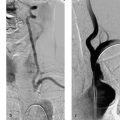
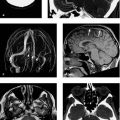
9 Treatment of Acute Cerebral Cerebral venous and sinus thrombosis (CVST) is contributory in 0.5% of all strokes. The incidence is ~4 cases per 1 million population. CVST may occur at any age, but young people and newborns are disproportionately affected. The peak incidence is 30 years of age. Three-fourths of patients are female, due partly to the fact that CVST has a .1:10 000 incidence in the peripartum period (Filippidis et al. 2009). CVST has numerous potential causes. Various prothrombotic states play an essential role. The occlusive process may cause interstitial edema, increased intracranial pressure, or intracerebral hemorrhage as a result of venous congestion, and associated ischemia can lead to intracellular edema and infarction. The clinical presentation may range from an absence of symptoms, headache, nausea, and papilledema to various neurologic deficits, epileptic seizures, and coma. Note Deep cerebral venous thrombosis takes a particularly severe course. The diagnosis of CVST relies on CT and CT angiography (CTA) as well as MRI using various weighting schemes and venographic sequences. When MRI is used, it is important to recognize and distinguish the various signal patterns that are associated with thrombi of different ages, organizing tissue, normal pacchionian granulations, and anatomic variants of the dural venous sinuses. A common feature is that in combination with the new thrombus formation there is some existing dural sinus thrombosis that has progressed to the cerebral veins and therefore become symptomatic. It should also be kept in mind that venous thrombosis may be combined with arteriovenous dural fistula. The gold standards in the treatment of CVST are conservative therapy with intravenous or low-molecular-weight heparin and the symptomatic treatment of increased intracranial pressure and epileptic seizures. Various forms of endovascular recanalization therapy have been developed. While they have been used successfully in small series, a definite benefit from these treatments has not yet been proven, due in part to the potential of fibrinolytic agents to intensify bleeding. Nevertheless, appropriate endovascular therapy may be justified for individual case management, especially if disease progresses with medical therapy, initial symptoms are severe, or the occlusion is located at a threatening site (e.g., deep cerebral venous thrombosis). Finally, a decompressive hemicraniectomy should be considered in patients with marked symptoms of increased intracranial pressure due to edema, infarction, or hemorrhage (Coutinho et al. 2009). Combined decompressive neurosurgery and surgical thrombectomy is also reported. The goal of endovascular therapy is to recanalize the occluded dural sinus or cerebral vein, first to improve tissue perfusion to prevent additional infarction and second to relieve venous congestion, thereby reducing cerebral edema and lowering the risk of intracerebral hemorrhage. Fibrinolytic agents, usually urokinase or rtPA, can be administered by the systemic, local transarterial, or local venous route, the latter ranging from a brief injection to a protracted infusion. Fibrinolytic therapy may be supplemented or replaced by mechanical techniques to dilate the thrombus with a stent or balloon or remove the thrombus using an aspiration or retriever system. Although systemic fibrinolytic therapy may now be considered obsolete, local intravenous thrombolysis has been performed in the dural sinuses and cerebral veins since 1988. Urokinase is infused for 15 min at a rate of 40 000–750 000 units/h for up to 10 days (or a total rtPA dose of 8–70 mg) by percutaneous venous access or, less commonly, through a burr-hole craniectomy. Case series consisting of one to no more than 20 patients have been reported. Most reports document significant clinical improvement with recanalization rates up to 100%, although deterioration or death from intracranial hemorrhage has occurred in 0–40% of cases (Rahman et al. 2009). The necessary duration of the thrombolytic infusion probably depends on thrombus age, noting that fresh and old thrombi are frequently combined and may even coexist with arteriovenous dural fistulae in older patients. Infusion duration also depends on the extent of the thrombosis and the thrombus mass. Concomitant heparinization is definitely advised during a continuous, prolonged infusion due to the presence of the indwelling catheter. Otherwise, many groups have discontinued heparinization during thrombolysis. Caution Although some groups favor access through the internal jugular vein, transfemoral access appears to be safer. With cervical access, there is a possibility that drainage of the fibrinolytic agent may promote bleeding at the puncture site.
Venous Occlusions
Epidemiology
Etiology, Pathogenesis, and Symptoms
Imaging Studies
Treatment
Endovascular Procedures
Pharmacologic Thrombectomy AngioJet
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree