4 Ultrasound-guided Interventions After mammography, ultrasound (US) is the second most important diagnostic breast imaging tool. Aside from its use in distinguishing between cystic and solid lesions, the device-related technical advances of the last years have afforded breast US an excellent capacity for differentiating between benign and malignant solid findings. Modern equipment technology and standardized examination technique make breast US an excellent diagnostic tool. In the hands of an experienced examiner, it has a sensitivity of 57–90% and a specificity of 60–90%. Dense parenchyma. Breast US is an important adjunct to mammography in the early detection of breast cancer. This is especially true when breast tissue composition is dense (American College of Radiology [ACR] density types III–IV) where the mammographic detection of noncalcifying breast cancer is limited. Many workgroups also favor the employment of breast US for women with scattered fibroglandular densities (ACR density type II). Studies have shown that an additional 3–4 per 1000 clinically and mammographically occult breast cancers can be detected through the adjunctive use of breast US in women with dense breast tissue. Importantly, these additionally detected tumors do not differ in size or stage from the mammographically detected, clinically occult breast cancers. Hence, experienced ultrasonographers can detect most focal masses with a diameter greater than 5–10 mm. Ambiguous palpable findings. Breast US is obligatory in the diagnostic work-up of ambiguous areas of palpable thickenings or lumps, with or without correlating findings on mammography or magnetic resonance (MR) mammography. In addition, it is a helpful adjunctive tool in the evaluation of clinically occult, mammographic, or MR mammographic findings. In women under 35 years of age, breast US is the diagnostic examination of first choice for working up ambiguous clinical findings. With this approach it is often possible to clearly assess a clinically conspicuous finding as harmless (e. g., bland cyst) and avoid unnecessary diagnostic imaging. If US reveals an ambiguous correlating finding, further work-up including mammography is mandatory. Core needle biopsy. US-guided minimally invasive biopsy of ambiguous findings is an accurate, rapid, safe, and cost-efficient method for harvesting representative tissue. For these reasons, US-guidance is preferred over other biopsy guidance techniques in the diagnostic and preoperative setting. A retrospective US examination should always be performed when an ambiguous focal mass is detected on mammography or MR mammography, and is also recommended even when the primary examination has shown no conspicuous findings (“second-look” US). Detection of a correlating lesion is often facilitated in awareness of lesion size, configuration, and position, and can then be subjected to a US-guided large core needle biopsy (CNB). Breast examination. Breast US is a real-time examination of breast sections. The patient is examined in the supine position with her arms raised and hands placed under her head or neck. The examination of a patient with large breasts can be facilitated by elevating the side to be examined (e. g., by placing pillows under the ipsilateral shoulder/back) to achieve a more even distribution of breast tissue on the chest wall. The transducer is best held at its base and moved primarily by wrist motions. A gel-like solution is applied to the skin to promote US wave transmission through the skin. Care should be taken that contact between the transducer and the breast is uniform and perpendicular to the surface. The weight of the transducer and hand is usually sufficient pressure to ensure good US wave transmission. As a rule, exerted pressure should be as light as possible, but as heavy as necessary to obtain good images. A systematic examination of the breast can be achieved by moving the transducer in the mediolateral direction with overlapping sagittal scan planes. Especially in the examination of large breasts, it is often helpful to image the lateral aspects in transversal planes. Radial imaging is particularly good for the assessment of ductal structures. Because US is a dynamic examination, it is possible to assess and document the spatial dimensions of a finding by rotating the scan plane. This is important to differentiate a true, 3D lesion from a pseudolesion seen in only one plane. By varying/increasing compression exerted with the transducer, US wave transmission through breast tissue is improved and the elasticity of a lesion can be assessed. Axillary examination. The US examination of the axilla should be performed routinely in follow-up patients after breast cancer and in patients with a suspicious breast finding. The detection of suspicious axillary lymph nodes is usually a contraindication for the performance of a sentinel lymph node biopsy in patients with breast cancer. In such cases, a conventional axillary dissection is indicated. Requirements. The ACR has defined technical standards for the diagnostic and performance monitoring of imaging equipment in its ACR Practice Guidelines and Technical Standards (http://www.acr.org/SecondaryMainMenuCategories/quality_safety/guidelines/toc.aspx). Quality Assurance Guidelines: Minimal Technical Device Specifications – internal structures of the breast, including vascular and ductal structures – solid and cystic structures The enormous technical advances made in the last years have recently been factored in the required device specifications described above. Transducers are available with higher frequencies and good penetration depths. Besides the frequency, signal processing is also an important factor in determining image quality. A special focusing technique employed by modern US equipment, for example, makes images with exceptionally high quality possible. The German Society for Ultrasound in Medicine (DEGUM) has taken great effort in developing a state-of-the-art statement on technical device specifications and in improving US training guidelines. One of its workgroups has compiled the following list of criteria to promote better technical quality assurance, taking the advances of modern US equipment into account (Table 4.1). International guidelines. The 4th edition of the European Guidelines for Quality Assurance in Breast Cancer Screening and Diagnosis includes for the first time a chapter pertaining to multidisciplinary aspects of quality assurance in breast diagnostics. Relating to ultrasonography of the breast, it requires that the examiner be highly experienced and especially trained in breast US, and that the transducer frequency be at least 7.5 MHz, but optimally at 10 MHz or higher. The International Breast Ultrasound School (IBUS: http://www.ibus.org) and the American College of Radiology (ACR: http://www.acr.org) have also issued up-to-date international guidelines.
Breast Ultrasound
Significance of Breast Ultrasound
Indications
Technique and Methodology
Quality Assurance Guidelines
 Operating mode requirement: B-mode
Operating mode requirement: B-mode
 Scan format: linear array
Scan format: linear array
 Transducer frequency: ≥ 7.0 MHz
Transducer frequency: ≥ 7.0 MHz
 Transmit focal setting: electronically variable focal zone for optimal lateral resolution
Transmit focal setting: electronically variable focal zone for optimal lateral resolution
 Transceiver aperture: variable with chosen focal zone
Transceiver aperture: variable with chosen focal zone
 Reception amplification: variable time gain compensation (TGC)
Reception amplification: variable time gain compensation (TGC)
 Dynamic range: at least 60 dB
Dynamic range: at least 60 dB
 Field of view: width ≥ 3–8 cm, penetration depth ≥ 6cm
Field of view: width ≥ 3–8 cm, penetration depth ≥ 6cm
 Echo acquisition: ≥ 15 images/second
Echo acquisition: ≥ 15 images/second
 Image documentation: image documentation on a digital or analogous medium in accordance with archiving requirements. The following data must be included: B-mode image with distance scale, measured values, measuring marks, transducer frequency or frequency range, focal zone position, patient identification, date of examination, transducer designation, and study center. The inclusion of a pictograph showing transducer position and orientation is recommended.
Image documentation: image documentation on a digital or analogous medium in accordance with archiving requirements. The following data must be included: B-mode image with distance scale, measured values, measuring marks, transducer frequency or frequency range, focal zone position, patient identification, date of examination, transducer designation, and study center. The inclusion of a pictograph showing transducer position and orientation is recommended.
 Bit depth: ≥ 8 bit
Bit depth: ≥ 8 bit
 Technical image quality (organ/body area): imaging of the breast
Technical image quality (organ/body area): imaging of the breast
 Technical image quality (characteristic image features): differentiation between
Technical image quality (characteristic image features): differentiation between
Image quality in the clinical situation |
128 gray levels per pixel |
Good differentiation of breast tissue components |
Depiction of structural irregularities in breast tissue |
Depiction of tumor border irregularities |
Distinct depiction of cysts ≥4mm (elevated standard ≥2mm) |
Distinct depiction of tumors ≥10mm (elevated standard ≥5mm) |
Penetration depth of at least 4cm with good spatial resolution |
Depiction of a 20-gauge needle in breast parenchyma along the image plane |
Technical requirements |
Documentation: digital or hardcopy (multiformat film, video printer, Polaroid) |
Transducer frequency >5MHz or multifrequency transducer (must fulfill quality assurance standards on phantom tests) |
Scan rate >12 images/second |
Field of view >3.8cm |
Incorporated acoustic stand-off if near field resolution is not sufficient |
Monitor display: patient I. D., date, transducer, caliper, body marker (or indication of localization, e. g., as text), capacity, time gain compensation (TGC), preset, depth scale |
Safety standards meeting US safety regulations |
Free-hand biopsy or using a biopsy guide with virtual monitor visualization of needle pathway (5-mm lesion must be accessible at every depth) |
* As per the German Society for Ultrasound in Medicine (DEGUM)
Terminology and Diagnostic Criteria in Breast Ultrasound
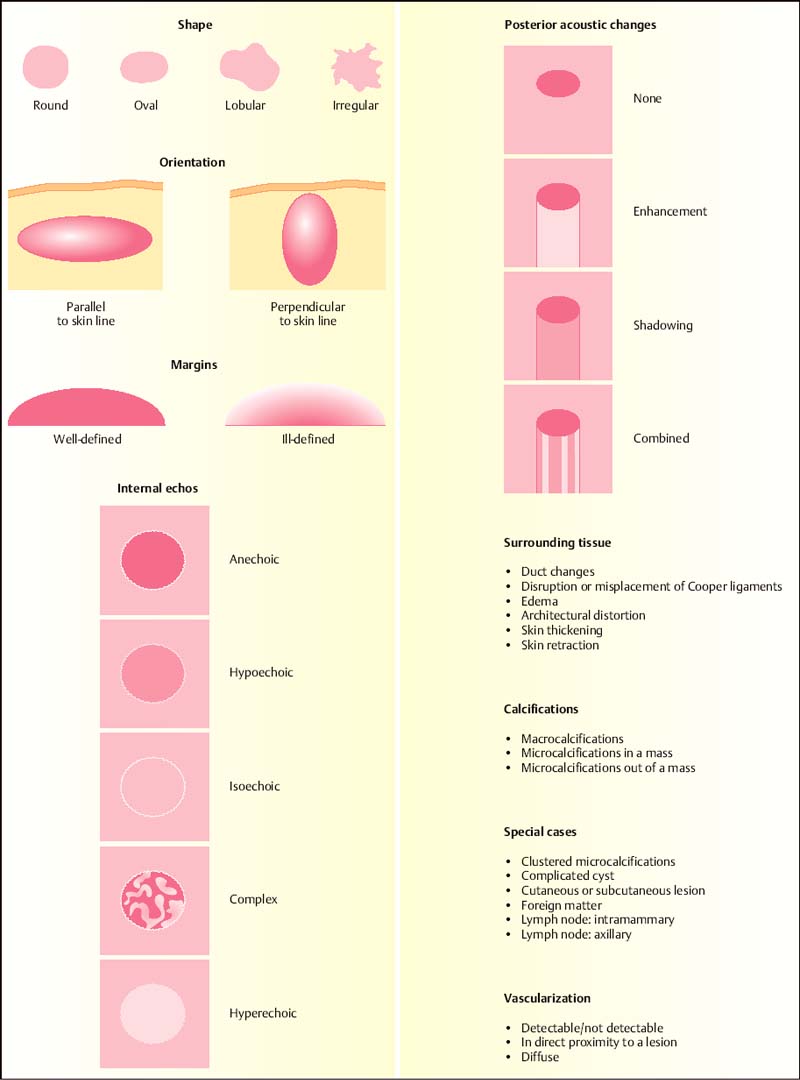
In analogy to the well-established ACR Breast Imaging Reporting and Data System (BI-RADS) categorization of mammographic findings, an ACR International Expert Working Group has developed a categorization system for US criteria of breast findings (BI-RADS-US). The resulting US lexicon has provided a consistent and universally understood terminology that serves as the basis for a standardized characterization of sonographic breast lesions, and thereby minimizes intra- and interobserver variability. The DEGUM’s Breast Ultrasonography Working Group has modified and expanded the ACR BI-RADS-US lexicon to reflect the group’s own experience (see Table 4.4).
DEGUM Ultrasound BI-RADS features. The following features are included in the BI-RADS-analogous DEGUM criteria for ultra-sonographic findings in the breast:
 Parenchymal density (parenchyma volume/total breast volume): classified into four density types (Table 4.2)
Parenchymal density (parenchyma volume/total breast volume): classified into four density types (Table 4.2)
 Structural composition of breast tissue: homogeneous, inhomogeneous (Table 4.3)
Structural composition of breast tissue: homogeneous, inhomogeneous (Table 4.3)
 Lesion description: shape, orientation, margin, lesion boundary, echo pattern, posterior acoustic features, calcifications, compressibility, mobility, surrounding tissue alterations (Table 4.4)
Lesion description: shape, orientation, margin, lesion boundary, echo pattern, posterior acoustic features, calcifications, compressibility, mobility, surrounding tissue alterations (Table 4.4)
Type I | Fibroglandular tissue < 25% | Fatty breast |
Type II | Fibroglandular tissue 25–50% | Partial involution |
Type III | Fibroglandular tissue 50–75% | Dense breast tissue |
Type IV | Fibroglandular tissue > 75% | Extremely dense breast tissue |
Category | Background echotexture | Sensitivity |
1 | Homogeneous, equivalent to parenchyma | Very good |
2 | Homogeneous, mixed fat/parenchyma equivalent | Good |
3 | Homogeneous, fat equivalent | Limited |
4 | Inhomogeneous | Very limited |
* Modified categorization of breast US sensitivity according to echogenicity patterns.
Criteria | Low level of suspicion | Higher level of suspicion |
Shape | Round, macrolobulated | Irregular |
Orientation | Parallel to the skin | Perpendicular to the skin |
Margin | Circumscribed | Indistinct, angular, microlobulated, spiculated |
Lesion boundary | Abrupt interface | Echogenic halo without sharp demarcation |
Echogenicity, echo pattern | Anechoic, hyperechoic | Hypoechoic (relative to fat) |
Internal structure | Homogeneous | Inhomogeneous |
Posterior acoustic features | Enhancement | Shadowing |
Posterior shadowing at borders | Bilateral |
|
Calcifications | Macrocalcifications |
|
Surrounding tissue alterations | Compression due to displacement | Architectural distortion, retraction |
Compressibility | Good | Little or none |
Mobility | Good | Little or none |
3D pattern | Compression pattern | Retraction pattern |
Vascularity | None | Present in or immediately adjacent to lesion |
Lymph nodes | Possessing high central echogenicity (hilus) | Hypoechoic, sometimes indistinct or angulated margins |
Ductal pattern | Regular | Solid internal structures, abrupt caliber changes or stoppage |
Tips and Tricks
Similar to the succinct description of the overall breast composition in the mammography report, the breast US report should also include a statement indicating the relative possibility that a lesion could be missed due to breast composition. It is important to communicate this information to the primary clinician, alerting him or her to the fact that the sensitivity of the examination in detecting small cancers is limited in certain women. With this goal in mind, it seems of little value to use the categories described in Table 4.2, which classify a breast according to the relative volume of parenchyma. Instead, the degree of homogeneity or heterogeneity of breast tissue has a greater influence on the sensitivity and specificity of the breast US examination. This information should be included in the examination report (Table 4.3).
The standard feature descriptors used to characterize US findings are listed in Table 4.4 and illustrated in Fig. 4.1.
In addition to the ACR BI-RADS-US features, the DEGUM has introduced the criteria compressibility, mobility, and 3D pattern, as well as a description of ductal structures and lymph nodes. The vascular criteria were expanded to include a quantification of vascular structures and a description of the vascular pattern.
Fig. 4.1 Schematic illustration of sonographic lesion criteria.
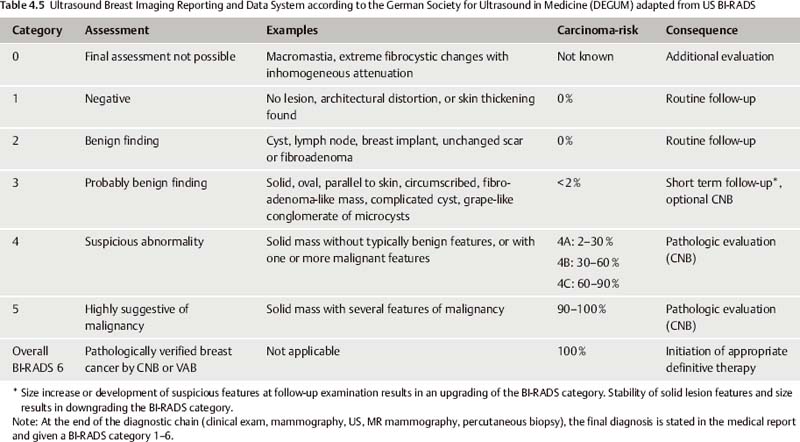
When assigning a US-BI-RADS category to an US lesion, previous US examinations should be taken into account and, if relevant, indicated in the report (Table 4.5).
Ultrasound-guided Percutaneous Core Needle Biopsy
Indications
Percutaneous biopsy of the breast is performed to provide a definitive diagnosis of ambiguous imaging findings, and to verify a breast cancer diagnosis before treatment (e. g., surgery, neoadjuvant chemotherapy). If a suspicious breast lesion is found in the primary US examination, or if a correlating lesion is identified in the “second-look” US examination after having been primarily detected on mammography or MR mammography, then the percutaneous biopsy should be performed under US-guidance. As this method requires no additional complex equipment or patient preparation, it is the most simple, rapid, and cost-efficient method for harvesting representative tissue, and is preferred over the other alternative techniques. As a real-time examination, an US-guided biopsy can be directed exactly and followed on the monitor. Targeted tissue sampling is thus possible in the majority of cases, independent of lesion location. The high rate of representative tissue acquisition from US-guided biopsies has been proven in many studies.
Axilla. Performing a CNB in the axillary region is associated with a higher complication rate due to the topographic proximity to large vascular and neural structures. For this reason, it is often preferable to perform a fine-needle aspiration biopsy (FNAB) of suspicious axillary lymph nodes. Larger lesions, however, may be core biopsied without great risk. In some cases, it is advisable to adjust the throw to the shorter setting.
Objective
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree