of bile leakage on ERCP, PTC, Tc-99 m DICIDA scan, or Gd-EOB-DTPA-enhanced MR can confirm the bile leak. Biliary obstructions can occur due to postoperative fibrosis at the bile duct stump or unexpected bile duct ligation.
10.2.3.2 Vascular Complications
Thrombotic occlusions of the hepatic artery, portal vein, or hepatic vein are uncommon, but should be considered in patients with deterioration of liver function in the early postoperative period. It can be diagnosed with contrast-enhanced CT or MR showing nonopacification of vessels. Doppler ultrasound is another useful diagnostic modality for hepatic vascular thrombosis.
10.3 Summary
1.
The liver is the second most frequently injured abdominal organ from blunt trauma. MDCT and interventional procedures play important roles in the nonoperative management of patients with blunt liver trauma.
2.
MDCT for trauma patients should be acquired with intravascular contrast materials to evaluate vascular extravasation such as active bleeding which typically appears as irregular or flame-like high-attenuating foci of extravasated intravenous contrast materials that increase in extent on successive enhanced CT scans with persistently high attenuation.
3.
Laceration of large hepatic vein is rare but potentially lethal due to profound hemorrhage. Right hepatic vein avulsion from the inferior vena cava or retrohepatic vena cava laceration should be suspected on CT when hepatic lacerations extend into the proximal right hepatic vein or inferior vena cava with a large amount of hemorrhage behind the right hepatic lobe or when active bleeding is seen from those veins.
4.
Delayed complications of the blunt hepatic injury such as delayed hemorrhage, abscess, and biloma are not uncommon. Clinical suspicion should prompt reevaluation by CT scan.
5.




Small fluid collection after partial hepatectomy is the most common early postoperative findings. After regeneration of the remaining liver, the configuration of the upper abdominal organs changes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree