CHAPTER 1 Ultrasound
Ultrasound is an interactive modality that integrates the art of the physical examination with modern high-resolution imaging technology. In some ways the evolutionary offspring of the stethoscope, ultrasound is a handheld diagnostic tool that is only as powerful as the experience and expertise of its user.
GENERAL PRINCIPLES OF ULTRASOUND TECHNIQUE
Ultrasound scanners use the piezoelectric effect to transform electricity into acoustic energy. The transducer serves to generate and transmit energy into the body, as well as to receive acoustic energy as it returns after being altered by tissues. Some of the many factors that influence image quality are listed in Box 1-1.
Transducer Array
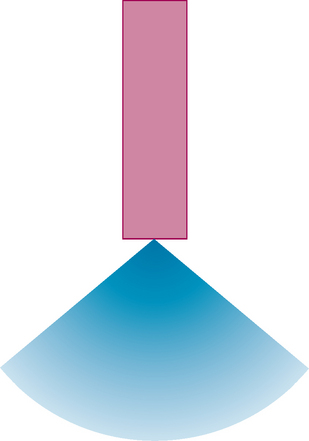
Sector Scanner
Sector scanners are the earliest type of transducer, and they utilize a single piezoelectric crystal. Because the source is a single point of oscillation, it results in a cone-shaped beam (Fig. 1-1). Sector scanners usually have a fixed range and are not in common use today.
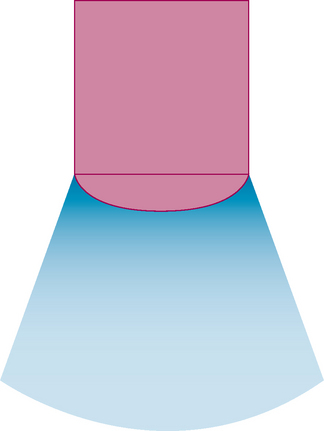
Curved Array
Curved array transducers have become the mainstay for most abdominal and pelvic applications. The convex surface results in a mildly diverging beam, optimizing anatomic coverage from a given window (Fig. 1-2). The smooth convexity also provides for patient comfort as the transducer is moved along the skin surface. Endocavitary transducers rely on small, curved arrays with high frequency to provide high-resolution images of the pelvic organs.
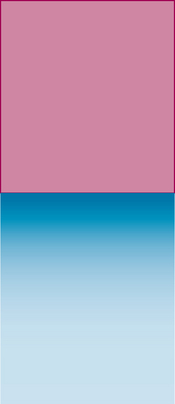
Linear Array
Using a flat footprint and high-frequency element, linear arrays have become the preferred transducer for most vascular applications, as well as for the evaluation of superficial small parts (testicles, thyroid). Parallel waves result in a rectangular field of view and provide for minimal distortion of anatomic structures (Fig. 1-3).
Phased Array
Phased array transducers orchestrate multiple elements activated in sequence to create a beam that can be steered electronically. Phased array transducers usually provide a cone-shaped field of view that appears similar to a sector scanner (see Fig. 1-1) but are more versatile because the beam can be steered from side to side. A small footprint makes these transducers useful when only a small sonographic window is available (e.g., intercostal approach, neonatal heads, postsurgical patients with wounds/bandages).
Transducer Frequency
Frequency selection is a key element that affects image quality. High-frequency transducers offer high-resolution imaging of superficial structures but are more susceptible to beam attenuation than low-frequency transducers. Low-frequency transducers provide better penetration, so they are useful for examining deep structures and large patients, but at a cost of lower image resolution. Thus a balance exists between the desired resolution and tissue penetration required to reach the object in question. In general, optimal image quality is achieved when using the highest frequency transducer that provides sufficient penetration. If that sounds subjective, it is! Frequent interaction between the radiologist and sonographer, rescanning patients with different transducers when necessary, will help achieve consistent image quality within an ultrasound department.
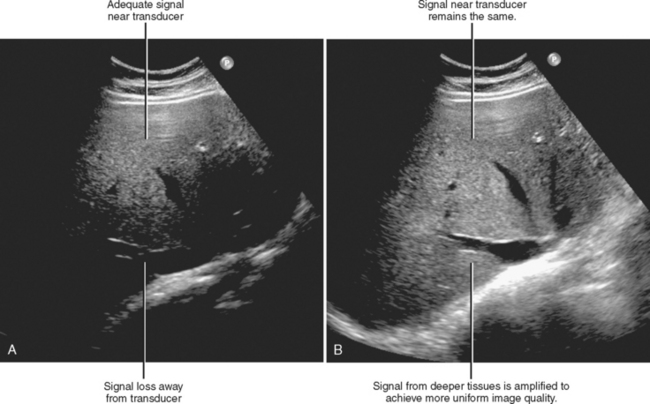
Gain
Because the tissues along the depth of a given field of view attenuate acoustic waves to a variable extent, a single gain setting cannot optimize image quality throughout the field of view. Time gain compensation is used to adjust gain settings according to depth to optimize gain throughout the image (Fig. 1-4).
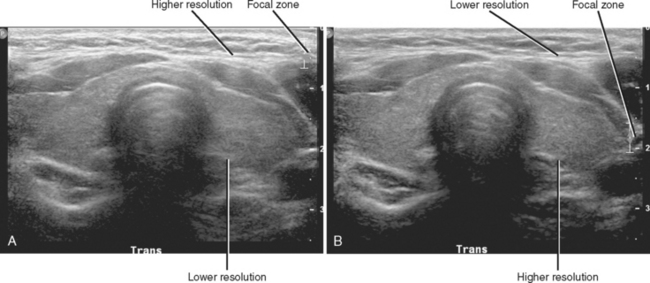
Focal Zone
The focal zone describes the distance from the transducer at which the beam is optimized for spatial resolution. In general, the focal zone should be adjusted to the depth of the object being examined (Fig. 1-5). Many transducers now provide multiple focal zones, allowing for more uniform image quality.
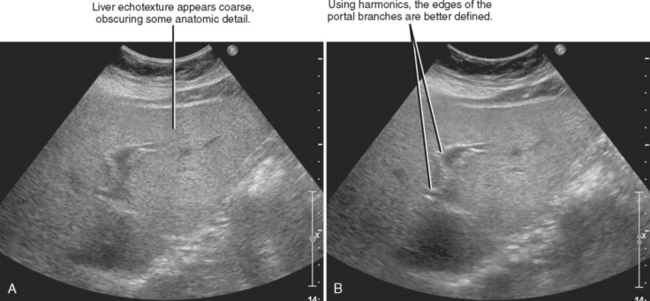
Harmonic Imaging
Although acoustic signal is transmitted at a specific frequency, the interaction of the beam with different tissues generates harmonic waves that resonate at frequencies that are double, triple, or quadruple the transmitted frequency. Because the types of tissue interfaces that generate most types of artifact do not produce harmonic waves, integrating harmonic information with the primary frequency improves the ratio of signal to noise (Fig. 1-6). Tissue harmonic imaging is particularly helpful with large body habitus or “noisy” tissues such as an echogenic liver.
COMMON ARTIFACTS
English dictionaries define the word artifact to mean something created by humans, whereas medical dictionaries define it as something that results from technique. In fact, every sonographic image is a human creation born of technical innovation. Perhaps the more common radiologic use of the word describes the unintended production of an image because of technical factors. This parsing of words may seem trivial, but despite the often negative connotation associated with the word artifact in the field of imaging, artifacts are sometimes a key diagnostic finding in sonography. Because the presence and recognition of an artifact can lead to diagnosis and the lack or recognition may lead to misdiagnosis, a basic understanding of the most common artifacts is critical to the effective use of sonography.
Acoustic Shadowing
Acoustic shadowing results when tissues absorb or reflect the incident ultrasound beam. Because there is no signal representing the tissues distal to that point, the image is replaced with a dark band along the projected course of the beam (Fig. 1-7). Shadowing is commonly seen with urinary or biliary calculi.
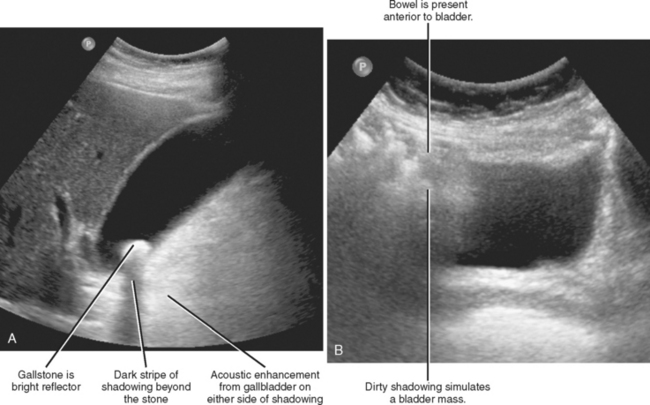
Figure 1-7 Different forms of acoustic shadowing include (A) clean shadowing and (B) so-called dirty shadowing.
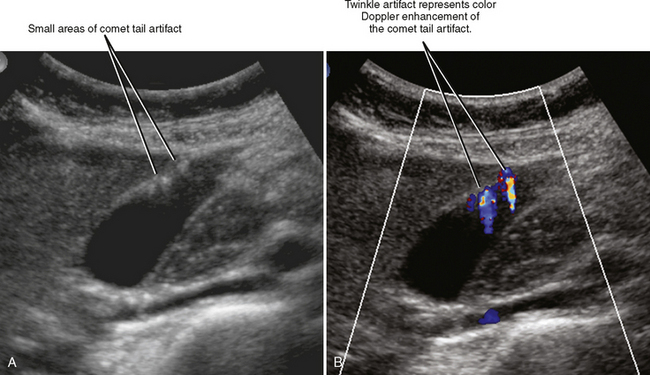
Calcium deposits and their interface with soft tissues can reflect and/or absorb ultrasound waves effectively. This has two main impacts on the ultrasound image: (1) a highly echogenic appearance at the near margin of the calcified object, and (2) a loss of signal beyond that object. The presence and type of posterior acoustic shadowing produced is related to the size and surface morphology of a structure. In the case of small calcium deposits, color Doppler can be used to increase conspicuity of tissue reflectivity in the form of the color comet tail artifact (CCTA), also called twinkle artifact (see Fig. 23-37 on CD-ROM).
Shadowing often results in a uniform dark stripe distal to the object, but this is not always the case. Although the authors prefer to avoid the term dirty shadowing, it is sometimes used in the literature to describe less uniform absorption, usually at soft-tissue interfaces or from gas (see Fig. 1-7). Although this has been reported to be helpful to identify structures or processes including lung, bowel, pneumobilia, and portal venous gas, caution must be applied. The sign is neither sensitive nor specific because there can be overlap with the more traditional shadowing.
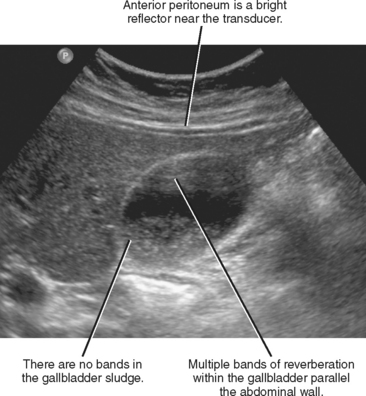
Reverberation
Reverberation occurs when acoustic energy “bounces” between two or more adjacent highly reflective surfaces. The result is a series of bands perpendicular to the beam, each representing a different delay in the return of energy to the transducer (Fig. 1-8). The effect is more pronounced when these surfaces are in the near field and in the center of the field of view. Reverberation artifact can be mistaken for sludge within the gallbladder, although examining the gallbladder from a different angle should eliminate the artifact. Reverberation is useful in creating the “comet tail” artifact characteristic of adenomyomatosis of the gallbladder wall. Color Doppler can be used to accentuate the reverberation effects of adenomyomatosis. The result is another form of CCTA (twinkle artifact) (Fig. 1-9).
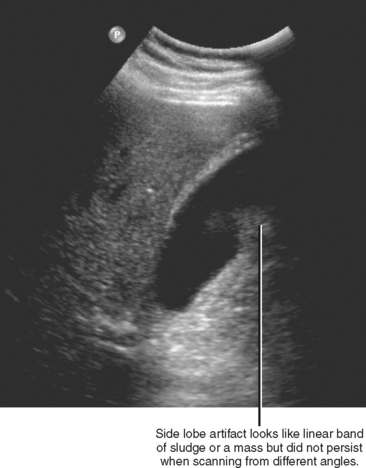
Side Lobe
Side lobes are the result of nonuniformity of the ultrasound beam at the periphery of the transducer. Although most of the beam is concentrated in the intended field of imaging, additional waves extend toward the periphery, out of the field of view. These “side lobes” typically account for only a minute component of the overall ultrasound energy, and only a small portion of it actually reflects back into the field of view most of the time. However, if those sound waves encounter an effective reflector and return to the field of view, they produce bands that are parallel to the primary incident beam. This is often seen as an apparent septation extending from the side of the gallbladder, the urinary bladder, or a simple cyst (Fig. 1-10). Unlike true septations, these bands will disappear or change with adjustment of the scan angle or focal zone.
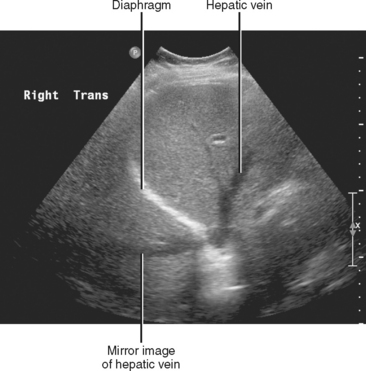
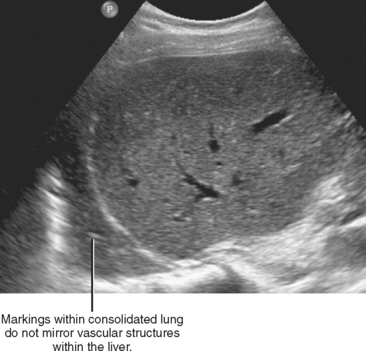
Mirror Image
Also known as multipath artifact, mirror image artifact is the result of the ultrasound beam “bouncing” off two strong specular reflectors before returning to the transducer. This is analogous to a billiard ball shot near a corner striking two cushions before returning to the shooter. Because the travel between the reflectors is not acknowledged by the ultrasound system, the result is duplication of the near-field image beyond the reflector. This occurs most commonly when the ultrasound beam reflects off two points of the diaphragm, resulting in projection of the liver into the thorax (Fig. 1-11). If structures do not precisely mirror the near field, consider alternative explanations for the image appearance (Fig. 1-12).
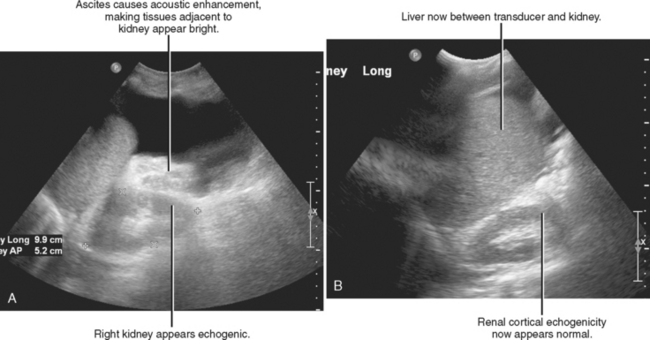
Acoustic Enhancement
Acoustic enhancement refers to a zone of increased signal (usually a bright stripe) seen deep to a structure with low acoustic impedance. This is most commonly seen deep to the gallbladder, urinary bladder, simple cysts, or large blood vessels (Fig. 1-13). Acoustic enhancement is usually omitted from lists of ultrasound artifacts, perhaps because of its utility in characterizing cystic structures. Nonetheless, acoustic enhancement is merely an unintended technical phenomenon, and although it is often useful, it can also lead to errant diagnosis if unrecognized. For example, ascites in the hepatorenal space can make the kidney appear echogenic, prompting an inaccurate diagnosis of diffuse renal parenchymal disease (Fig. 1-14).
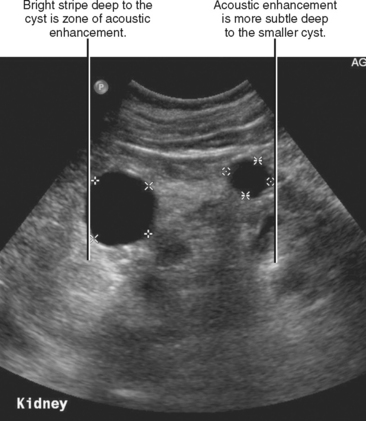
Figure 1-13 Ultrasound image of the right kidney shows two renal cysts causing acoustic enhancement.
ULTRASOUND OF THE UPPER ABDOMEN
Ultrasound of the Liver
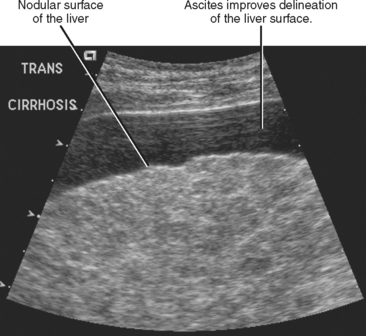
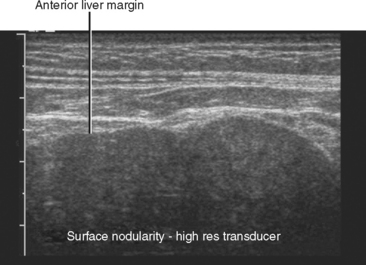
The liver is best imaged with the patient in the supine and left lateral decubitus positions, starting with 3- to 7-MHz curved array transducers. In most cases, harmonic imaging improves image quality in the liver. A subcostal acoustic window should be attempted first, supplemented with intercostal scanning as necessary. The liver surface (usually the ventral left lobe) should be evaluated for nodularity with a near-field, optimized, 5- to 12-MHz linear array transducer. It is easier to appreciate subtle nodularity during real-time examination or on video clips than on hard-copy images. Furthermore, surface characteristics are easier to appreciate when ascites is present (Fig. 1-15) Angling the transducer so that it is not perpendicular to the liver surface may falsely simulate nodularity.
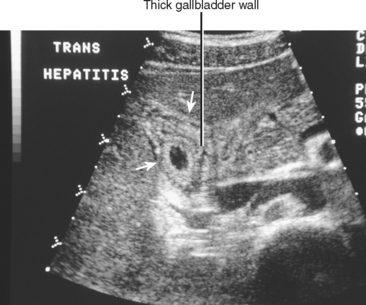
Viral Hepatitis
No specific sonographic findings are found in acute hepatitis. The most common sonographic finding in hepatitis is probably hepatomegaly, although this is easily overlooked. The so-called starry sky pattern, increased periportal echoes coupled with decreased parenchymal echogenicity, is relatively insensitive for the detection of acute viral hepatitis. In one series, the starry sky liver pattern was found in only 19 of 791 patients with viral hepatitis. In the same study, there was no difference in sonographic findings between a control group and patients with acute viral hepatitis. Marked gallbladder wall thickening is sometimes present in patients with acute hepatitis (Fig. 1-16).
Hepatomegaly and heterogeneously increased echogenicity are common in chronic hepatitis and are related to the amount of fatty infiltration and fibrosis present. The liver surface is smooth, unless cirrhosis is also present. In chronic active hepatitis, enlarged arteries are noted on color Doppler sonography because of increased arterial flow. This may cause a “double-channel” sign on grayscale images that can be confused with biliary dilatation. Lymph nodes are often detected in the hepatoduodenal ligament.
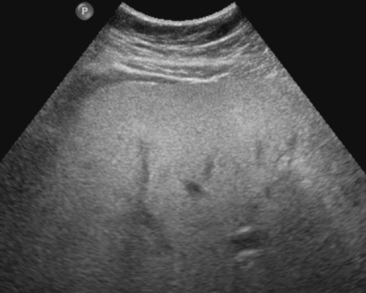
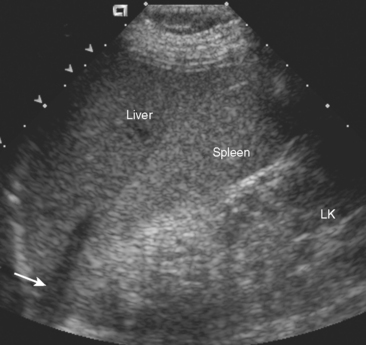
Steatohepatitis
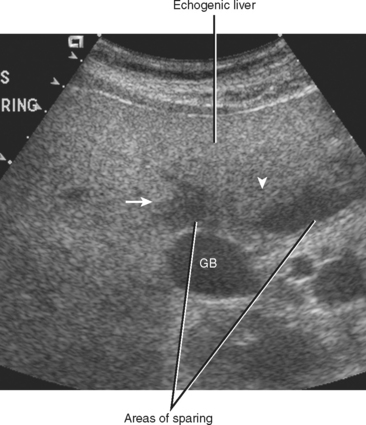
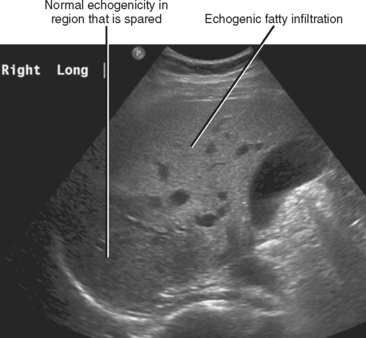
Severe fatty infiltration of the liver often results in hepatomegaly and diffusely increased echogenicity (Fig. 1-17). Acoustic penetration may be decreased, resulting in indistinctness of blood vessels and the diaphragm. Hepatic echogenicity is usually equal to or greater than that of the renal cortex. Although subjective assessment of the renal cortex and liver parenchyma echogenicity is useful in severe fatty infiltration, this approach is error prone and insensitive. Although unproven, we prefer to use the relative echogenicity of the kidneys compared with the spleen and liver (Fig. 1-18). The normal spleen is slightly more echogenic than the normal liver. Therefore, if the difference in echogenicity between the liver and right kidney is greater than the difference between the spleen and left kidney, the liver parenchyma has abnormally increased echogenicity. This approach assumes, of course, that the echogenicity of the kidneys is equal bilaterally.
Fat deposition and sparing are not always uniform, with focal (Fig. 1-19) and regional (Fig. 1-20) differences possible within the liver. Patterns of fat deposition and sparing are discussed in more detail in Chapter 12.
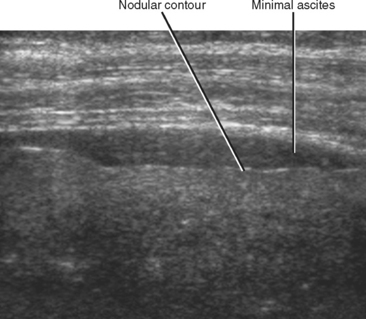
Cirrhosis
Cirrhosis is the end stage of chronic hepatocellular injury, characterized by bridging fibrosis and regeneration. The most common sonographic findings in cirrhosis are listed in Table 1-1. Unfortunately, many of these signs are insensitive and insufficiently specific for cirrhosis to be diagnosed reliably with sonography. Furthermore, the extent of sonographic changes is not a reliable predictor of disease severity. Nevertheless, evaluation of the liver surface with a high-resolution linear array transducer is useful because surface nodularity may be the only sonographic sign of cirrhosis (Fig. 1-21). Be aware that metastases to the liver can also result in a nodular liver contour, and this nodularity may be the only indication of metastatic disease in patients with a known primary malignancy (Fig. 1-22).
Table 1-1 Sonographic Findings of Cirrhosis
| Finding | Comments |
|---|---|
| Nodular liver surface | More specific than sensitive; however, also consider metastatic disease if patient has known primary malignancy |
| Echogenic liver | Nonspecific, commonly seen with fatty infiltration |
| Flow reversal in portal vein | Specific finding, although transient reversal occasionally seen with cardiac disease |
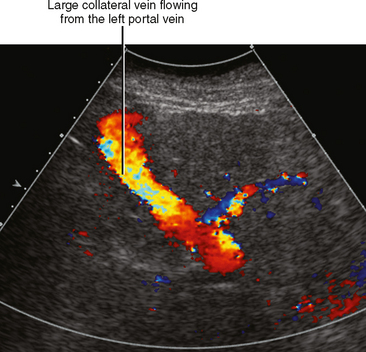
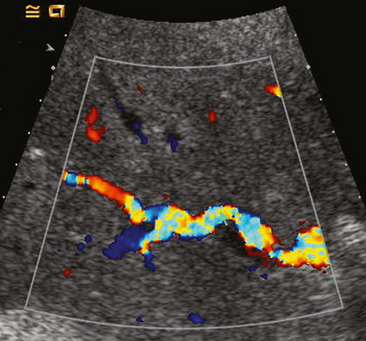
| Collateral venous flow | Specific finding when present (Fig. 1-23) |
| Enlarged hepatic arteries (Fig. 1-24) | Also seen with portal vein thrombosis and arteriovenous shunting |
| Narrowing of the hepatic veins and intrahepatic IVC | Dampens transmission of cardiac waveform (see Fig. 1-25) |
IVC, Inferior vena cava.
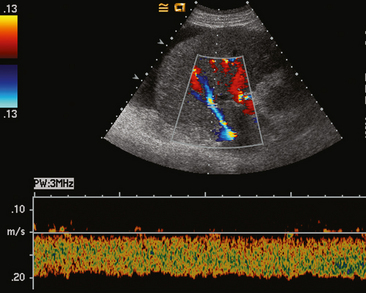
Color Doppler sonography can show portal vein flow reversal or portosystemic collaterals, suggesting the diagnosis of portal hypertension (Fig. 1-26). Because considerable variation exists in the size of the portal vein with changes in respiration and patient position, absolute portal vein diameter is not a reliable predictor of portal hypertension. In fact, a lack of respiratory variation (an increase in portal vein diameter during inspiration and a decrease during expiration) can indicate portal hypertension. Other portal flow abnormalities include bidirectional flow and, rarely, nearly static blood flow. Be aware that transient portal flow reversal also occurs in some clinical conditions not related to liver disease such as tricuspid regurgitation and heart failure (Fig. 1-27).
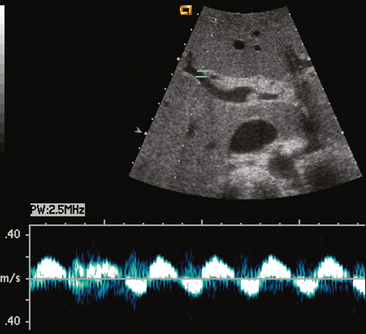
Figure 1-27 Spectral Doppler imaging shows a biphasic waveform in portal vein in patient with tricuspid regurgitation.
Sonography also plays an important role in the evaluation and follow-up of patients with known liver cirrhosis. Although focal fatty infiltration, regenerating nodules, and other benign lesions can occur in a cirrhotic liver, any sonographically detected mass within a cirrhotic liver should be considered suspicious for hepatocellular carcinoma (HCC) and referred for additional diagnostic evaluation.
Focal Liver Lesions
The sonographic appearance of hydatid disease in the liver can range from simple cystic to complex, demonstrating calcifications, mural nodules, and the so-called water lily sign. The latter finding represents separation of the endocyst layer of the hydatid cyst. When a hydatid cyst has dense egg-shell calcification, the shadowing produced from the reflected echoes may simulate a granuloma or be confused with other solid lesions (Fig. 1-28).
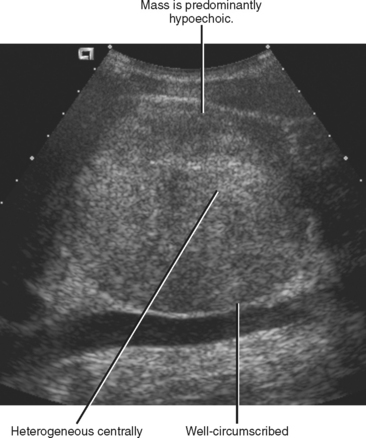
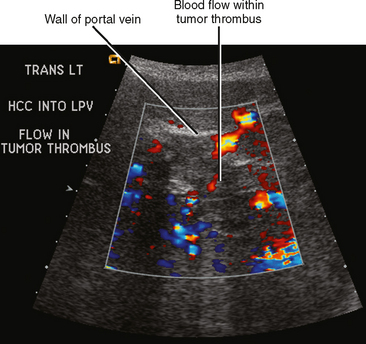
In the United States, 85% of HCCs occur in patients with cirrhosis or precirrhotic conditions. Small HCCs (<5 cm) are often hypoechoic. With further progression, lesions become more numerous and heterogeneous, and often develop a hypoechoic peripheral rim (Fig. 1-29). Advanced HCC is often multifocal, making it difficult to distinguish from metastatic disease. Echogenic nodules are fairly common in multifocal HCC (Fig. 1-30). Fatty metamorphosis of HCC also causes increased echogenicity and can result in confusion with hemangioma. A mass associated with invasion of the portal or hepatic veins should suggest the diagnosis of HCC (Fig. 1-31), although other liver tumors occasionally invade venous structures. About three-fourths of HCCs have identifiable internal color flow, a feature present in only one-third of metastases.

Figure 1-30 Sonographic appearance of multifocal hepatocellular carcinoma as multiple echogenic masses.
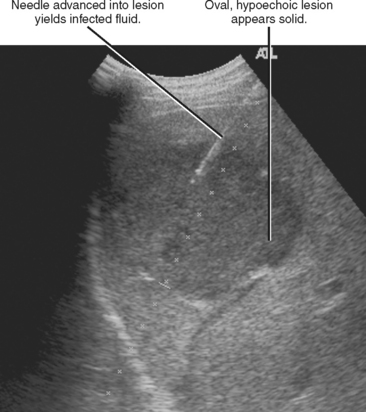
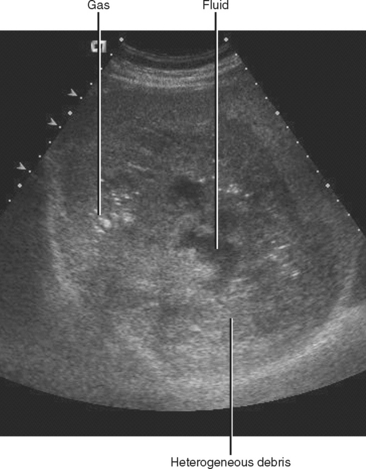
Because patients presenting with right upper quadrant pain, fever, and leukocytosis usually undergo an ultrasound as the initial imaging examination, liver abscesses are frequently identified with ultrasound. The sonographic appearance of liver abscess is quite variable. Abscesses are usually round or oval and hypoechoic with irregular margins (Fig. 1-32). The abscesses can be homogeneous or inhomogeneous. They may also simulate solid masses, and acoustic enhancement is frequently absent. Often, the internal contents of a liver abscess can be seen to move during real-time sonography, distinguishing it from a solid tumor.
The presence of echogenic fine foci within the abscess usually indicates microbubbles (Fig. 1-33). Microbubbles can also simulate the appearance of blood flow within some abscesses on color Doppler. Large, confluent pockets of gas within an abscess can be confused with bowel gas, particularly in right lobe abscesses close to the diaphragm.
Cavernous hemangiomas are usually well-defined, echogenic lesions that blend with the normal liver without distinctive halos and have enhanced through transmission. Larger hemangiomas frequently diverge from this pattern, with mixed echogenicity or even hypoechoic lesions (Fig. 1-34
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree