Fig. 40.1
Non-contrast enhanced head computed tomography (CT) in a patient after motor vehicle collision displayed in bone algorithm shows fracture through the right occipital bone (arrow)
Epidural Hematomas
An epidural hematoma (EDH) is present in 1–4 % of patients with TBI. The epidural space is located between the dura and the calvarium and can accumulate extravasated blood from injured blood vessels, most commonly arteries (85 %), such as the middle meningeal artery. An underlying fracture is present in more than 90 % of cases. Typically, EDHs appear as biconvex, hyperdense, extra-axial collections on non-contrast enhanced CT examinations (Fig. 40.2). They do not cross suture lines except at the level of the sagittal suture, where the dura does not invest the suture due to the presence of the superior sagittal sinus. Unlike subdural hematomas (SDH), an EDH can cross dural reflections such as the falx cerebri or tentorium cerebelli. Mixed density or heterogeneous EDHs have been shown to have a worse prognosis than more homogenous EDHs, due to the presence of active bleeding with hypodense areas representing unclotted blood; this has been termed the “swirl sign” (Fig. 40.3).

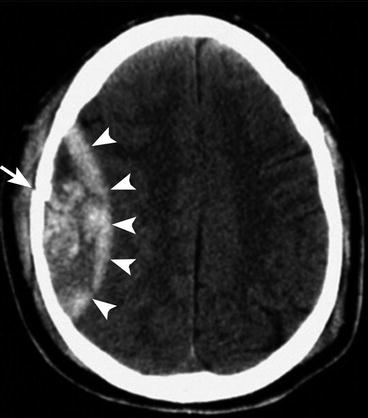

Fig. 40.2
Small epidural hematoma along the posterior left temporal lobe causing mass effect on underlying brain parenchyma (arrow)
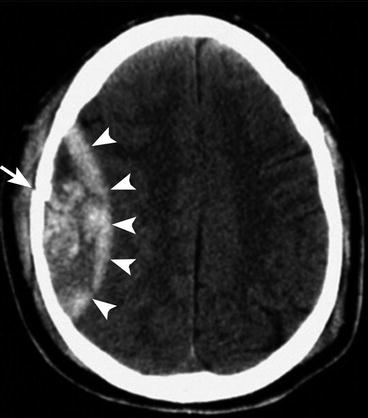
Fig. 40.3
Non-contrast enhanced head computed tomography (CT) in a patient after a motor vehicle collision demonstrates a high density, biconvex epidural hematoma (arrowheads) deep to the parietal skull fracture (arrow). Areas of hypodensity within the epidural hematoma are likely related to areas of active bleeding
Following decompressive craniectomies, small EDHs remote from the surgical site may dramatically increase in size. This is thought to relate to release of a tamponade effect generated by preoperative elevated intracranial pressure.
Subdural Hematomas
Ten to twenty percent of patients with TBI will present with a subdural hematoma. The subdural space is a potential space located between the inner meningeal layer of the dura and the arachnoid mater. As opposed to EDHs, the majority of SDHs are venous in origin, the result of traumatic injury to bridging cortical veins that traverse the subdural space. They are less frequently associated with skull fractures compared with EDHs. The majority of SDHs are supratentorial and occur along the cerebral convexities, tentorium cerebelli or falx cerebri. On non-contrast CT they appear as crescentic extra-axial collections that cross suture lines and often span an entire hemisphere. Internal characteristics of SDHs on CT however vary based on whether they are acute, subacute or chronic. Acute SDH (<1 week) are typically homogenously hyperdense (Fig. 40.4). In patients with underlying anemia, acute SDHs can appear iso- or hypointense. Like EDHs, if there is active bleeding, acute SDHs can also appear heterogeneous.
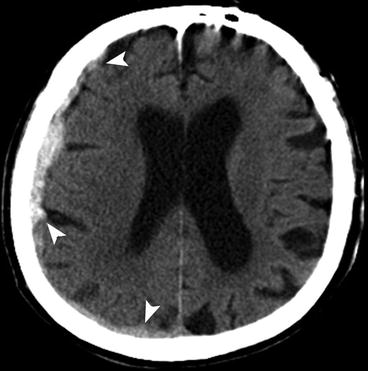
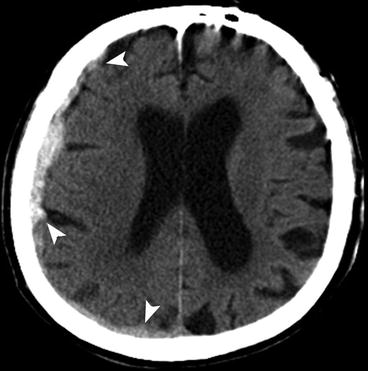
Fig. 40.4
Non-contrast enhanced head computed tomography (CT) in a patient after a fall shows a subdural hematoma (arrowheads) along the right convexity causing mild mass effect on underlying right cerebral hemisphere with sulcal effacement. High density suggests more acute blood products
Over time, subdural blood breaks down and cellular elements are removed causing a progressive decrease in attenuation. Subacute SDHs (1–3 weeks) often have internal density on a spectrum that includes an isodense phase. The isodense collection can be difficult to recognize on non-contrast medium enhanced CT (Fig. 40.5). Clues to the presence of an isodense SDH include white matter buckling, medial displacement of the gray-white junction and presence of a mass effect (midline shift, sulcal effacement, compression of ipsilateral ventricle). As the collection ages, it will eventually become homogeneously hypodense. Chronic SDHs (>3 weeks) can sometimes contain adhesions and membranes, producing multiple compartments.
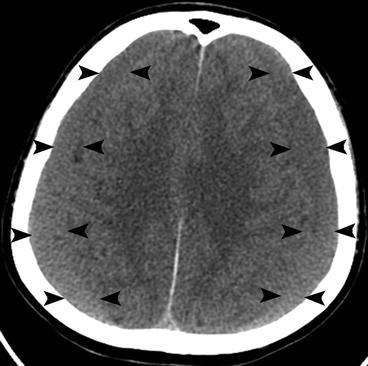
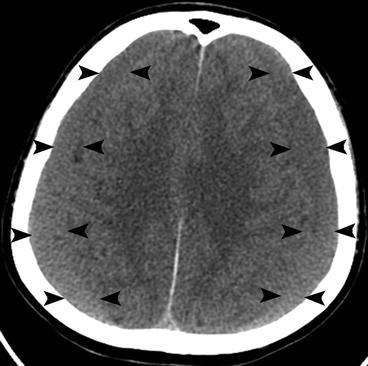
Fig. 40.5




Non-contrast enhanced head computed tomography (CT) in patient several weeks after fall shows intermediate density, crescent shaped collections (arrowheads) overlying both cerebral hemispheres consistent with subacute subdural hematomas. As the blood products become reabsorbed, the hematomas become isodense to normal gray matter and may be difficult to visualize. Note the presence of balanced mass effect on both cerebral hemispheres
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree