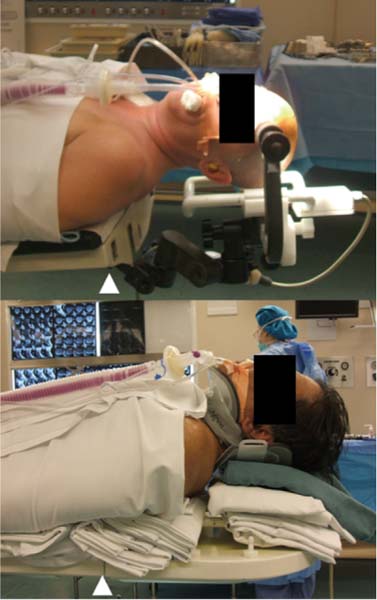
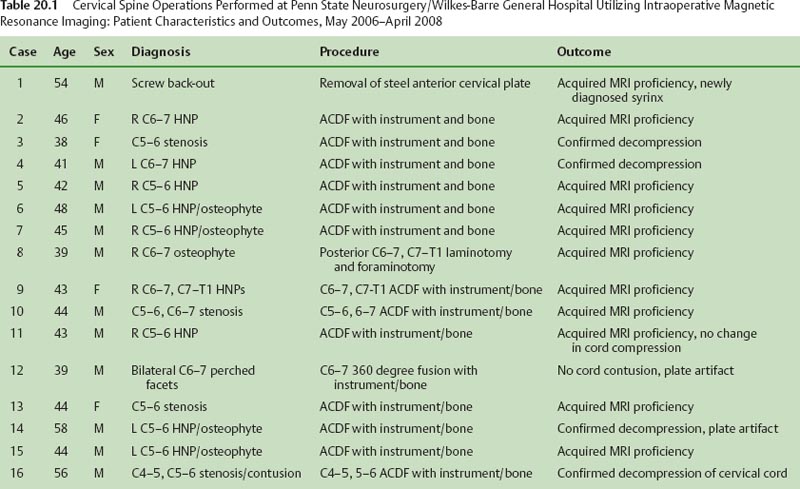
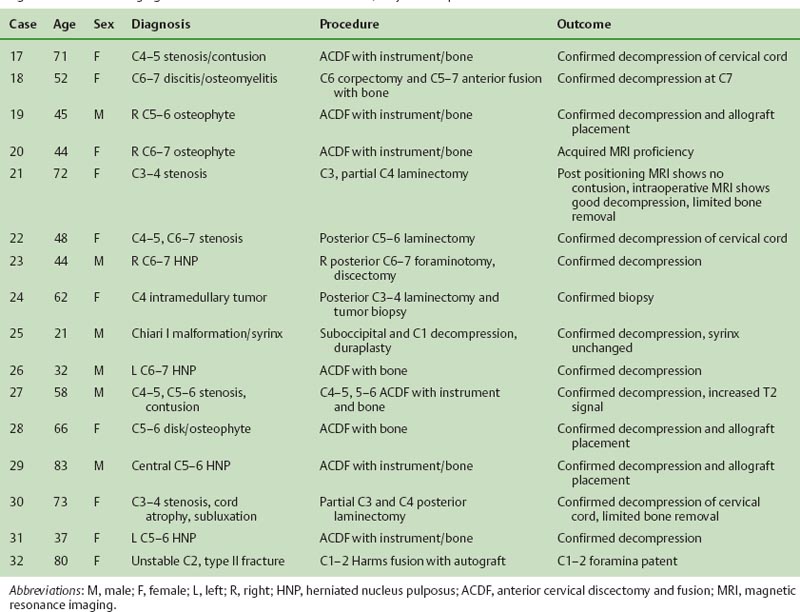
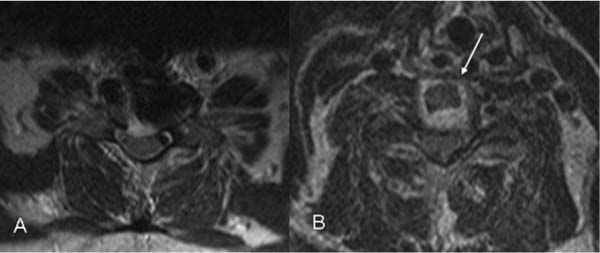
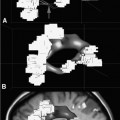
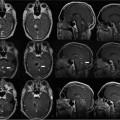
20 The growth of intraoperative magnetic resonance imaging (iMRI) technology has led to significant advances in the field of cranial neurosurgery. MRI’s ability to visualize the surgical field in multiple planes and to combine physiologic data with near-real-time imaging has begun to change the way tumors are being resected.1–4 In contrast, there are currently no iMRI systems that are in common use for the adult spine. There are also fewer published reports describing spinal applications for iMRIs. Part of the reason may be that, unlike cranial operations, spinal surgery does not easily fit inside a magnet. Another reason could be due to MRI’s superior ability to visualize intracranial lesions and this has naturally led to a greater focus on these surgeries. Regardless of the reason, iMRI could potentially have more usefulness for diseases of the spine than the brain. If cranial neoplasms have traditionally been the most common indication for intraoperative imaging, neoplasms of the spinal cord and vertebral column are far more prevalent when metastatic disease is included.5,6 Degenerative diseases causing spinal cord or nerve root compression are even more common and account for a greater proportion of operations than cranial or spinal neoplasms in most general neurosurgery practices. Finally, spine surgery already incorporates intraoperative imaging. This is most commonly seen in spinal stabilization procedures to check for correct positioning of implants. The added ability to intraoperatively assess the spinal cord during such procedures or to confirm the radiologic success of a decompression would be an easily recognizable advantage of MRI. If the recent history of cranial surgery is a guide, iMRI for spine surgery will likely grow with technological advances. The direction of this growth will depend on which systems are adopted by the surgical community. Therefore, as this field is in its infancy, understanding the history and current state of the art can lead to a better understanding of where spinal intraoperative imaging will be in the future. MRI is the most recent imaging technology being adapted to the neurosurgical operating room (OR). The use of portable ultrasound for localizing intracranial tumors has a long history.7 Intraoperative angiograms using portable fluoroscopy have already become standard additions to the neurosurgical armamentarium for clipping aneurysms.8 Ultrasound is also being studied to assist spinal surgery.9,10 The successful introduction of any imaging technology into the OR is subject to numerous factors. The above examples suggest that portability and convenience are key components. Although a discussion of MRI technology is beyond the scope of this chapter, it is relatively apparent that traditional MR diagnostic systems are neither portable nor easy to use in an OR. The first systems developed in the late 1990s required modifications to the OR to accommodate intraoperative imaging.11,12 Regardless, the initial experience of spinal surgeries using MRI were performed on these systems. In 1999, Verheyden et al described 16 thoracic and lumbar surgeries utilizing instrumentation that were performed within a GE Signa SP (General Electric Medical Systems, Waukesha, WI) double-donut MRI scanner.13 Woodard et al in 2001, used a similar system to perform iMRI during nine cervical and three lumbar operations.14 Hall et al, in a review of high-field iMRI procedures at the University of Minnesota in 2000, included one lumbar operation, three thoracic operations, and one sacral operation using a Philips Gyroscan (Philips Healthcare, Andover, MA).15 Each of these studies demonstrated the safety and feasibility of iMRI for spinal surgery in a magnetic environment. Otherwise, the number of cases performed was generally small and a search of the literature showed no other published reports for spine surgery in any of the major journals. The absence of additional observations appears to parallel the lack of acceptance that these systems received outside their respective centers. More recently, several newer systems developed for neurosurgical applications, such as PoleStar (Medtronic Navigation, Inc., Louisville, CO),16 Brainsuite (Laboratory of Neuro Imaging, UCLA),17 and IMRIS (IMRIS, Winnipeg, Manitoba, Canada),18 have adopted the strategy of having lower impact on the surgical environment. None of these newer systems, however, are designed to intraoperatively image the adult spine. These developments and the paucity of recent studies utilizing MRI for spinal surgery indicate that technologic advances have not yet been applied to this field. One way to illustrate what the future may hold is to review the experience using iMRI on a personal, unpublished series of recent cervical spine operations performed at Wilkes-Barre General Hospital in Pennsylvania. The IMRIS at Wilkes-Barre General Hospital was one of the first systems installed in the United States that utilized a large-bore, high-field magnet mounted on rails (Fig. 20.1). It allowed general neurosurgical procedures to be performed in a suite where the magnet was brought in as surgical circumstances warranted. This site had the additional advantage of being associated with a general neurosurgery practice. There was therefore an ample population of spinal surgeries which could be exposed to this technology. During the early utilization of the system, it became apparent that a standard craniotomy position allowed the IMRIS to visualize the superior cervical spine. This property had been described before. Kaibara et al in 2001, reported on three transoral resections for odontoid pathology that used intraoperative imaging.19 This demonstrated that a mobile magnet could image the cervicomedullary junction during surgery and that the information could alter surgical planning. At Wilkes-Barre, it was noticed that positioning the patient 10 to 20 cm superior on the OR table allowed imaging of the entire cervical spine (Fig. 20.2). Given the relative ease of visualizing the cervical spine, a decision was made to use IMRIS in these operations. Clinical usefulness, however, was not the initial goal at Wilkes-Barre. Cervical surgeries were performed frequently enough that they could be used to make OR personnel proficient with MRI protocols. Otherwise, the preparation and imaging were similar to cranial operations and these were the surgeries that were expected to benefit from intraoperative imaging. As experience developed, these initial procedures revealed several distinct drawbacks that demonstrated how much more difficult cervical spine surgeries were when using iMRI. Fig. 20.1 The IMRIS (IMRIS, Winnipeg, Manitoba, Canada) suite at Wilkes-Barre General Hospital with Siemens Open Bore Espree 1.5 tesla magnetic resonance imaging (MRI) scanner positioned at the head of operating room table. Head holder is attached to the table with paired two channel coils in place. Fig. 20.2 Comparison of standard supine craniotomy position in pins (top) to supine anterior cervical diskectomy position on bolsters (bottom). In cervical diskectomy position, head is ~15 cm. superior. White arrow indicates table break. Imaging the cervical spine in IMRIS requires positioning paired coils around the patient’s neck. These are the same coils used for cranial MRIs. These rigid coils were designed to lie in close proximity to the patient’s head. They are configured as paired half cylinders positioned superior and inferior to the surgical site. Positioning these coils to fit under the patient’s neck would sometimes cause them to protrude into the base of the cervical spine. This happened most frequently in obese or broad-shouldered individuals and extra care was taken to pad these patients. In extreme cases, it was found that if the inferior paired coil could not fit, the other coil could be placed on top of the surgical site. The images obtained were usually adequate enough to visualize the cervical spine. Although these steps prolonged the preparation time for the surgery, they did not affect the operation. What had the greatest impact on the operation were those systems that were in physical contact with the patient. Physiologic monitoring became limited. Because of inherent constraints to electrocardiogram (EKG) monitoring during MR imaging, cardiac electrodes could not be dispersed in the standard montage. Axis deviation and changes in signal polarity could not be reliably measured. In addition, the copper wires and stainless steel needles for electrophysiologic monitoring can have potentially deleterious effects in a high-field magnet. Prior to imaging, all of these wires are removed. Therefore, no further monitoring can be performed after the first intra-operative image. Finally, the wrapping and padding of the patient restricts access to the prominence of the iliac crest. This severely limits how easily autologous bone graft can be harvested. In some cases cutting through the drapes can alleviate this, but it was occasionally difficult to obtain a sufficient amount of autologous bone graft. Except for these preparations, the actual surgical procedure could be performed in a routine manner. Between May 2006 and April 2008, 32 cervical surgeries were performed. Case characteristics are summarized in Table 20.1. In every case, a standard approach using normal instrument trays was performed. Surgical time was prolonged due to the MR imaging. In general, it would take at least 15 to 20 minutes to prepare the surgical field to bring in the magnet, another 20 minutes to acquire the images, and a final 15 to 20 minutes to resume the surgery. Interrupting this surgery was analogous to performing an intraoperative angiogram during aneurysm clipping. Reviewing the 32 operations, there were no adverse effects from positioning, anesthesia, or MR imaging. There were also no complications from the prolonged preparation or surgical times. Isolated problems arose when imaging quality was poor. These occurred early in the program and were mostly attributed to radiofrequency interference from sources inside the OR. Several observations were made during these surgeries that underscored the advantage of intraoperative imaging. The majority of intraoperative imaging for cervical spine surgery was for anterior cervical discectomies with fusion. Seventeen single-level and four two-level discectomies were performed for degenerative spine disease. Most of the procedures performed in the first year were used for training purposes. Patients would be prepared for a magnet case, the surgical procedure was performed including instrumenting with an anterior plate, and then the MRI was obtained prior to removing the surgical drapes and transferring the patient. These images were therefore not clinically different than obtaining an outpatient MRI following surgery. As proficiency improved, however, review of the images showed subjectively better detail than standard outpatient studies. It was unclear whether this was due to the proximity of the coil to the neck or the absence of movement with the patient under anesthesia. Metal artifact from the anterior plate and screws obscured some detail but overall, the initial cases proved the feasibility of intraoperative imaging for anterior cervical discectomies. More importantly, the information from the intraoperative images became useful for the cervical surgeries themselves. It provided immediate feedback that the herniated disk was removed or that the stenosis was relieved. This gave a subjective sense of certainty that the goal of surgery had been accomplished. It is analogous to the objective confirmation that occurs after obtaining a plain x-ray to check the position of an anterior cervical plate.
Treatment of Spinal Disorders
History
Penn State/Wilkes-Barre Experience
Anterior Cervical Discectomies
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree