Fig. 2.1
Measurement of the ovary, with a sonographic window provided by the full bladder
Different types of probes operate at different frequencies. The human ear can detect sound from 20 to 20,000 Hz. Routinely used ultrasound probes are found with a range of operating frequencies, typically from 3.5 MHz to 11+ MHz (11,000,000 Hz). Higher frequency probes produce higher quality images but are unable to penetrate deep into the body. Thus, there is a trade off between depth of visualization and image detail. The workhorse abdominal imaging probe operates at around 3.5 MHz.
Normal imaging is performed using the setting termed M-mode (Fig. 2.2a), which gives a real-time two-dimensional representation of the tissue examined. Doppler imaging allows information on the direction of flow of blood within a tissue; by convention, red is towards the probe and blue is away (Fig. 2.2b). Pulse wave and continuous wave Doppler enable the analysis of vascular flow within a small, user-defined area of interest inside a vessel, to give information on waveform, velocity and direction (Fig. 2.2c). Both of these additional modes consume capacity within the probe, further limiting the useful working depth of a probe.
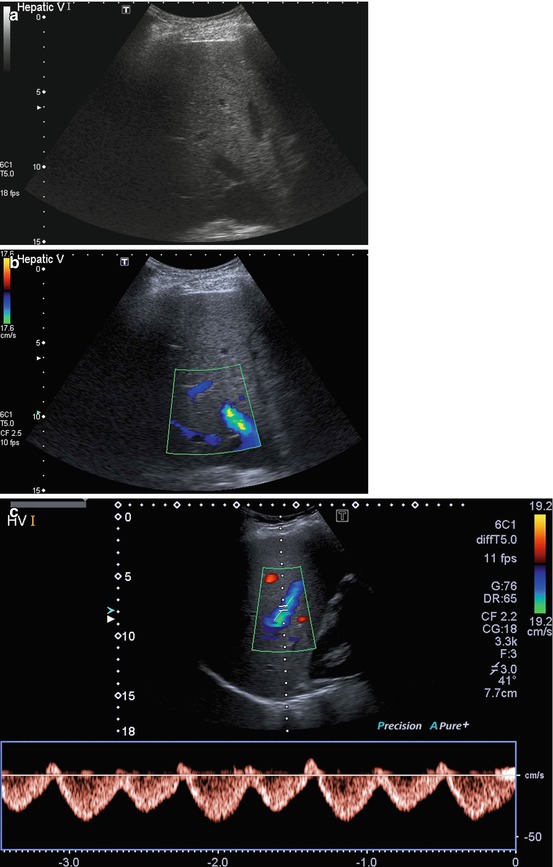
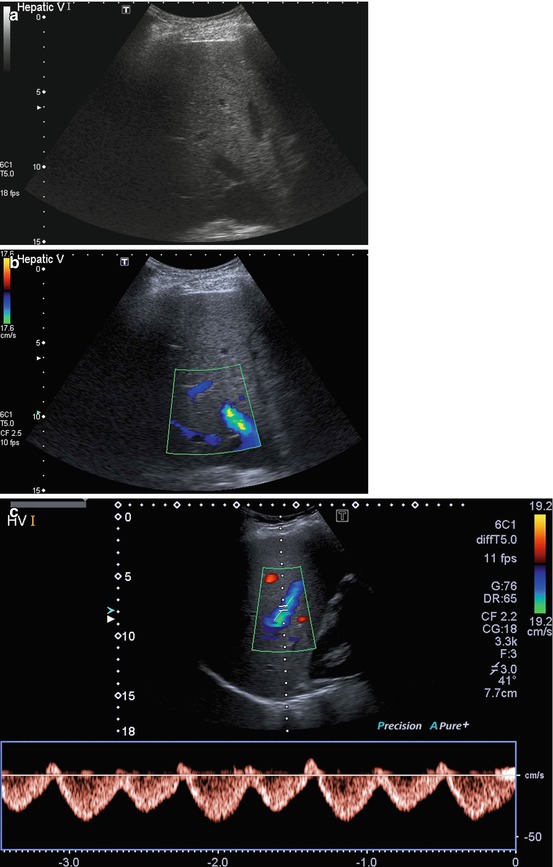
Fig. 2.2
(a–c) Images of the hepatic veins. (a) Uses M-mode to give an anatomical overview. (b) Is a Doppler image, with blue colours indicating flow away from the probe. (c) Shows the phasic pulse wave Doppler signal often shown by the hepatic veins
Strengths
While some ultrasound machines can be bulky, portable versions are becoming more commonplace, and diagnostic quality images can now be produced using a machine the size of a laptop. Once in place at the bedside, the image acquisition is through a maneuverable and lightweight probe. Diagnosis of an unstable patient in the safety of the ICU is an important benefit of ultrasound. Some studies have found value in routine ultrasound of all ICU patients. Use of ultrasound has been shown to diagnose previously unknown pathology and potentially avoid the need for more complex investigations, such as CT, which involve transfer.
There are theoretical risks of tissue heating from prolonged ultrasound examination at one site, but under normal circumstances ultrasound is a completely safe investigative procedure. This allows repetition of examination; if clinical need dictates, pathology can be reassessed at short intervals.
Ultrasound provides functional, morphological as well as physiological information. Assessment of vascular flow is often important (Fig. 2.3). While cross sectional modalities may typically only indicate vascular patency, ultrasound can ascertain flow direction, velocity and waveform.
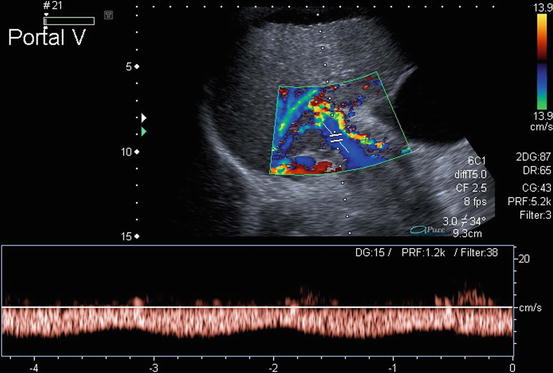
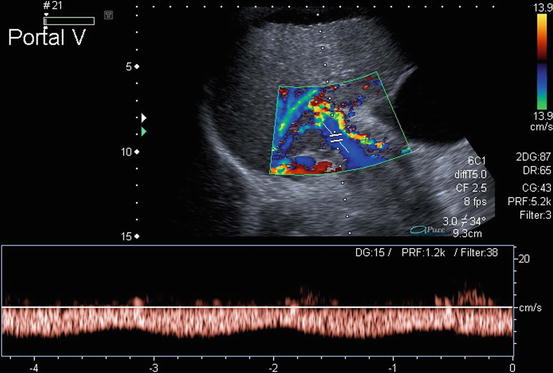
Fig. 2.3
Pulse wave Doppler image of the portal vein, showing flow away from the liver (hepatofugal), in a patient with decompensated cirrhosis
Image guided intervention has made a number of bedside procedures safer. A skilled operator can use ultrasound to track placement of a needle in any plane that can be visualized by the probe (Fig. 2.4). Sites can be targeted easily using ultrasound by choice of the most direct route, avoiding vascular and other structures. At the same time the success of the intervention can be controlled. Ultrasound guided procedures in the ICU regularly include vascular cannulation, fluid aspiration, drain placement or tissue biopsy.


Fig. 2.4
Ultrasound guided insertion of an ascitic drain; the white arrow indicates the needle inserted into the ascites, to allow passage of a guide-wire
Limitations
The limitations of ultrasound result from the transcutaneous method of image acquisition. It is mainly physical factors that limit the view obtained. The most common examples are:
Patient body habitus – overweight patients can be extremely difficult to scan. As already discussed, fat has a negative effect on image quality (Fig. 2.5a, b). When considering the value of an ultrasound request, or report, this should always be born in mind.
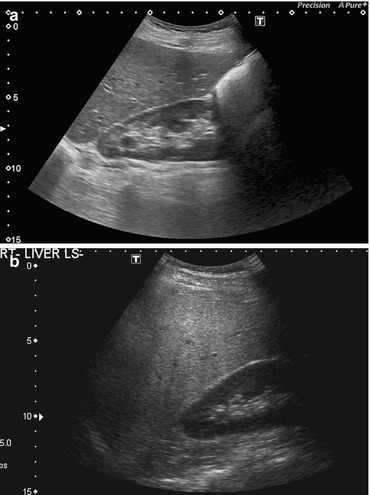
Fig. 2.5
(a) Illustrates the normal relationship between kidney and liver, with the liver parenchyma slightly more echogenic than the renal cortex. (b) Is a patient with hepatic steatosis; the liver is markedly echogenic. The absorption of the sound wave results in poor visualisation of the deeper aspects of the liver
Patient mobility – the highest quality ultrasound images are obtained in a mobile, cooperative patient. This may include turning the patient to give access to the site where the tissue of interest is closest (e.g., posteriorly for the kidneys). Suspended respiration removes respiratory motion artifact, and a deep breath may move subdiaphramatic organs below the shadows cast by the ribs. Neither turning, nor respiratory control, may be possible in critically ill or injured ICU patients. Easy to perform US guided procedures might become impossible to do in immobile patients; e.g., pleural effusions tend to collect posteriorly in the supine patient, making it difficult to reach them and leading to false negative results.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree