Long-Term Ultrasound Follow-Up of Liver Transplantation
Introduction
Ultrasound plays a vital role in the long-term follow-up of liver transplant patients.1,2 Ultrasound provides a simple first-line noninvasive imaging modality to assess the graftfor structural complications; disease recurrence in the graft is an important cause of morbidity and mortality in the transplant patient.3 Long-term complications of immunosuppression may be assessed with ultrasound. In our institution all post-transplant patients undergo a color Doppler ultrasound examination immediately prior to clinical follow-up, with results available to the consulting hepatologist.
Ultrasound is the imaging modality of choice in patients who develop symptoms or deranged biochemical parameters at any stage following liver transplantation. A detailed knowledge of the surgical anatomy of the transplant graft (including older surgical techniques) is required for accurate assessment of the graft at follow-up. The following chapter reviews the possible long-term structural complications that can occur in the transplanted liver, with disease recurrence dealt with in the context of initial indications for transplantation, and complications of long-term immunosuppression are examined.
Vascular Complications
All vascular complications discussed in the previous chapter are relevant in the long-term surveillance, with some important differences.
Hepatic Artery
The main hepatic artery “proper” and the left and right branches should be examined with color Doppler ultrasound with a spectral Doppler waveform recorded. Color Doppler studies of the intrahepatic arterial tree become more difficult to interpret with time after the operation. A normal hepatic artery spectral Doppler waveform on serial examinations accurately excludes significant hepatic artery disease.4 The diagnosis of hepatic artery stenosis may be inferred using color Doppler imaging if serial hepatic arterial spectral Doppler waveform shows a progressive reduction in arterial velocity and the development of the tardus parvus waveform in the absence of parenchymal abnormality.5–7 Angiography should then be recommended.
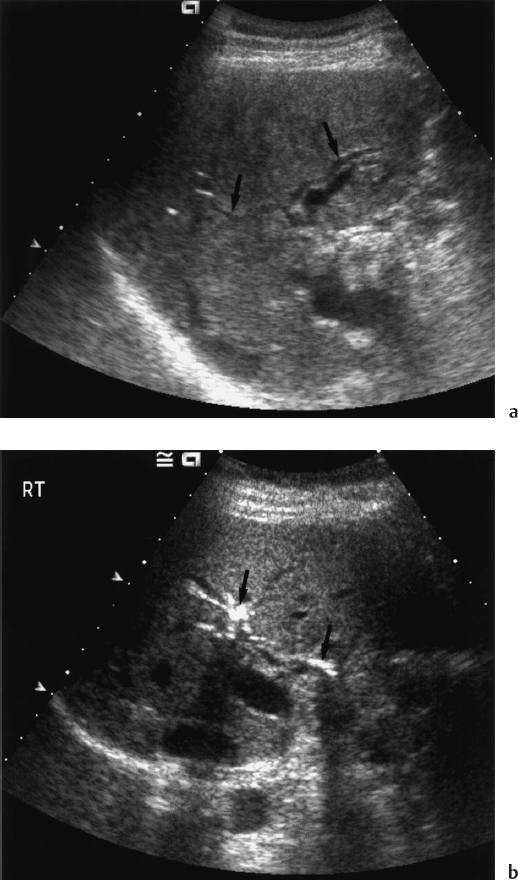
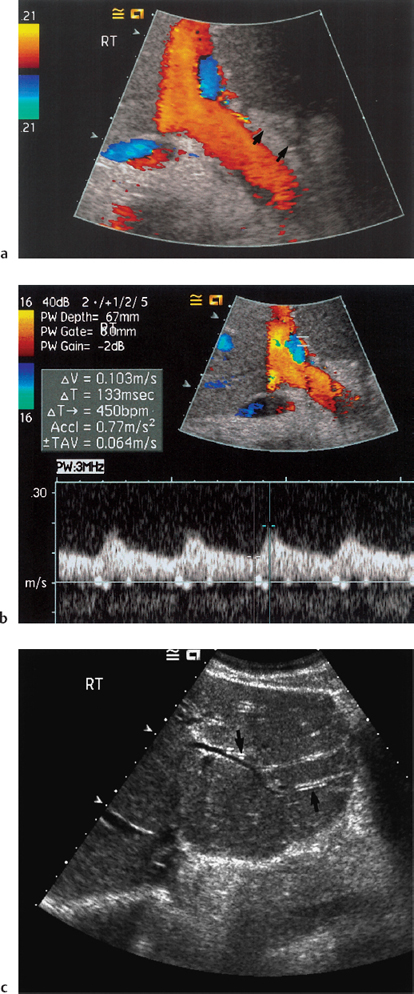
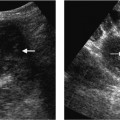
Fig. 11.1 a Roux-en-Y loop in a transplant patient. Narrowing at the anastomosis site has produced intrahepatic bile duct dilatation (arrows). b Roux-en-Y loop allows free reflux of air from the jejunal bowel loop, producing “aerobilia” (arrows)
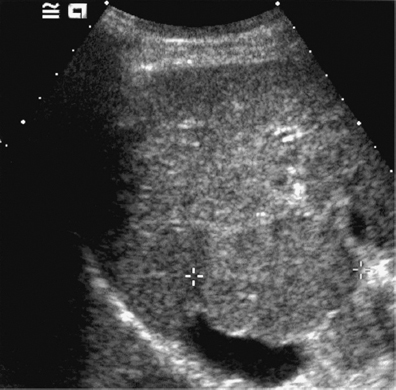
Hepatic artery stenosis and occlusion over a long period may have less devastating immediate consequences to the liver graft than acute hepatic artery occlusion in the immediate post-operative period. If the hepatic artery narrows and subsequently becomes occluded, graft function maybe preserved by the formation of a number of collateral arteries. Furthermore, when a Rouxen-Y loop is fashioned in children or adults (Fig. 11.1), replacing a recipient common bile duct, the highly vascular jejunal bed allows rapid collateralization and protects the graft from acute ischemic complications.5 In the event of the establishment of a good collateral supply, an entirely normal intrahepatic spectral Doppler waveform may be demonstrated even in the presence of complete main hepatic artery occlusion (Fig. 11.2). A more common finding is the damping of the intrahepatic systolic arterial spectral Doppler waveform with the maintenance of high diastolic spectral Doppler waveform.8 Hence, the presence of hepatic arterial flow within the graft must be taken in the clinical context of graft function.
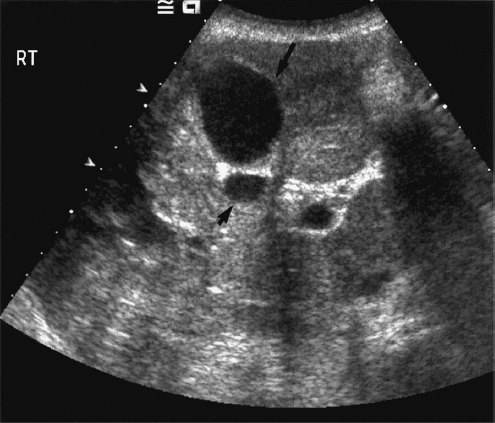
Although late arterial occlusion may be clinically silent, the majority of patients suffer one or more complications.9 In the first few weeks after transplantation, arterial occlusion may present as a biliary leak. However, if the biliary tree survives the initial ischemic event, then biliary strictures may develop, particularly at the hilum of the left and right ducts.10 This in turn may lead to infective complications suchascholangitis and biliary abscess formation. Hepatic abscess formation is also more common with chronic ischemia (Fig. 11.3).9
Portal Vein
Portal Vein Occlusion
Immediate portal vein complications are rare, with portal vein thrombosis occurring in fewer than 2% of cases of liver transplantation.11 Long-term portal vein occlusion is a rare late consequence of transplantation (Fig. 11.4). It is seen in patients with conditions predisposing to an increased incidence of portal vein thrombosis: coagulopathies, Budd-Chiari syndrome, abnormal portal vein anatomy including cases of cut-down liver or live related donor patients with a portal vein conduit, or patients who have had an operative thrombectomy.11 Acute portal vein occlusion presents with graft dysfunction and signs and symptoms of portal hypertension. Ultrasound will demonstrate thrombus and features of portal hypertension.
Portal Vein Stenosis
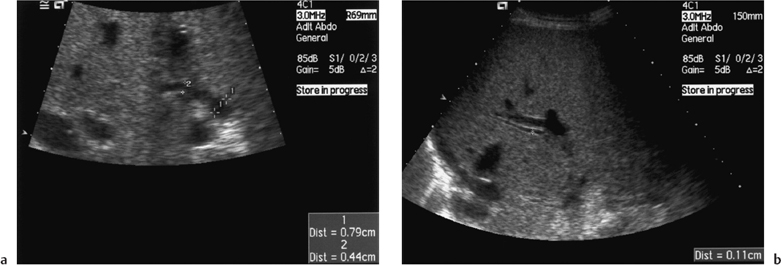
Portal vein stenosis is a rare but important complication, which can lead to portal hypertension and portal vein thrombosis.12 Turbulent flow is common at the portal vein anastomotic site, and this tends to be the area where a stenosis occurs (Fig. 11.5). Patients with portal vein stenosis usually have increasing portal vein velocity measurements and increasing spleen size over time, with a portal vein that demonstrates “waisting,” i.e., pre- and poststenotic dilatation.13
A portal vein peak systolic velocity of 1.00 m/s indicates significant hemodynamic stenosis that warrants further investigation. In children with a left lobe graft the portal vein may become “stretched” following hypertrophy of the transplanted left lobe. This results in portal vein occlusion, which may be treated using a jump graft. Serial measurements of the spleen should be made at all ultrasound examinations, as an increase in spleen size may be an indicator of portal hypertension.
gg
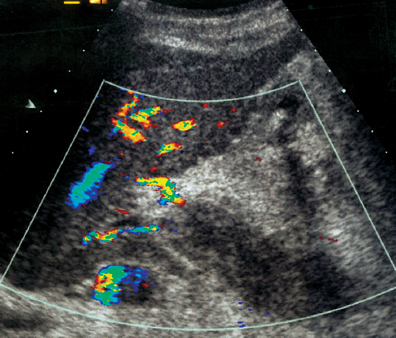
Fig. 11.4 Portal vein occlusion following liver transplantation
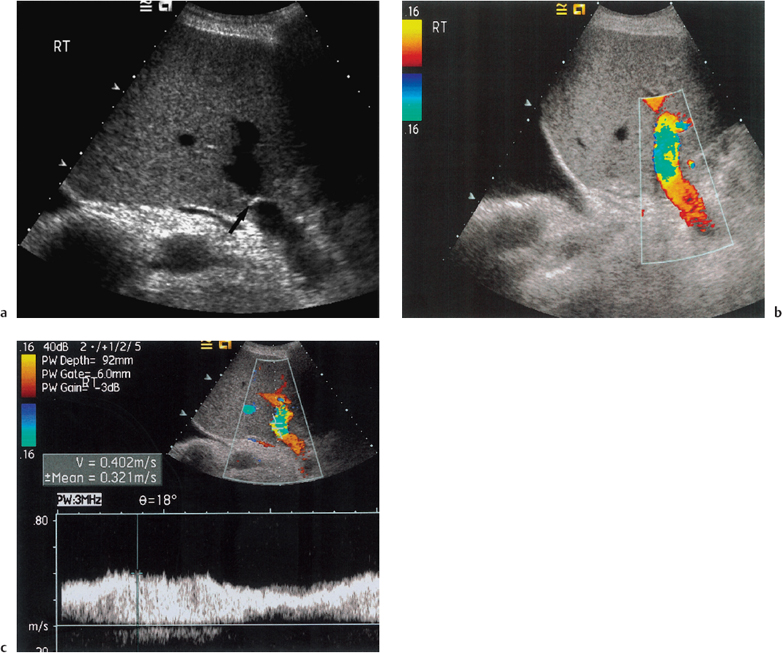
Fig. 11.5 a Suture material is seen as an echogenic area (arrow) in the portal vein. b Minor narrowing with turbulence on color Doppler imaging is present at the anastomotic site in the portal vein. c Spectral Doppler analysis demonstrates a velocity of 0.40 m/s, not suggestive of a stenosis of the portal vein
Inferior Vena Cava
Thrombosis or stenosis of inferior vena cava (IVC) anastomoses are rare, occurring in less than 1-4% of patients, and are usually due to technical surgical problems or a consequence of compression by a fluid collection.14 Infrahepatic stenosis may cause only lower extremity swelling. Suprahepatic stenosis presents with a Budd-Chiari-like picture of ascites, liver enlargement, and pleural effusion. Color Doppler studies will demonstrate these changes and demonstrate absence or dampening of the normal hepatic vein spectral Doppler waveform. There may also be distension of the hepatic veins and IVC.15
 Summary point:
Summary point:
- A normal hepatic artery spectral Doppler waveform on serial ultrasound examinations accurately excludes significant hepatic artery disease
- Hepatic artery occlusion and stenosis over a long period may have less devastating consequences for liver graft function than acute hepatic artery occlusion in the immediate postoperative period; hepatic abscess formation is more common
Nonvascular Complications
Renal Complications
Renal insufficiency due to nephrotoxic effects of the immunosuppressive therapy is a common complication and has been reported in up to 25% of pediatric recipients.16 Ultrasound may be used to exclude obstruction in patients with deteriorating renal function and give information about the size and reflectivity of the kidneys.
Graft-Versus-Host Disease
Graft-versus-host disease is a common complication following bone marrow transplantation and is becoming increasingly recognized following solid organ transplantation.17 It has serious consequences and may be fatal. Imaging has no role in the assessment of graft versus host disease other than to exclude structural abnormalities of the graft.
Rejection
Rejection is common in liver transplant recipients but imaging is neither sensitive nor specific for detecting rejection.18 Ultrasound is used to exclude structural abnormalities in the graft that may have a similar clinical presentation to rejection. The diagnosis of rejection is made on histological study following liver biopsy.
Infection
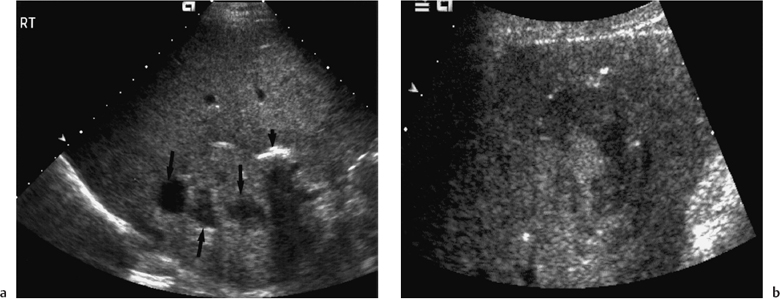
Infection is the most common complication of liver transplantation, with immunosuppressive therapy the major risk factor.19 In the presence of a structural abnormality of the graft, such as hepatic artery thrombosis or a biliary stricture, infection may be localized to the graft. Hepatic abscess formation may be readily visualized with ultrasound and treated by ultrasound-guided drainage. Abscesses may be visualized as either increased echogenicity or decreased echogenicity (Fig. 11.6). A retrospective review of adult liver transplantation over a nine-year period demonstrated an incidence of hepatic abscess of 3.9%.9 Eighty-five percent of abscesses were bacterial in origin, 15% fungal and contributed to eventual graft failure.
Biliary Complications
The current surgical practice for biliary reconstruction is end-to-end anastomoses, where the recipient bile duct may be used. However, if the recipient has an underlying biliary abnormality with an insufficient length of common bile duct, such as in biliary atresia or sclerosing cholangitis, or when a cut-down graft is transplanted, it will be necessary to construct a Rouxen-Y-loop.
Bile duct dilatation is unusual in the early postoperative period.6 On ultrasound, in the early postoperative period it is practice to measure the common, left, and right bile ducts to confirm nondilatation and record the baseline measurement. Thisisparticularly important in cut-down grafts in children, where intrahepatic bile duct dimensions are of adult proportions and early measurement will avoid an erroneous call of bile duct dilatation. The presence of a normal biliary system on ultrasound makes the presence of a structural biliary complication unlikely.2 If the bile duct size increases are accompanied by biochemical changes or persist for more than three months after transplantation, a biliary system abnormality is invariably present and cholangiography is then required (Fig. 11.7).2
Nonanastomotic biliary strictures at the hilum of the liver are most commonly associated with ischemia as a consequence of hepatic artery stenosis or thrombosis.10,20 Other established causes of nonanastomotic strictures include chronic rejection and infection, particularly with cytomegalovirus.2 Anastomotic strictures arise secondary to operative difficulties and respond to transhepatic balloon dilatation.21 A small group of patients with postoperative biliary system obstruction have extensive epithelial casts forming within the biliary tree (Fig. 11.8). These patients usually have a patent hepatic artery, suggesting that the lesions are unlikely to be vascular in origin. It is possible that this is a late manifestation of preservation injury affecting the harvested liver, leading to epithelial sloughing within the biliary system. Most patients with this condition require retransplantation.22
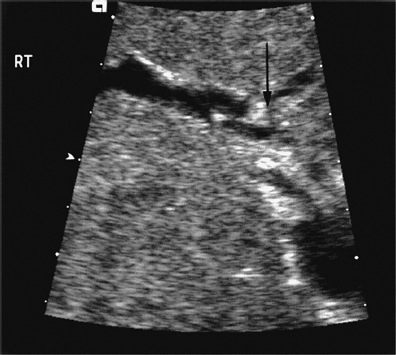
Fig. 11.8 Intrahepatic bile duct dilatation, with echogenic material (arrow) within the bile ducts, in a liver transplant patient
 Summary point:
Summary point:
- Renal insufficiency due to nephrotoxic effect of immunosuppressive therapy is a common complication, occurring in 25% of pediatric liver transplant patients
- Imaging is not specific for rejection
- Immunosuppressive therapy is a risk factor for infection
- Nonanastomotic biliary strictures are associated with ischaemia.
Disease Recurrence
The initial indication for liver transplantation should be taken into account (although not often offered by the referring physician) when surveillance ultrasound is performed in the post-transplant phase, to allow for the possibility of disease recurrence.
Viral Infection
Viral infection does recur in the transplant liver. Biopsy evidence of recurrence of hepatitis C is seen in 87% of transplants and tends to occur within two years of transplantation.23
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree