Indications: When history and physical exam do not provide a clear answer to the volume status of the patient. Especially useful in undifferentiated shock or to assess response to therapy.
This exam is usually combined with a cardiac and lung assessment, making it most convenient to use the sector/cardiac probe; however, a curved-array probe is equally effective. For assessment of the IJ, a linear probe is preferable.
Acquire both transverse and longitudinal views.
More details, including common acquisition pitfalls are in Chapter 8.
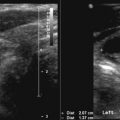
M-mode of the IVC can be useful to allow for quantitative measurements of diameter change over the respiratory cycle.
First, make a visual assessment of the collapse of the vessel.
Place the M-mode sampling line through an appropriate location in the vessel.
In the transverse plane, assess the side-to-side motion of the vessel throughout the respiratory cycle, as a pronounced side-to-side motion is likely to undermine accurate M-mode measurements in the longitudinal plane.

Set the sweep speed (x-axis) of the M-mode to a low speed to assess more than one respiratory cycle.
In the transverse view, identify the hepatic veins and visualize immediately inferior to that plane.
The cylinder tangent effect: if a longitudinal ultrasound imaging plane is not precisely in the center of the vessel, it will appear smaller than its true size. This can occur if the vessel moves from side to side during the respiratory cycle.
Assess at the midclavicular line in the anterior lung zones bilaterally for the presence of B-lines and lung sliding (see Chapter 6 for details).
Assess at the lung bases bilaterally for the presence of pleural effusions.
Useful in a situation where JVD would be helpful, but physical habitus or facial hair prevents an evaluation, or when it is impossible to obtain adequate IVC views. In our practice, it has mostly been replaced by IVC imaging.
Sit patient upright, or correct measurement for the angle of patient incline.
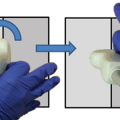
With a very light touch, visualize the IJ in the longitudinal plane. This is often done by starting in the transverse plane, centering the IJ on the screen, and rotating the probe so the indicator is cranial.
The goal is to acquire a clip in which the IJ narrows with a “paintbrush” or “German wine bottle” appearance. The height at which the vessel is collapsed has been shown to correlate tightly with jugular venous distention (JVD).
Excessive hand pressure or misalignment can cause result in the artifactual appearance of a smaller or more collapsed IJ, as with longitudinal scanning of the IVC, as noted above.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree