12 The clinical application of spine radiosurgery has been rapidly evolving. There is ample evidence to support integrating this modality into the treatment of spinal tumors, both malignant and benign. To maximize a successful clinical response to spine radiosurgery while maintaining a low toxicity profile, it is critical to analyze both the patterns of failure and the complications of this treatment. Because of the steep dose gradient and often small target volumes, the patterns of failure must be carefully correlated to the dosimetry profile of each case. There is currently a paucity of information regarding the patterns of failure and associated complications of spine radiosurgery, especially in clinical series with long-term follow-up. Nevertheless, the knowledge of such treatment failures and complications will help to better determine the role of radiosurgery in different clinical situations and ultimately determine the extent of the use of radiosurgery for spinal tumors. In this chapter, the patterns of clinical failures as well as the neural and non-neural complications of spine radiosurgery will be described. Treatment failures after spine radiosurgery can be divided into three categories. In-field failure refers to tumor regrowth inside the treatment volume as seen on follow-up imaging studies or worsening of symptoms felt to be derived from the treated area. Marginal failure denotes a failure within the region of rapid dose fall-off immediately outside the target volume. Causes of marginal failure can be geographical misses due to limitations in the accuracy of treatment delivery and patient setup error or underestimation of the clinical target volume (CTV), either by limitations of imaging or underestimation of the volume at risk. Distant failure is progressive metastatic disease involving other untreated vertebral bodies within the spinal column. For the purpose of this discussion, distant failure may be subclassified as failure at the immediately adjacent levels or at true distant portions of the untreated spine (Table 12.1). The parameters to determine treatment failures are twofold in spine radiosurgery: clinical and radiographic. Because pain is the most common symptom of spine tumors, the serial scoring of pain is a reliable, though subjective, functional end point. It is important to note that involvement of other untreated spinal pathology and nonspine metastatic sites may make pain assessment difficult and obscure the outcome assessment. Another clinical end point is the neurologic examination, especially when there was any neurologic deficit prior to treatment. This end point is an objective measurement of outcome compared with the subjective reporting of pain scores. Follow-up imaging studies (magnetic resonance imaging [MRI], computed tomography [CT], and positron emission tomography [PET]) may provide information on the anatomical extent of tumor control or possible progression. Results of failure after radiosurgery in the initial experience of 61 treated patients with spine metastases at the Henry Ford Hospital (Detroit, Michigan) have been reported.1 Failure of pain control from the symptomatic spine lesion was seen in 6% of the cohort. The results are illustrated in Fig. 12.1. There were two different categories of failure of pain control: in-field persistent pain (lack of pain response) and in-field progressive pain (symptomatic progression). In the category of persistent pain, the pain may persist without improvement, or the pain may be briefly improved but rapidly recurs.
Treatment Failure and Complications
 Patterns of Treatment Failure
Patterns of Treatment Failure
| In-field persistent pain (lack of pain response) |
| In-field progressive pain (symptomatic progression) |
| Radiographic progression within the treatment volume |
| Marginal radiographic progression at the periphery of the target volume |
| Progression at the immediately adjacent spine level |
| Progression at remote spine levels |
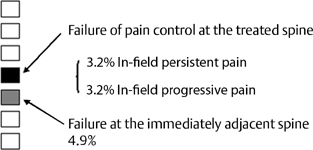
Figure 12.1 Patterns of failure after radiosurgery for solitary spine metastasis.
Although the persistent or progressive pain seems to be due solely to tumor progression at the treated spine, there can be other causes of pain recurrence at the treated spine. An example of such a clinical scenario is presented here. A patient with metastatic non-small cell lung cancer developed left arm radiculopathy and upper extremity weakness with finger grip strength 3/5 of left hand. MRI revealed an enhancing epidural soft tissue mass at C7-T1 with involvement of neural foramen, more on the left side (Fig. 12.2A). The patient was treated with radiosurgery 16 Gy to the epidural lesion and the involved spines. After radiosurgery, muscle strength improved to 4/5 as well as radiculopathy. MRI obtained 6 months after radiosurgery showed a reduction of epidural lesion (Fig. 12.2B). However, 13 months after radiosurgery, the patient started having recurrent and worsening left arm pain. MRI scan showed worsening of the epidural-enhancing lesion extending longitudinally beyond the original target spines (Fig. 12.2C). Subsequently, the patient underwent decompressive surgery. The final pathology showed necrosis without evidence of tumor presence. This suggests that the recurrent pain was due to the tumor necrosis after radiosurgery, rather than tumor progression. Other causes are the compression fracture and spinal instability. A combined modality approach with vertebroplasty or kyphoplasty has also been shown to be effective in the treatment of pain related to compression fractures.2
Another type of pain failure is a progression of pain in the treated spine. This may be due to an inadequate radiosurgery dose or inadequate target definition. Some tumor histology may be more radioresistant, such as renal cell carcinoma and melanoma. A series of 60 cases of renal cell carcinoma spine metastases treated with radiosurgery at the same dose level used in other histologies (mean 20 Gy) demonstrated good initial pain responses in 89% of the patients. But 12% of patients underwent subsequent open surgical intervention for disease progression.3 All failures occurred in patients receiving a lower maximum dose of 17.5 Gy. This rate of failure was not observed in other series of patients with other histologies. Dose escalation and/or the use of radiosensitizing agents may prove of benefit in some tumor histologies.
Failure at the immediately adjacent spine is an anatomical cause of failure after spine radiosurgery. It is important to identify the failure at the immediately adjacent spine because the radiosurgery targets only the involved vertebral segment. An example is illustrated in Fig. 12.3. This patient had a metastatic lung cancer initially involving T5 and this was treated with radiosurgery. The patient developed a T4 metastasis after 6 months, then a T3 metastasis after 8 months. These lesions were individually treated with radiosurgery. The patient had excellent symptomatic relief following each radiosurgery procedure. Note the thickening of the prevertebral fascia and soft tissue mass in the mediastinum extending along the vertebra. The patient had simultaneous tumor progression at the primary site as well as systemic metastasis. One important “limitation” of spine radiosurgey may be that it provides treatment to the targeted spinal level only. This is different from the conventional external beam radiotherapy that includes one or two spine segments both above and below the involved level. Failure rates in the immediately adjacent spine were found to be only 5%.1 This low rate of adjacent-level failure supports the radiosurgery approach.

Figure 12.2 Recurrence of pain due to necrosis of epidural lesion at the treated spine. (A) This patient was treated for a C7-T1 metastatic lung cancer with epidural compression with a dose of 16 Gy. The patient had a arm pain relief and motor improvement. (B) MRI after 6 months showed stable appearance with mild reduction of the epidural lesion. (C) At 13 months after radiosurgery, patient had worsening pain in the arm. MRI showed progression of epidural compression. Decompressive surgery was performed. Pathology revealed necrosis with no evidence of viable tumor.

Figure 12.3 Failure at the immediately adjacent spine. This patient had a metastatic lung cancer initially involving T5 and was treated with radiosurgery. More metastases occurred at T4 after 6 months and at T3 after 8 months. These were treated with radiosurgery each time. Complete pain relief was achieved with each radiosurgery treatment. Note the thickening of the prevertebral fascia and soft tissue mass in the mediastinum extending along the vertebra.
Failures of cases of epidural cord compressions are discussed in detail in Chapter 11, with an emphasis on the relative indications of radiosurgery versus open surgery.
 Neural Complications
Neural Complications
The potential consequence of radiation-induced spinal cord injury can be severe. The classic treatment of acute and chronic radiation effects has been mainly steroid therapy and supportive care for the symptoms. Although surgical resection has been employed for focal brain radionecrosis, it cannot be readily used if a necrotic focus occurs within the spinal cord. The best way to prevent radiation myelopathy is to avoid unnecessary or excessive irradiation to the spinal cord. Therefore, it is crucial to achieve good dose conformality to the tumor volume while minimizing the dose to the spinal cord.
The nature of radiation-induced myelopathy may not be different from that of brain injury following radiosurgery or fractionated radiotherapy. The mechanism of radiation injury of the neural tissue is not well understood. A current understanding of radiation neural damage involves the existing concept of parenchymal cell loss and vascular damage and a more complex dynamic interaction with active participation of various host cells in the local tissue.4–8 The spinal cord may have unique radiobiologic features associated with blood-spinal cord barrier disruption after radiation, in addition to the damage to long neuronal tracts.9 Details of radiobiological consideration of spinal cord damage are described in Chapters 1 and 2. Within the spinal cord, there are several different neural tissues, and these may have varying sensitivities to radiation. It is also believed that the anterior spinal artery has the potential to be injured by high doses of radiation, leading to spinal cord ischemia. Finally, radiation-induced edema within the spinal cord can also cause acute or chronic clinical symptoms.
Neural complications may be divided into three categories based on the time of clinical manifestation after radiosurgery (Table 12.2). Acute complications occur in the first month after radiosurgery and are usually temporary. Subacute complications occur approximately 3 to 6 months after radiosurgery. The transient development of neurologic symptoms is thought to occur secondary to demyelination. Long-term complications occur after 6 months, and the symptoms may be either transient or permanent. The time frame of clinical manifestation of complications may overlap throughout the process. In addition, there are many other tumor and host factors that predispose the patient to the development of neural complications.10,11 Fortunately, the reported incidence of spinal cord complications seems to be very low after radiosurgery for both benign and malignant spine tumors, although long-term follow-up is still lacking.12.16
| Acute |
| Exacerbation of pain |
| Exacerbation of neurologic dysfunction |
| Subacute |