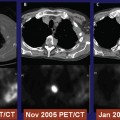
11 Spinal cord compression from the epidural spread of cancer is both common and debilitating. Up to 2.5% of all cancer patients have at least one admission to the hospital for epidural cord compression. At presentation, 90% have either local or radicular pain, sensory changes, or bowel and bladder incontinence, and up to 50% may have lost the ability to ambulate. As a result of complications due to decreased mobility, these patients frequently develop infection and deep vein thrombosis (DVT), complications associated with decreased life expectancy. Their medical condition and pain are difficult to manage and present a great challenge to families and society as a whole. Before radiation therapy was contemplated as a treatment modality for the management of metastatic epidural disease, surgical decompression was the primary option. Until recently, little consideration was given to the anatomical characteristics of the lesion causing the spinal cord compression, and the primary surgical approach consisted of posterior decompressive laminectomy. However, given that most epidural disease is located anterior to the spinal cord, strategies approaching from posterior to the spinal cord frequently resulted in insufficient tumor removal and spinal instability. Surgical outcomes based on posterior strategies were thus less likely to lead to neurologic improvement. After the establishment of radiation therapy as an effective treatment for epidural metastatic disease, laminectomy fell out of favor as subsequent clinical investigations failed to demonstrate a benefit for surgery as compared with radiation therapy alone. External beam radiotherapy has been reported to improve ambulatory function in about 30 to 40% of patients with epidural spinal cord compression.1,2 Unfortunately, neither posterior surgical decompression (i.e., laminectomy) nor radiation therapy represents a truly satisfactory method for treating malignant epidural spinal cord compression. Recently, advances in surgical technique for decompression and stabilization have led to more frequent use of anterior surgical approaches tailored to the anatomical characteristics of the lesion compressing the spinal cord. Although these contemporary surgical strategies have led to apparently superior clinical outcomes, presumably due to more thorough tumor removal, spinal cord decompression, and spinal stabilization, it remains unclear whether these more extensive surgical interventions will prove to be more effective than radiation alone. Patchell et al performed a randomized trial comparing the use radiation therapy alone with the use of up-to-date surgical strategies in combination with radiation therapy.3 Patients who received surgery and radiation retained the ability to ambulate longer than those treated with radiation alone. Patients in the surgical cohort also survived longer and had less pain. It was concluded that metastatic epidural lesions were best treated by the combination of surgery, anatomically tailored to tumor location, followed by external beam radiation therapy. Presumably, the improved clinical and survival outcomes were partly influenced by the fact that greater numbers of patients were ambulatory, which, in turn, led to a decreased incidence of DVT and infection, both of which strongly influence morbidity. Given these encouraging results, one must remain aware of the general infirmity of these patients and realize that operative morbidity can be significant, even though the rate of complications in the patients in the surgical cohort of this investigation was not higher than that noted for patients in the radiation therapy alone cohort. More recently, stereotactically delivered radiation has served as an effective alternative to surgery for many lesions located in the brain and, based in part on improvements in the technology of image guidance, has been applied for the management of lesions in and around the spine and spinal cord.4–14 Given its focused nature, radiosurgery can treat a tumor with high doses of conformal radiation while exposing the surrounding spinal cord to relatively low doses. Radiosurgery currently stands as a treatment alternative to surgery and conventional radiation therapy and may well prove to be superior to conventional radiotherapy for neoplasms in and around the spine and spinal cord. As it becomes more apparent that radiosurgery can serve effectively in the management of certain neoplastic lesions, the question remains whether radiosurgery can be considered an alternative to surgery for tumors located within the spinal canal and, in certain instances, tumors directly compressing the spinal cord. Currently, there is little literature that specifically addresses the role of radiosurgery in the management of neoplastic spinal canal compromise and spinal cord compression, although a considerable body of evidence supports the use of radiosurgery for spinal tumors and other spinal conditions.15 At the Henry Ford Hospital (Detroit, Michigan), we have been conducting a phase II clinical trial addressing the use of radiosurgery in the management of spinal epidural disease and epidural spinal cord compression. Since December 2005, 75 patients with neoplastic disease within the spinal canal have been enrolled. Of these, clinical and radiographic follow-up was available for 42 lesions in 38 patients; these patients comprise the study group for this investigation. All patients were treated with single-fraction spine radiosurgery according to previously detailed protocols used at the Henry Ford Hospital and described elsewhere.12–14,16 The frameless image-guided Novalis system from Brain-Lab AG (Feldkirchen, Germany) and the dosimetric characteristics have been reported.17,18 Patient positioning was achieved using the BodyFix system (Medical Intelligence Medizintechnik GmbH, Schwabmünchen, Germany) with vacuum bags or other positioning devices, as needed. Infrared reflective markers were placed on the skin. Computed tomographic (CT) simulation was performed with intravenous contrast in 2 to 3 mm slices without spacing. Using the dedicated planning system with the BrainScan planning computer (BrainLab), image fusion was routinely achieved with simulation CT and T1-weighted gadolinium contrast and T2-weighted magnetic resonance (MR) images. The radiosurgery target volume and spinal cord were delineated. Radiosurgical treatment generally consisted of multiple (usually 7–9 beams) intensity-modulated radiation beams to minimize the dose to the critical organs, and image-guided repositioning was achieved using infrared marker and image fusion of internal bony structures (i.e., vertebral bony anatomy). Prior to radiation delivery, orthogonal portal films were obtained for final verification of the isocenter. The guidance process that brings the treatment isocenter into alignment with the preplanned isocenter uses six degrees of freedom, with rotations along three axes also considered. Because a target positioning process based solely on infrared skin fiducials is incapable of providing the high precision localization required for treating spinal lesions, the final adjustments (i.e., bringing the target isocenter to the preplanned treatment isocenter) are accomplished with an automated patient-positioning device, which represents co-ordination between the ExacTrac and Novalis Body systems (both BrainLab). The details of these systems are described in other chapters. All patients received single-dose radiosurgery to the involved spine only, and the target volume included the involved vertebral body and pedicles. When paraspinal or epidural soft tissue tumor was present, the involved spine and the gross tumor were both included in the target volume. The spinal cord at-risk volume was consistently defined as the volume extending from 6 mm above to 6 mm below the radiosurgery target. The target tumor and the spinal cord were delineated by fusing data from contrast-enhanced simulation CT images, T1-weighted images (with and without gadolinium contrast), and T2-weighted MR images. The radiation dose was consistently prescribed to the 90% isodose line, which encompassed the periphery of the target. Although radiosurgery doses were selected as part of a dose-escalation paradigm, the primary criteria determining dose selection were the spinal cord dose and the tumor volume coverage constraints. When the spinal cord dose constraint (< 10 Gy to < 10% of the spinal cord volume) was not met, the overall dose prescription had to be reduced. The median radiosurgery dose was 16 Gy, and the median target volume was 66.75 cc. All patients had clinical follow-up from 2 to 30 months (mean 9.2 months, median 8.0 months) and pre- and post-treatment radiographic follow-up (mean 8.46 months, median 8.10 months). The pretreatment grading system was based on a combination of radiographic and neurologic data (Fig. 11.1): Grade 0 No visible tumor within the spinal canal Grade I Tumor identified within the spinal canal but not involving the dura; normal neurologic examination Grade II Tumor involving/distorting the dura without spinal cord involvement; normal neurologic examination Grade III Tumor compressing/distorting the spinal cord; normal neurologic examination Grade IV Tumor compressing the spinal cord; abnormal neurologic examination Tumor was noted within the spinal canal in all cases.
Treatment of Spinal Canal Compromise
 Radiosurgery Procedure
Radiosurgery Procedure
Definition of Tumor Volume and Spinal Cord
Grading of Canal Compromise and Outcome of Radiosurgery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree