5 Tumors and Tumor-Like Lesions
Definition
Primary bone tumors and tumor-like lesions comprise malignant and benign space-occupying lesions. They are relatively rare in the shoulder region. According to Barlow and co-workers, only 5% of all primary bone tumors are in the proximal humerus, scapula, and acromial end of the clavicle. Certain lesions, however, have a predilection for the shoulder. For instance, 51% of juvenile bone cysts occur in the shoulder region.
Clinical Findings
 Pain
Pain
 Swelling
Swelling
 Pathological fractures
Pathological fractures
Diagnostic Evaluation
General remarks
The age of the patient and location of the tumor are of utmost importance in diagnosing bone tumors:
 Young patients up to age 30 years generally harbor benign or malignant primary bone tumors, while patients over age 50 years predominantly have secondary malignant bone tumors (metastases)
Young patients up to age 30 years generally harbor benign or malignant primary bone tumors, while patients over age 50 years predominantly have secondary malignant bone tumors (metastases)
 Typical bone tumors of older patients include plasmocytoma, chondrosarcoma, malignant fibrous histiocytoma, and lymphoma
Typical bone tumors of older patients include plasmocytoma, chondrosarcoma, malignant fibrous histiocytoma, and lymphoma
Most tumors are located in the metaphyses, with the following exceptions:
 Giant cell tumor, chondroblastoma, and clear cell chondrosarcoma are characteristically located in the epiphyses
Giant cell tumor, chondroblastoma, and clear cell chondrosarcoma are characteristically located in the epiphyses
 Ewing sarcoma is characteristically located in the diaphyses
Ewing sarcoma is characteristically located in the diaphyses
 Juvenile bone cysts generally arise in the metaphyses and can grow into the diaphyses
Juvenile bone cysts generally arise in the metaphyses and can grow into the diaphyses

Indications
 Most important modality for diagnostic classification of bone tumors
Most important modality for diagnostic classification of bone tumors
Recommended views
 Standard projections in two views
Standard projections in two views
 Special projections depending on the location of the tumor
Special projections depending on the location of the tumor
Findings
 Smoothly or indistinctly outlined osteolysis
Smoothly or indistinctly outlined osteolysis
 Osteoblastic changes
Osteoblastic changes
 Cortical destruction
Cortical destruction
 Matrix calcifications or ossifications
Matrix calcifications or ossifications
 Periosteal changes
Periosteal changes

Indications
 Plays no significant role in tumors
Plays no significant role in tumors
 Possibly for evaluation of soft-tissue component or joint effusion
Possibly for evaluation of soft-tissue component or joint effusion

Indications
 Evaluation of the outline of a lesion
Evaluation of the outline of a lesion
 Cortical destruction (differentiating an enchondroma and low-grade chondrosarcoma)
Cortical destruction (differentiating an enchondroma and low-grade chondrosarcoma)
 Better evaluation of matrix changes
Better evaluation of matrix changes
 Assessment of mechanical stability
Assessment of mechanical stability
Recommended protocol (See p. 16, Standard Parameters)
 Standard computed tomography (CT) or spiral CT:
Standard computed tomography (CT) or spiral CT:
– Section thickness: 2–5 mm
– Table feed: 2–5 mm/rotation
– Increment: 1–3 mm
Findings
 Smoothly or indistinctly outlined osteolysis
Smoothly or indistinctly outlined osteolysis
 Osteoblastic changes
Osteoblastic changes
 Cortical destruction
Cortical destruction
 Matrix calcifications or ossifications (more discernible and better evaluated than with conventional radiographic views)
Matrix calcifications or ossifications (more discernible and better evaluated than with conventional radiographic views)
 Periosteal changes
Periosteal changes

Indications
 Main indication is preoperative staging to evaluate articular invasion and neurovascular infiltration
Main indication is preoperative staging to evaluate articular invasion and neurovascular infiltration
 Monitoring of malignant tumors undergoing chemotherapy
Monitoring of malignant tumors undergoing chemotherapy
 Limited role in establishing the diagnosis
Limited role in establishing the diagnosis
 For the diagnostic evaluation of cystic lesions: Detection of blood products, for example, in aneurysmal bone cyst and pigmented villonodular synovitis (PVNS)
For the diagnostic evaluation of cystic lesions: Detection of blood products, for example, in aneurysmal bone cyst and pigmented villonodular synovitis (PVNS)
Recommended sequences
 T1-weighted spin-echo (SE) sequence (long axis)
T1-weighted spin-echo (SE) sequence (long axis)
 T1-weighted SE sequence (long axis) with contrast enhancement
T1-weighted SE sequence (long axis) with contrast enhancement
 T2-weighted turbo spin-echo (TSE) sequence (short axis)
T2-weighted turbo spin-echo (TSE) sequence (short axis)
 Fat-saturated T1-weighted SE sequence (short axis) with contrast enhancement
Fat-saturated T1-weighted SE sequence (short axis) with contrast enhancement
 Short time inversion recovery (STIR) sequence (long axis)
Short time inversion recovery (STIR) sequence (long axis)
 T1-weighted SE or STIR sequence of the entire humerus with adjacent joints in malignant tumors to exclude skip lesions
T1-weighted SE or STIR sequence of the entire humerus with adjacent joints in malignant tumors to exclude skip lesions
Findings
 T1-weighted SE sequence:
T1-weighted SE sequence:
– Hypointense visualization of the tumor
– Cortical destruction
– Hypointense soft-tissue component
 T2-weighted SE sequence:
T2-weighted SE sequence:
– Hyperintense visualization of the tumor, possibly also hypointense depending on the extent of the sclerosis
– Hyperintense visualization of the bone marrow and the soft-tissue component
– Hypointense visualization of blood products (hemosiderin), as found in PVNS
 T1-weighted SE sequence with contrast enhancement:
T1-weighted SE sequence with contrast enhancement:
– Enhancement of solid tumors and cyst membranes
– Enhancement of the extraosseous soft-tissue component
– Enhancement of the bone-marrow edema
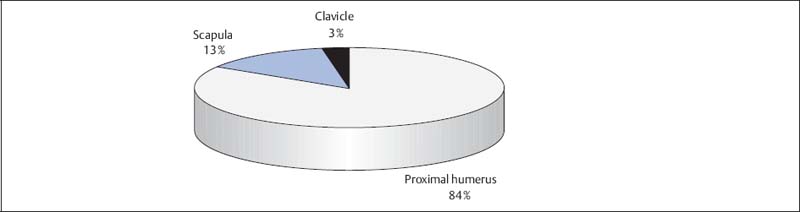
Fig. 5.1  Tumor location in the shoulder (n = 711)
Tumor location in the shoulder (n = 711)
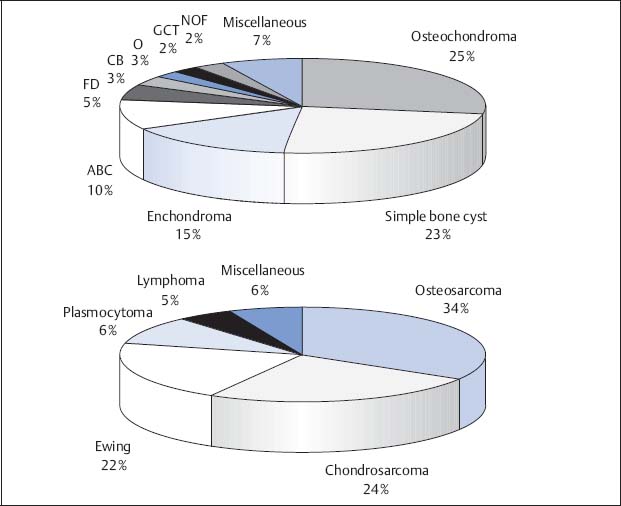
Fig. 5.2 a, b  Benign and malignant bone tumors of the shoulder
Benign and malignant bone tumors of the shoulder
a Benign bone tumors (n = 494)
b Malignant bone tumors (n = 217)
ABC | Aneurysmal bone cyst |
CB | Chondroblastoma |
FD | Fibrous dysplasia |
NOF | Nonossifying fibroma |
O | Osteoid osteoma |
GCT | Giant cell tumor |
Location and Distribution of Primary Bone Tumors and Tumor-like Lesions
From 1974 to 1998, the Tumor Registry of the University of Munster, Germany, recorded and analyzed 711 tumors:
 Of these tumors, 602 were located in the humerus, 90 in the scapula, and 19 in the clavicle (Fig. 5.1). This distribution correlates well with the results of the review conducted by Barlow and co-workers, who found 75% of the tumors in the proximal humerus, 20% in the scapula, and 5% in the clavicle.
Of these tumors, 602 were located in the humerus, 90 in the scapula, and 19 in the clavicle (Fig. 5.1). This distribution correlates well with the results of the review conducted by Barlow and co-workers, who found 75% of the tumors in the proximal humerus, 20% in the scapula, and 5% in the clavicle.
 The average patient age at the time of diagnosis was 31.5 years.
The average patient age at the time of diagnosis was 31.5 years.
 69% of the recorded lesions were benign compared to 50% benign lesions found in the review conducted by Barlow and co-workers:
69% of the recorded lesions were benign compared to 50% benign lesions found in the review conducted by Barlow and co-workers:
– The benign tumors included 143 osteochondromas, 115 juvenile bone cysts, 75 enchondromas, and 50 aneurysmatic bone cysts
– The remaining benign tumors included 25 fibrous dysplasias, 15 chondroblastomas, 13 osteoid osteomas, 12 giant cell tumors, and 11 nonossifying fibromas (NOF, Fig. 5.2 a)
 Malignant tumors are less frequent:
Malignant tumors are less frequent:
– The malignant tumors included 72 osteosarcomas, 52 chondrosarcomas, and 46 Ewing sarcomas (Fig. 5.2 b). Primary lymphomas of the bone were found in 10 cases
– Focal plasmocytomas with primary manifestation in the shoulder were found in 20 cases
– The tumor can be judged to be probably benign or probably malignant by its outline on the conventional radiograph (Figs. 5.3, 5.4)
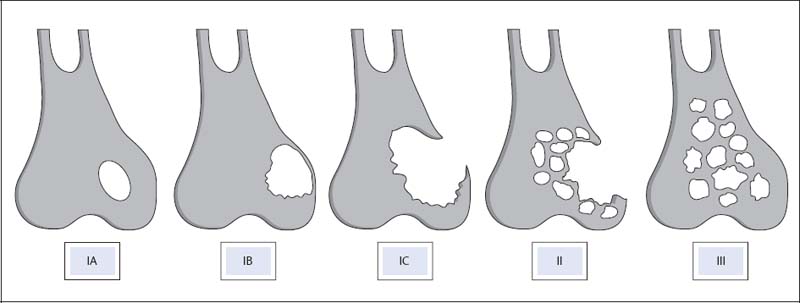
Fig. 5.3  Lodwick’s classification for estimating growth rates of focal bone lesions
Lodwick’s classification for estimating growth rates of focal bone lesions
IA lesions are sharply defined osteolytic lesions located within the bone. IB lesions are sharply defined osteolytic lesions with cortical expansion and thinning. IC lesions show cortical destruction in the presence of a relatively smooth edge. Grade II lesions have a poorly defined outline and show cortical destruction. Grade III lesions are permeative, motheaten-like, aggressive lesions. The IA and IB lesions correspond to a pattern of slow growth rate (e.g., juvenile bone cyst) and the II and III lesions to a pattern of high growth rate (e.g., osteosarcoma). The IC lesions can have a slow or high growth rate, with the giant cell tumor a typical example.

Fig. 5.4 a, b  Lodwick IB and II lesions
Lodwick IB and II lesions
a Sharply defined Lodwick IB lesion, histologically corresponding to a juvenile bone cyst.
b Poorly defined Lodwick II lesion, histologically corresponding to metastatic bone lesion (from a renal cell carcinoma).
Benign Bone Tumors
Osteochondroma
Goals of Imaging
 Visualization of the osteolytic or osteoblastic lesion (with conventional radiography or computed tomography [CT])
Visualization of the osteolytic or osteoblastic lesion (with conventional radiography or computed tomography [CT])
 Detection of matrix changes (with conventional radiography or Visualization of periosteal reaction (with conventional radiography or CT)
Detection of matrix changes (with conventional radiography or Visualization of periosteal reaction (with conventional radiography or CT)
 Detection of cortical destruction (with conventional radiography or CT)
Detection of cortical destruction (with conventional radiography or CT)
 Relationship of the tumor to the joint (with magnetic resonance imaging [MRI])
Relationship of the tumor to the joint (with magnetic resonance imaging [MRI])
 Relationship of the tumor to vessels and nerves (with MRI)
Relationship of the tumor to vessels and nerves (with MRI)
Therapeutic Principles of the Osteochondroma
 Resection if symptomatic or causing complications, for example, damage to vessels or nerves, fractures, bursitis
Resection if symptomatic or causing complications, for example, damage to vessels or nerves, fractures, bursitis
 Resection also when the tumor is growing and if desired by patient, prophylactically or if located close to the axial skeleton
Resection also when the tumor is growing and if desired by patient, prophylactically or if located close to the axial skeleton
 Resection along the margin, usually including the base
Resection along the margin, usually including the base
 Recurrences originate in the region of the cartilaginous component and generally occur only in children, thus surgical intervention preferably after puberty
Recurrences originate in the region of the cartilaginous component and generally occur only in children, thus surgical intervention preferably after puberty
Definition
 Most common benign bone lesion
Most common benign bone lesion
 Cartilage-forming tumor
Cartilage-forming tumor
 Osseous projection with cartilage cap
Osseous projection with cartilage cap
 Located in the shoulder in 22 % of cases
Located in the shoulder in 22 % of cases
 In the presented patient material, of 143 osteochondromas, seven were located in the clavicle, 39 in the scapula, and 97 in the humerus
In the presented patient material, of 143 osteochondromas, seven were located in the clavicle, 39 in the scapula, and 97 in the humerus
 Average age of patients: 19.3 ± 14.9 years
Average age of patients: 19.3 ± 14.9 years
Pathology
 Osteochondromas can be broad-based (Fig. 5.5) or on a stalk (Fig. 5.6)
Osteochondromas can be broad-based (Fig. 5.5) or on a stalk (Fig. 5.6)
 While malignant transformation is rare for osteochondromas on a stalk, it is more frequent in sessile osteochondromas
While malignant transformation is rare for osteochondromas on a stalk, it is more frequent in sessile osteochondromas
 Histologically, osteochondromas show a cartilaginous cap and an osseous component that connects with the underlying bone
Histologically, osteochondromas show a cartilaginous cap and an osseous component that connects with the underlying bone
 The osseous component is histologically identical to the structure of healthy bone
The osseous component is histologically identical to the structure of healthy bone
 The thickness of the cap is an indication for a possible malignant transformation: a width exceeding 2–3 cm is suspicious for malignant transformation (frequent in the shoulder)
The thickness of the cap is an indication for a possible malignant transformation: a width exceeding 2–3 cm is suspicious for malignant transformation (frequent in the shoulder)
 Furthermore, irregular calcifications away from the base of the lesion are suspicious for malignant degeneration
Furthermore, irregular calcifications away from the base of the lesion are suspicious for malignant degeneration
Clinical Findings
 Usually asymptomatic
Usually asymptomatic
 Rarely, symptomatic due to pressure on muscle, bone, nerves, or vessels
Rarely, symptomatic due to pressure on muscle, bone, nerves, or vessels
 Rarely, inflammatory changes in an exostotic bursa (bursitis) overlying the cartilage cap
Rarely, inflammatory changes in an exostotic bursa (bursitis) overlying the cartilage cap
Diagnostic Evaluation

Findings
 Typical picture of broad-based or stalked exostosis
Typical picture of broad-based or stalked exostosis
 Occasional calcifications in the cartilage cap
Occasional calcifications in the cartilage cap
 Adjacent bone can be deformed or show growth disturbance
Adjacent bone can be deformed or show growth disturbance
 In general, no further imaging necessary to establish the diagnosis
In general, no further imaging necessary to establish the diagnosis

Indications
 Method of choice to determine the width of the cartilaginous cap if malignant transformation is suspected
Method of choice to determine the width of the cartilaginous cap if malignant transformation is suspected

Fig. 5.5  Osteochondroma of the humerus
Osteochondroma of the humerus
Sessile osteochondroma of the proximal humerus in an 11-year-old boy.

Fig. 5.6  Osteochondroma of the scapula
Osteochondroma of the scapula
Tangential view of the scapula with stalked osteochondroma of the scapula in an 18-year-old male patient.
Juvenile Unicameral Bone Cyst
Definition
 Simple juvenile unicameral bone cysts are relatively common, typically located in the region of the shoulder (51%)
Simple juvenile unicameral bone cysts are relatively common, typically located in the region of the shoulder (51%)
 The preferred site is the proximal metadiaphyseal region of humerus, with rare extension of the cyst into the epiphysis
The preferred site is the proximal metadiaphyseal region of humerus, with rare extension of the cyst into the epiphysis
 In the presented patient material, all 115 unicameral bone cysts were in the humerus, with no lesions found in the scapula or clavicle
In the presented patient material, all 115 unicameral bone cysts were in the humerus, with no lesions found in the scapula or clavicle
 Average age of patients: 13.8 ± 9.7 years
Average age of patients: 13.8 ± 9.7 years
Pathology
 Smoothly marginated cyst formation
Smoothly marginated cyst formation
 The lining membrane consists of a few cells and can measure up to 1 cm (Fig. 5.7 a)
The lining membrane consists of a few cells and can measure up to 1 cm (Fig. 5.7 a)
 Surgical curettage essentially produces no solid tissue
Surgical curettage essentially produces no solid tissue
 The cyst fluid has an elevated concentration of alkaline phosphatase
The cyst fluid has an elevated concentration of alkaline phosphatase
Clinical Findings
 Pathological fractures are frequent and are the first symptom in 70% of cases of this nonneoplastic condition (Fig. 5.7 b)
Pathological fractures are frequent and are the first symptom in 70% of cases of this nonneoplastic condition (Fig. 5.7 b)
 Not infrequently, pain, swelling, and restricted mobility of the shoulder joint Diagnostic Evaluation
Not infrequently, pain, swelling, and restricted mobility of the shoulder joint Diagnostic Evaluation
Diagnostic Evalution

Findings
 Located centrally in the bone
Located centrally in the bone
 Not infrequently, intersecting lines traversing the cyst
Not infrequently, intersecting lines traversing the cyst
 Marginal sclerosis (Fig. 5.7 b)
Marginal sclerosis (Fig. 5.7 b)
 Generally causing only a moderate expansion of the bone
Generally causing only a moderate expansion of the bone
 Periosteal reaction only after fracture
Periosteal reaction only after fracture
 In 20%, a fallen cortical fragment (“fallen leaf sign”) indicative of a fracture
In 20%, a fallen cortical fragment (“fallen leaf sign”) indicative of a fracture
 Radiographic finding usually so unequivocal that additional imaging studies are not necessary
Radiographic finding usually so unequivocal that additional imaging studies are not necessary

Indications
 If inconclusive due to superimposition or atypical presentation
If inconclusive due to superimposition or atypical presentation

Indications
 Reserved for unclear cases
Reserved for unclear cases
Findings
 Typical signal of a cyst with hypointensity on T1-weighted and hyperintensity on T2-weighted images
Typical signal of a cyst with hypointensity on T1-weighted and hyperintensity on T2-weighted images
 Smooth demarcation
Smooth demarcation
Therapeutic Principles
 Therapy only with fracture or if at risk for fracture
Therapy only with fracture or if at risk for fracture
 No therapy if cortex is maintained and strong, or after puberty
No therapy if cortex is maintained and strong, or after puberty
 Curettage, filling with spongiosa chips, but up to 30% recurrence
Curettage, filling with spongiosa chips, but up to 30% recurrence
 Alternatively, evacuation of cyst with two needles and injection of corticosteroids every two months, three to five times (according to Campanacci, 1999)
Alternatively, evacuation of cyst with two needles and injection of corticosteroids every two months, three to five times (according to Campanacci, 1999)
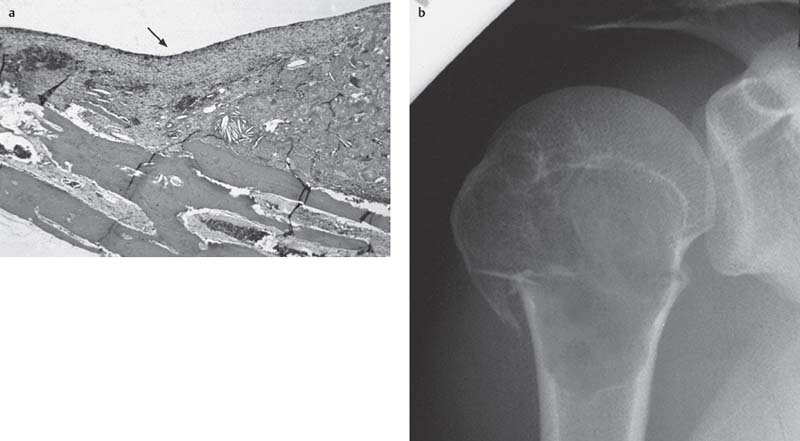
Fig. 5.7 a, b  Juvenile bone cyst in a 25-year-old female patient
Juvenile bone cyst in a 25-year-old female patient
a Histological section of the juvenile bone cyst. The membrane of the cyst is marked by a black arrow.
b Corresponding radiographic view of the juvenile bone cyst with a pathological fracture.
Therapeutic Principles
 Usually no therapy necessary, but follow-up is indicated
Usually no therapy necessary, but follow-up is indicated
 Surgical excision if larger than 5 cm, risk of fracture, proliferation, cosmetic problems, or other complaints
Surgical excision if larger than 5 cm, risk of fracture, proliferation, cosmetic problems, or other complaints
 Aggressive curettage or marginal en-bloc resection, filling with spongiosa chips
Aggressive curettage or marginal en-bloc resection, filling with spongiosa chips
Enchondroma
Definition
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


