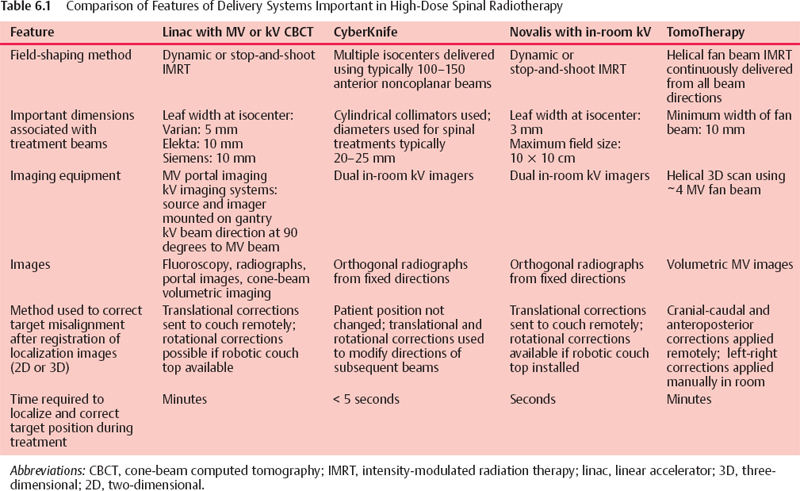
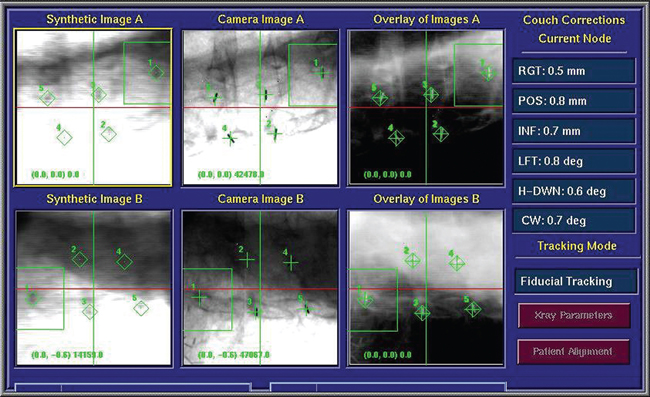
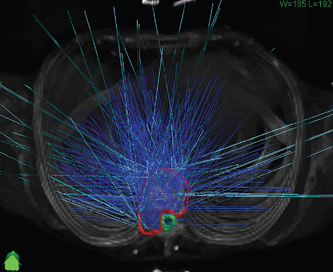
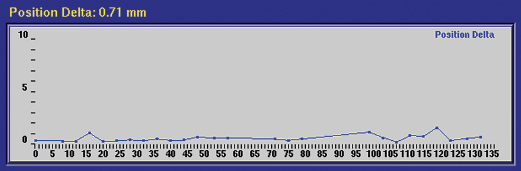
6 Essential requirements for a delivery system to be used for spinal treatment include the following: For the irradiation of deep-seated tumors of the spine, a variety of treatment machines that use linear accelerators (linacs) to generate high-energy photons are now in use. The most common radiosurgery systems are the Novalis system from BrainLab AG (Feldkirchen, Germany) and the CyberKnife system from Accuray Inc. (Sunnyvale, California). Novalis uses a micro-multileaf collimator for beam shaping with one isocenter, whereas Cyberknife employs a robotic computer-controlled gantry with multiple isocenters. Other sophisticated arrangements of a linac-mounted gantry with various image-guidance methods are being developed. Another system called Hi Art, from TomoTherapy Inc. (Madison, Wisconsin), features a 6 MV linac mounted on a computed tomography (CT)–like gantry. The imaging systems associated with the various treatment machines vary considerably. Some are capable of three-dimensional (3D) volumetric imaging; others are capable of rapidly verifying target position during treatment. Implanted fiducial markers may also be required for some patients, depending on the imaging technique used. Because of the close proximity of the spinal cord, even small patient movements that may occur after the final pretreatment imaging could result in the delivered dose to the spinal cord being higher than that planned. It is therefore important to be able to verify in 3D the target position at regular times during dose delivery. On a conventional linac, this can be done by stopping treatment and acquiring either a pair of localization images taken at different gantry angles or a cone-beam scan. Delivery using the TomoTherapy machine would be done in several passes. These can be interleaved with passes using the imaging beam. Therapy machines equipped with in-room imaging systems are capable of acquiring a pair of radiographs in a few seconds. When coupled with a means of rapidly registering the radiographs with the corresponding reference images and automatically implementing the corresponding correction, in effect the system can compensate for any small movements the patient may make during treatment. The clinical effort required to localize the target during treatment, then correct the patient position, depends on the treatment delivery platform. Careful patient immobilization will reduce the chances of movement during dose delivery, especially necessary because frequent target position verification is slow and time consuming. Clinical procedures differ widely. Table 6.1 compares features important to high-dose spinal radiotherapy for four different delivery systems. The remainder of this chapter describes some of the clinical experiences gained from two centers, each of which has been using radiosurgery to treat patients with paraspinal disease for 6 years or more. Although the two centers use very different treatment platforms, a CyberKnife and a conventional linac equipped with kV imaging, both perform hypofractionated and high-dose (24 Gy) single-fraction treatments. Each has developed techniques and clinical procedures necessary to safely deliver these complex treatments. The CyberKnife is an image-guided whole-body stereotactic radiosurgery system that consists of a 6 MV compact linac mounted to a robotic arm that is coupled through a control loop to a digital diagnostic x-ray imaging system. The robotic arm can point the radiation beam anywhere in space with six degrees of positioning freedom, without being constrained to a conventional isocenter.1–4 The CyberKnife was developed to overcome the geometrical limitations of gantry-based systems and to eliminate the need for application of invasive frames. Figure 6.1 depicts the basic components of the CyberKnife: To ensure safe delivery of high doses of radiation to spinal tumors, the position of the tumor needs to be tracked continually throughout the radiosurgery procedure. The CyberKnife system’s software is capable of tracking spinal tumors based on fiducial markers implanted in or near the tumor or by registering the position of one or two vertebrae close to the tumor. These two different techniques are described briefly below. Prior to treatment, each patient is implanted with four to six fiducial markers, which act as radiographic landmarks for the image guidance system. The fiducials are 0.8 x 5 mm cylindrical gold seeds or 2 x 6 mm stainless steel screws. They are typically implanted percutaneously in or near vertebrae under fluoroscopic guidance; the pedicles are the most common location. By placing fiducials in bony structures, one can significantly reduce the chance of fiducial migration. Three fiducials are necessary to define a full spatial transformation in all six degrees of freedom of target translation and rotation. Fiducials are implanted rostrally and caudally to the lesion so that the tumor is approximately centered within them. They are placed such that they are 2 cm or more apart and arranged in a noncoplanar configuration. For spine radiosurgery, rotational tracking accuracy can be important; therefore, we aim to use at least four fiducials because four fiducials yield much better tracking accuracy than three, whereas more than five fiducials give little further improvement5 (Fig. 6.2.) Following the implantation of fiducial makers, the patient returns for the planning CT. The patient is placed in a supine position in a conformal alpha cradle or Vac-Lok (MEDTEC, Orange City, Iowa) bag during CT scanning as well as during treatment. CT images are acquired with a slice thickness of 1.25 mm to include the lesion of interest as well as the fiducials. Because the fiducial markers are 5 mm or longer, they are visible in one to five consecutive slices, depending on their orientation. During treatment planning, the fiducials are located and their positions identified in three dimensions on the CT dataset. On the day of treatment, the patient is positioned supine in the same immobilization device that was used for the CT scan study. Two diagnostic orthogonal x-ray images (“live” images) are taken synchronously using the x-ray sources mounted to the ceiling and the flat-panel detectors positioned opposite the sources. CyberKnife tracking software processes the live images and extracts coordinates of the fiducial makers, then compares them to the position of the fiducials in digitally reconstructed radiographs (DRRs). Discrepancies between the two sets of values are reported as “couch corrections” to the operator. The operator can use these values to move the couch remotely from the operating console room. The patient is positioned with six degrees of freedom, three translations (inferosuperior, anteroposterior, and left/right) and three rotations (roll, yaw, and pitch). Once the fiducial markers are identified and verified by the operator at the beginning of the treatment, the determination of the patient position is a completely automated process. It takes only 2 to 4 seconds to produce a pair of orthogonal images and determine the patient position. It typically takes 10 to 20 minutes to set up a patient, although one may sometimes have difficult setups that take longer. For example, visualization of the fiducial markers in live images may prove to be a difficult task when large patients are imaged due to the limited penetrating power of the diagnostic x-ray sources. Figure 6.1 The main components of the CyberKnife robotic radiosurgery system: compact 6 MV X-band linear acceleratorlinac mounted to a robotic arm; two flat-panel in-floor x-ray detectors positioned opposite to the diagnostic x-ray sources mounted to the ceiling; and a robotic treatment couch with six degrees of freedom. (Courtesy of Accuray Inc., Sunnyvale, California.) Figure 6.2 A snapshot from the CyberKnife console computer taken during treatment of a patient with a spinal lesion. The synthetic images are digitally reconstructed radiographs (DRRs) generated from the patient’s computed tomography scan. The “diamonds” in the DRRs indicate the position of the gold markers. The camera images are the near-real-time x-ray images taken during the treatment. The green crosses in these images depict the positions of the gold fiducial markers as determined by real-time automatic image-processing algorithms. “Couch corrections” indicate how much one needs to move the couch to set up the patient exactly as he or she was scanned. Note that these corrections are six dimensional (three translations and three rotations). Once the initial setup is complete, radiation treatment may commence. A typical CyberKnife treatment has 100 to 150 beams6,7 (Fig. 6.3). Each beam enters from a different trajectory and typically has 200 monitor units (MU) or less. Because the linac has a dose rate of 600 MU/min, it takes 20 seconds or less to deliver the dose associated with each beam. The patient position can be verified by imaging the patient before the dose for each beam that is delivered. In this fashion, CyberKnife can continually correct for any deviation in patient position from the planning CT throughout the treatment. Figure 6.4 shows the changes in patient position during a spine radiosurgery treatment for a patient with a lesion at L4. Note that the patient position has deviated from the planning CT position by only 0.71 mm based on the last diagnostic x-ray image taken. However, because the robot moves the radiation beam to compensate for this deviation, in theory, the targeting error is reduced to its residual systematic component. For static targets such as spinal lesions, the CyberKnife system has been shown to have overall submillimeter radiation delivery accuracy.8–10 The CyberKnife robot can move the radiation beam to compensate for patient movements of up to 1 cm along each axis. The robot can also rotate the beam to compensate for target rotations of up to 1 degree about each axis. If the patient movement exceeds these limits, the system automatically turns off the radiation beam, and the treatment can only be resumed after the patient is moved back into the ideal position. The typical treatment time for a single-fraction radiosurgical procedure is 30 to 60 minutes. Figure 6.3 Beam directions for a plan of a patient with a lesion at T9. Beams with nonzero dose are shown in cyan. The tumor and spinal cord are outlined in red and green, respectively. This plan had 147 beams. Figure 6.4 “Position delta” is the deviation of the patient’s position during treatment from the planning computed tomography position. The vertical axis shows the deviation in millimeters, and the horizontal axis indicates the beam number. Position delta was 0.71 mm when this patient was imaged for the last time. The patient moved only a few millimeters throughout the treatment, which is typical of most spine treatments.
Treatment Delivery
 Clinical Experience from the University of Pittsburgh Medical Center
Clinical Experience from the University of Pittsburgh Medical Center
Spine Tracking
Six-Degree Fiducial Tracking

Six-Degree Skeletal Structure Tracking
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree