Key Points
- ▪
Extracranial carotid artery assessment is one of the most elegant applications of vascular ultrasound.
- ▪
With careful technique and adherence to a comprehensive Duplex protocol, ultrasound assessment of the carotid arteries is accurate.
- ▪
Knowledge of the potential extent of disease and how it may complicate ultrasound assessment of carotid artery disease, as well as the intrinsic limitations of the modality, are critical.
Carotid Artery and Variant Anatomy
Anatomic variants of the aortic arch occur in about one third of cases. The innominate artery branch of the aorta gives rise first to the right common carotid artery (CCA) and subsequently the right vertebral artery, beyond which it becomes the subclavian artery. On the distal aortic arch, the left CCA and further distally the left subclavian artery normally arise from the aortic arch with independent ostia. Anomalously, they may arise from a common ostium, and rarely they may arise from a common brachiocephalic artery. The left vertebral artery normally arises from the left subclavian artery.
Normally, the CCAs, which have no branches, divide into the internal and external carotid artery at approximately the level of the upper border of the thyroid cartilage. The main branches of the external carotid artery (ECA), in order of ascension, include the superior thyroid artery, ascending pharyngeal artery, lingual artery, occipital artery, facial artery, posterior auricular artery, maxillary artery, transverse facial artery, and superficial temporal artery.
The first three ECA branch vessels (superior thyroid artery, ascending pharyngeal artery, and lingual artery) are often seen on duplex scanning, and they are visualized more frequently in the presence of an ICA occlusion because they commonly enlarge to become important collateral vessels interconnecting the vertebral artery and ICA via the ophthalmic artery. The facial and superficial temporal arteries are the principal vessels that supply collateral flow around an occlusion of the ICA. The facial artery runs along the lateral border of the mandible and along the cheek to eventually join the ophthalmic artery via the nasal artery. The superficial temporal artery, which runs in front of the tragus of the ear, divides into two vessels, runs across the forehead, and communicates with branches of the terminal ophthalmic artery.
Because the ECA and ICA may be anatomically indistinguishable on grayscale scanning and their flow patterns may be rendered similar by disease, the superficial temporal artery branch of the ECA is sometimes used to attempt to distinguish the ECA from the ICA. The temporal tap technique, which is widely used, has the sonographer simultaneously recoding the spectral flow pattern of the ECA while tapping the superficial temporal artery and observing for waveform artifacts of the same frequency of the tapping. These artifacts are most easily recognized in the diastolic component of flow. However, this technique may fail to depict artifacts of sufficient clarity to avoid confusion of the ECA and ICA. Thus, the temporal tap technique is not adequately reliable to distinguish the ECA from the ICA (see Common Technical Problems).
The ICA has no branches along its extracranial portion and is arbitrarily divided into four segments. The extracranial/cervical segment runs between the carotid bifurcation and the carotid canal, where it becomes the petrous segment. From here, the artery passes through the petrous bone to the cavernous sinus, where it becomes the cavernous segment. After penetration through the dura, it becomes the supraclinoid segment and extends to the bifurcation into the anterior and middle cerebral arteries. There are three branches of the supraclinoid segment (ophthalmic artery, posterior communicating artery, and anterior choroidal artery). In some case, the ophthalmic artery may provide an important collateral of distal (to the ophthalmic artery) occlusion of the ICA.
The vertebral artery extends from the subclavian artery on the left and from the innominate on the right, through the atlanto-occipital membrane and dura mater to join the contralateral vertebral artery and become the basilar artery. There are numerous branches throughout its course.
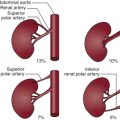
Common anatomic variants include (1) adjoining or common origin of the innominate artery and the left CCA (16%) ; (2) left CCA originating from the innominate artery (13%); (3) left vertebral artery arising from the aortic arch between the left CCA and left subclavian artery (6%); (4) unilateral or bilateral congenital absence of the CCA, which is very rare, with only 25 recorded cases (when the right CCA is absent, the ICA arises from the subclavian artery and the ECA from the innominate artery; when the left CCA is absent, both the ICA and ECA arise from the aortic arch) ; and (5) absence of the ICA, which is also very rare, supposedly occurring in less than 0.01% of the population. Collateral flow in this case may occur from the circle of Willis, persistent embryonic branches, or through transcranial vessels interconnected to branches of the ECA ( Fig. 2-1 ).

Carotid Artery Disease
Carotid artery disease accounts for approximately 25% of all cases of stroke and is the second largest cause of ischemic stroke ( Fig. 2-2 ). Despite the landmark gains in stroke reduction (>40%) in the past four decades, the total number of strokes per year is increasing due to the aging of the population.

The detection of carotid stenosis by physical diagnosis is relatively poor. Occlusions, lesser severity disease, and inexperience give false-negative results in the detection of carotid disease. Venous hums, ECA stenoses, and tortuosity and “kinking” of the ICA, as well as transmitted aortic stenosis murmurs, give false-positive results in the detection of ICA stenosis. Physical diagnosis sensitivities of 36% to 79% and specificities of 61% to 98% have been reported, establishing the need for more accurate imaging assessment. Duplex ultrasound is the usual screening test, although its yield and benefit is significantly determined by the clinical context in which carotid disease is being sought.
Pathology and Pathogenesis
It is recognized that carotid artery disease that results in stroke does so by embolization of atherothrombosis into the intracranial circulation or retina. Occlusion of a carotid artery by itself does not result in stroke if the circle of Willis is complete and has adequate inflow. A complete carotid occlusion may result in propagating distal thrombosis that may yield emboli and result in stroke, although the lesion may also be stable and clinically bland.
The usual location of an atherosclerotic carotid lesion is in the proximal ICA, typically arising off the posterior wall. However, considerable variability of plaque location and length does occur. Stenosis and occlusion of the larger CCA may also occur, as may disease of the intracranial portion of the ICA. ICA stenosis may extend a variable distance up the extracranial carotid artery. In addition to describing the severity of carotid stenosis, detailed description of the morphology of carotid stenosis is important, because successful endarterectomy requires that the entire plaque can be removed. If significant plaque extends further than can be accessed surgically, a shelf is left facing the bloodstream, which may result in dissection.
Treatment
The medical treatment of carotid disease, particularly of symptomatic carotid disease, confers limited benefit ( Table 2-1 and Table A-2 ). Medical treatment provides 15% to 20% relative risk reduction of stroke in a secondary prophylaxis with the use of acetylsalicylic acid (50 to 650 mg) or acetylsalicylic acid (50 mg) and dipyridamole (400 mg). It provides little or no proven benefit for primary prevention with acetylsalicylic acid (325 mg/day). Recommendations for antithrombotic therapy in patients with extracranial carotid atherosclerotic disease not undergoing revascularization are given in Box 2-1 , and guidelines for level of evidence are given in Table A-1 (appendix tables begin on page 277).
| STUDy | SAMPLE SIZE ( n ) | TREATMENT | OUTCOME | RISK REDUCTION |
|---|---|---|---|---|
| Meta-analysis | 73,247 | Antiplatelet therapy | Stroke, death, nonfatal stroke | 27% 25% from ASA |
| Meta-analysis | ASA | Stroke | –16% | |
| CATS, Hass trial | Ticlopidine | Stroke | –23% | |
| CAPRIE | ASA/ticlopidine vs. no treatment | Stroke, MI, vascular death | –9% | |
| ESPS-1 | ASA/dipyridamole | Stroke | –33% | |
| ESPS-2 | 6,602 | ASA/dipyridamole | Stroke | –21% |
| PRoFESS | 20,332 | Dipyridamole vs. clopidogrel | Stroke, MI, death from vascular causes | — |
Class I
- 1.
Antiplatelet therapy with aspirin, 75 to 325 mg daily, is recommended for patients with obstructive or nonobstructive atherosclerosis that involves the extracranial carotid and/or vertebral arteries for prevention of MI and other ischemic cardiovascular events, although the benefit has not been established for prevention of stroke in asymptomatic patients. ( Level of Evidence: A )
- 2.
In patients with obstructive or nonobstructive extracranial carotid or vertebral atherosclerosis who have sustained ischemic stroke or TIA, antiplatelet therapy with aspirin alone (75 to 325 mg daily), clopidogrel alone (75 mg daily), or the combination of aspirin plus extended-release dipyridamole (25 and 200 mg twice daily, respectively) is recommended ( Level of Evidence: B ) and preferred over the combination of aspirin with clopidogrel. ( Level of Evidence: B ). Selection of an antiplatelet regimen should be individualized on the basis of patient risk factor profiles, cost, tolerance, and other clinical characteristics, as well as guidance from regulatory agencies.
- 3.
Antiplatelet agents are recommended rather than oral anticoagulation for patients with atherosclerosis of the extracranial carotid or vertebral arteries with ( Level of Evidence: B ) or without ( Level of Evidence: C ) ischemic symptoms. (For patients with allergy or other contraindications to aspirin, see Class IIa recommendation #2.)
Class IIa
- 1.
In patients with extracranial cerebrovascular atherosclerosis who have an indication for anticoagulation, such as atrial fibrillation or a mechanical prosthetic heart valve, it can be beneficial to administer a vitamin K antagonist (such as warfarin, dose-adjusted to achieve a target international normalized ratio [INR] of 2.5 [range 2.0 to 3.0]) for prevention of thromboembolic ischemic events. ( Level of Evidence: C )
- 2.
For patients with atherosclerosis of the extracranial carotid or vertebral arteries in whom aspirin is contraindicated by factors other than active bleeding, including allergy, either clopidogrel (75 mg daily) or ticlopidine (250 mg twice daily) is a reasonable alternative. ( Level of Evidence: C )
Class III: No Benefit
- 1.
Full-intensity parenteral anticoagulation with unfractionated heparin or low-molecular-weight heparinoids is not recommended for patients with extracranial cerebrovascular atherosclerosis who develop transient cerebral ischemia or acute ischemic stroke. ( Level of Evidence: B )
- 2.
Administration of clopidogrel in combination with aspirin is not recommended within 3 months after stroke or TIA. ( Level of Evidence: B )
Although the potential revascularization benefit for carotid artery disease is prominent, several factors contribute to achieving, or not achieving, a net benefit, and all have to be carefully considered: (1) symptom status; (2) stenosis severity; (3) patient’s comorbidities, operative stroke, and cardiac risk; and (4) the surgeon’s operative morbidity and mortality rate.
The understanding of the relative merits of surgical endarterectomy and carotid stenting is evolving. By limited trials, they appear similar in overall benefit, with some age influence ( Fig. 2-3 ), and with more myocardial infarction associated with surgical endarterectomy and more stroke associated with stenting.

The optimal combination of nondisabling symptoms, severe stenosis but no occlusion, low comorbidity/patient risk, and low surgeon morbidity/mortality yields an impressive 70% to 85% relative risk reduction of subsequent stroke and mortality from carotid endarterectomy (CEA). Following CEA performed in optimal circumstances, survival free of ipsilateral stroke is excellent; it is 97% at 2 years, 93% at 5 years, and 92% at 10 years. Surgical endarterectomy of in cases of greater than 60% stenosis of asymptomatic patients, although validated, remains controversial. The lower (10%) relative risk reduction of endarterectomy for asymptomatic disease renders the outcome critically dependent on patient risk and surgeon risk. Optimally, the stroke and mortality risk for CEA should be less than 6% for symptomatic individuals and less than 3% for asymptomatic individuals. For every 2% complication rate greater than 6% to 7%, the 5-year benefit of CEA falls by 20%. If the complication rate exceeds 6% to 7%, then only severe and symptomatic lesions may have net benefit from CEA ( Fig. 2-4 ).

Results of the comparative utility of CEA and modes of therapy are presented in Table A-3 .
Results of trials comparing CEA and carotid artery stenting are presented in Table A-4 , Table A-5 , Table A-6 .
A summary of ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline recommendations regarding the selection of revascularization techniques for patients with carotid artery stenosis is given in Table A-7 .
Recommendations for diagnostic testing in patients with symptoms or signs of extracranial carotid artery disease are given in Box 2-2 .
Class I
- 1.
The initial evaluation of patients with transient retinal or hemispheric neurological symptoms of possible ischemic origin should include noninvasive imaging for the detection of ECVD. ( Level of Evidence: C )
- 2.
Duplex ultrasonography is recommended to detect carotid stenosis in patients who develop focal neurological symptoms corresponding to the territory supplied by the left or right internal carotid artery. ( Level of Evidence: C )
- 3.
In patients with acute, focal ischemic neurological symptoms corresponding to the territory supplied by the left or right internal carotid artery, magnetic resonance angiography (MRA) or computed tomography angiography (CTA) is indicated to detect carotid stenosis when sonography either cannot be obtained or yields equivocal or otherwise nondiagnostic results. ( Level of Evidence: C )
- 4.
When extracranial or intracranial cerebrovascular disease is not severe enough to account for neurological symptoms of suspected ischemic origin, echocardiography should be performed to search for a source of cardiogenic embolism. ( Level of Evidence: C )
- 5.
Correlation of findings obtained by several carotid imaging modalities should be part of a program of quality assurance in each laboratory that performs such diagnostic testing. ( Level of Evidence: C )
Class IIa
- 1.
When an extracranial source of ischemia is not identified in patients with transient retinal or hemispheric neurological symptoms of suspected ischemic origin, CTA, MRA, or selective cerebral angiography can be useful to search for intracranial vascular disease. ( Level of Evidence: C )
- 2.
When the results of initial noninvasive imaging are inconclusive, additional examination by use of another imaging method is reasonable. In candidates for revascularization, MRA or CTA can be useful when results of carotid duplex ultrasonography are equivocal or indeterminate. ( Level of Evidence: C )
- 3.
When intervention for significant carotid stenosis detected by carotid duplex ultrasonography is planned, MRA, CTA, or catheter-based contrast angiography can be useful to evaluate the severity of stenosis and to identify intrathoracic or intracranial vascular lesions that are not adequately assessed by duplex ultrasonography. ( Level of Evidence: C )
- 4.
When noninvasive imaging is inconclusive or not feasible because of technical limitations or contraindications in patients with transient retinal or hemispheric neurological symptoms of suspected ischemic origin, or when noninvasive imaging studies yield discordant results, it is reasonable to perform catheter-based contrast angiography to detect and characterize extracranial and/or intracranial cerebrovascular disease. ( Level of Evidence: C )
- 5.
MRA without contrast is reasonable to assess the extent of disease in patients with symptomatic carotid atherosclerosis and renal insufficiency or extensive vascular calcification. ( Level of Evidence: C )
- 6.
It is reasonable to use MRI systems capable of consistently generating high-quality images while avoiding low-field systems that do not yield diagnostically accurate results. ( Level of Evidence: C )
- 7.
CTA is reasonable for evaluation of patients with clinically suspected significant carotid atherosclerosis who are not suitable candidates for MRA because of claustrophobia, implanted pacemakers, or other incompatible devices. ( Level of Evidence: C )
Class IIb
- 1.
Duplex carotid ultrasonography might be considered for patients with nonspecific neurological symptoms when cerebral ischemia is a plausible cause. ( Level of Evidence: C )
- 2.
When complete carotid arterial occlusion is suggested by duplex ultrasonography, MRA, or CTA in patients with retinal or hemispheric neurological symptoms of suspected ischemic origin, catheter-based contrast angiography may be considered to determine whether the arterial lumen is sufficiently patent to permit carotid revascularization. ( Level of Evidence: C )
- 3.
Catheter-based angiography may be reasonable in patients with renal dysfunction to limit the amount of radiographic contrast material required for definitive imaging for evaluation of a single vascular territory. ( Level of Evidence: C )
Recommendations for carotid artery evaluation and revascularization before cardiac surgery are given in Box 2-3 .
Class IIa
- 1.
Carotid duplex ultrasound screening is reasonable before elective CABG surgery in patients older than 65 years of age and in those with left main coronary stenosis, PAD, a history of cigarette smoking, a history of stroke or TIA, or carotid bruit. ( Level of Evidence: C )
- 2.
Carotid revascularization by CEA or CAS with embolic protection before or concurrent with myocardial revascularization surgery is reasonable in patients with greater than 80% carotid stenosis who have experienced ipsilateral retinal or hemispheric cerebral ischemic symptoms within 6 months. ( Level of Evidence: C )
Class IIb
- 1.
In patients with asymptomatic carotid stenosis, even if severe, the safety and efficacy of carotid revascularization before or concurrent with myocardial revascularization are not well established. ( Level of Evidence: C )
Recommendations for selection of patients for carotid revascularization are given in Box 2-4 .
Class I
- 1.
Patients at average or low surgical risk who experience nondisabling ischemic stroke or transient cerebral ischemic symptoms, including hemispheric events or amaurosis fugax, within 6 months (symptomatic patients) should undergo CEA if the diameter of the lumen of the ipsilateral internal carotid artery is reduced more than 70% as documented by noninvasive imaging (20,83) ( Level of Evidence: A ) or more than 50% as documented by catheter angiography ( Level of Evidence: B ) and the anticipated rate of perioperative stroke or mortality is less than 6%.
- 2.
CAS is indicated as an alternative to CEA for symptomatic patients at average or low risk of complications associated with endovascular intervention when the diameter of the lumen of the internal carotid artery is reduced by more than 70% as documented by noninvasive imaging or more than 50% as documented by catheter angiography and the anticipated rate of periprocedural stroke or mortality is less than 6%. ( Level of Evidence: B )
- 3.
Selection of asymptomatic patients for carotid revascularization should be guided by an assessment of comorbid conditions, life expectancy, and other individual factors and should include a thorough discussion of the risks and benefits of the procedure with an understanding of patient preferences. ( Level of Evidence: C )
Class IIa
- 1.
It is reasonable to perform CEA in asymptomatic patients who have more than 70% stenosis of the internal carotid artery if the risk of perioperative stroke, MI, and death is low. ( Level of Evidence: A )
It is reasonable to choose CEA over CAS when revascularization is indicated in older patients, particularly when arterial pathoanatomy is unfavorable for endovascular intervention. ( Level of Evidence: B )
- 3.
It is reasonable to choose CAS over CEA when revascularization is indicated in patients with neck anatomy unfavorable for arterial surgery. ( Level of Evidence: B )
- 4.
When revascularization is indicated for patients with TIA or stroke and there are no contraindications to early revascularization, intervention within 2 weeks of the index event is reasonable rather than delaying surgery. ( Level of Evidence: B )
Class IIb
- 1.
Prophylactic CAS might be considered in highly selected patients with asymptomatic carotid stenosis (minimum 60% by angiography, 70% by validated Doppler ultrasound), but its effectiveness compared with medical therapy alone in this situation is not well established. ( Level of Evidence: B )
- 2.
In symptomatic or asymptomatic patients at high risk of complications for carotid revascularization by either CEA or CAS because of comorbidities, the effectiveness of revascularization versus medical therapy alone is not well established. ( Level of Evidence: B )
Class III: No Benefit
- 1.
Except in extraordinary circumstances, carotid revascularization by either CEA or CAS is not recommended when atherosclerosis narrows the lumen by less than 50%. ( Level of Evidence: A )
- 2.
Carotid revascularization is not recommended for patients with chronic total occlusion of the targeted carotid artery. ( Level of Evidence: C )
- 3.
Carotid revascularization is not recommended for patients with severe disability caused by cerebral infarction that precludes preservation of useful function. ( Level of Evidence: C )
Scanning Protocol
Both carotid arteries, as well as the subclavian, vertebral, and brachiocephalic arteries, are scanned. Flow findings in one carotid artery may be influenced by lesions in the contralateral artery; flow patterns (and direction) in the vertebral arteries may be influenced by subclavian artery lesions ( Figs. 2-5 to 2-9 ). The
- ▪
Using a curved linear probe for the scanning of the most distal and deep extracranial portion of the internal carotid artery (ICA) not only will achieve better acoustic penetration but will also give (because of its wider field of view) the “big picture” more clearly than a linear probe, especially when the vessel is tortuous.
- ▪
Beware of the possibility that the external carotid artery (ECA), depending on the configuration and ostial position of the branches, can and often does have a less resistive waveform shape than the classic pattern. Those branches might not always be in evidence, if imaging is suboptimal. This can sometimes cloud distinction between the ECA and the ICA. (This also applies to the proximal profunda femoris artery.)
- ▪
The most comfortable scanning position is from above the head of the patient’s bed, using the right hand for the right carotid, and the left hand for the left carotid, supporting the scanning hand as described in Chapter 1 by using the elbow and part of the scanning hand as support.
- ▪
When using different angles of approach around the circumference of the neck, it may be necessary to angle steeply to insonate the carotids (e.g., if scanning from a posterior direction angle anteriorly and vice versa).
- ▪
With a variation in the angle of approach, the ICA and ECA will change position with respect to one another (e.g., if the ECA was anterior to the ICA with an anterior/mid approach, it will be posterior to the ICA with a posterior approach).
- ▪
In the presence of eccentric calcified plaque, first analyzing the artery in short axis to determine the best angle of approach, around the plaque, and then seeking those clear windows in long axis, will provide better color filling and better defined spectral Doppler envelope.
- ▪
To facilitate visualization of the vertebral artery, first find the common carotid artery (CCA) in long axis and then either slide the transducer laterally without changing its angle or angle laterally without shifting to left or right and look for segments of the artery lying between the vertebral processes.
- ▪
Be aware that as the ICA extends distally in the neck, the caliber will decrease and in a normal vessel flow velocity will consequently rise slightly.
- ▪
In addition, in performing spectral Doppler sampling in the distal extracranial ICA, there will be a greater sample volume-to-vessel size ratio, possibly resulting in apparent flow turbulence because a greater cross-section of flow speeds will be included.





| ANATOMIC SEGMENT | TECHNIQUE | DUPLEX MODALITY |
|---|---|---|
| Common carotid | SAX sweep | Grayscale |
| Color Doppler | ||
| LAX sweep | Grayscale | |
| Color Doppler | ||
| LAX | ||
| Proximal | Grayscale | |
| Color Doppler | ||
| Pulsed-wave spectral | ||
| Mid | Grayscale | |
| Color Doppler | ||
| Pulsed-wave spectral | ||
| Distal | Grayscale | |
| Color Doppler | ||
| Pulsed-wave spectral | ||
| Internal carotid | LAX | |
| Proximal | Grayscale | |
| Color Doppler | ||
| Pulsed-wave spectral | ||
| Mid | Grayscale | |
| Color Doppler | ||
| Pulsed-wave spectral | ||
| Distal | Grayscale | |
| Color Doppler | ||
| Pulsed-wave spectral | ||
| External carotid | LAX | Grayscale |
| Color Doppler | ||
| Pulsed-wave spectral | ||
| Brachiocephalic | LAX | Grayscale |
| Color Doppler | ||
| Pulsed-wave spectral | ||
| Subclavian | LAX | Grayscale |
| Color Doppler | ||
| Pulsed-wave spectral | ||
| Vertebral | LAX | |
| Ostial | Color Doppler | |
| Pulsed-wave spectral | ||
| Mid | Color Doppler | |
| Pulsed-wave spectral | ||
| Brachial blood pressure recording | ||
Scanning of the Common Carotid Artery
The CCA is scanned as it may harbor significant pathology (e.g., stenosis, dissection), and its flow velocity is used to establish a reference to the ICA flow velocity (peak systolic velocity [PSV] ICA/CCA). Usual (velocity) criteria for ICA stenosis assessment assume nondisturbed prestenotic flow (no CCA stenosis jet contamination of ICA flow characteristics). A significant CCA stenosis is evident as a greater than 50% narrowing seen on grayscale imaging and a 50% or 100% focal increase in the PSV of the CCA. Advanced congestive heart failure lowers the PSV of the CCA, and it also lowers the PSV of the ICA. Aortic stenosis jets commonly radiate into the CCA, where they are often auscultated. High-grade obstruction of the ICA may increase the pulsatility of the CCA (due to pulse wave reflection) and render the CCA flow profile high resistance, with diminished diastolic velocity or postsystolic flow reversal.
Recommendations for duplex ultrasonography to evaluate asymptomatic patients with known or suspected carotid stenosis are given in Box 2-5 .
Class I
- 1.
In asymptomatic patients with known or suspected carotid stenosis, duplex ultrasonography, performed by a qualified technologist in a certified laboratory, is recommended as the initial diagnostic test to detect hemodynamically significant carotid stenosis. ( Level of Evidence: C )
Class IIa
- 1.
It is reasonable to perform duplex ultrasonography to detect hemodynamically significant carotid stenosis in asymptomatic patients with carotid bruit. ( Level of Evidence: C )
- 2.
It is reasonable to repeat duplex ultrasonography annually by a qualified technologist in a certified laboratory to assess the progression or regression of disease and response to therapeutic interventions in patients with atherosclerosis who have had stenosis greater than 50% detected previously. Once stability has been established over an extended period or the patient’s candidacy for further intervention has changed, longer intervals or termination of surveillance may be appropriate. ( Level of Evidence: C )
Class IIb
- 1.
Duplex ultrasonography to detect hemodynamically significant carotid stenosis may be considered in asymptomatic patients with symptomatic PAD, coronary artery disease (CAD), or atherosclerotic aortic aneurysm, but because such patients already have an indication for medical therapy to prevent ischemic symptoms, it is unclear whether establishing the additional diagnosis of ECVD in those without carotid bruit would justify actions that affect clinical outcomes. ( Level of Evidence: C )
- 2.
Duplex ultrasonography might be considered to detect carotid stenosis in asymptomatic patients without clinical evidence of atherosclerosis who have two or more of the following risk factors: hypertension, hyperlipidemia, tobacco smoking, a family history in a first-degree relative of atherosclerosis manifested before age 60 years, or a family history of ischemic stroke. However, it is unclear whether establishing a diagnosis of ECVD would justify actions that affect clinical outcomes. ( Level of Evidence: C )
Class III: No Benefit
- 1.
Carotid duplex ultrasonography is not recommended for routine screening of asymptomatic patients who have no clinical manifestations of or risk factors for atherosclerosis. ( Level of Evidence: C )
- 2.
Carotid duplex ultrasonography is not recommended for routine evaluation of patients with neurological or psychiatric disorders unrelated to focal cerebral ischemia, such as brain tumors, familial or degenerative cerebral or motor neuron disorders, infectious and inflammatory conditions affecting the brain, psychiatric disorders, or epilepsy. ( Level of Evidence: C )
- 3.
Routine serial imaging of the extracranial carotid arteries is not recommended for patients who have no risk factors for development of atherosclerotic carotid disease and no disease evident on initial vascular testing. ( Level of Evidence: C )
The CCA sweep is performed to overview the CCA anatomy from the ostium (right CCA: brachiocephalic; left CCA: aorta) to the bifurcation. The distribution and extent of intima-media thickness (IMT), plaque, or other pathology is noted. The CCA sweep is repeated with color Doppler flow mapping to associate anatomic and flow findings. The sweep is performed in both short-axis and long-axis orientations. The intention is to both localize and establish the severity of luminal narrowing by grayscale imaging to provide corroboration with Doppler findings. As well, long-axis grayscale imaging is recorded. In the proximal, middle, and distal CCAs, color Doppler and pulsed-wave recordings of flow are recorded. Stenosis may occur in any portion of the CCA, particularly the ostium—hence the need to assess for pathology at any level and to endeavor to characterize the grayscale and Doppler findings of the CCAs at all levels.
Scanning of the Brachiocephalic Artery
The brachiocephalic artery is scanned to assess for the presence of significant lesions (e.g., dissection, stenosis) within it. Brachiocephalic lesions influence the flow patterns within the right CCA; hence, interpretation of the right CCA velocity pattern can only be performed with knowledge of the inflow characteristics. In some patients, there are bilateral brachiocephalic arteries ( Fig. 2-10 ).

Scanning of the Internal Carotid Artery
The short-axis and long-axis scanning of the CCA gives a preview of the proximal ICA. As with the CCA, the ICA is scanned with grayscale, color Doppler, and pulsed-wave Doppler recording of its proximal, middle, and distal portions. Although the large majority of atherosclerotic stenoses involve the proximal ICA, some stenoses extend well up into the ICA and are more difficult to remove at endarterectomy. Some lesions, such as spontaneous dissection, are typically present above/beyond the proximal ICA, which is a region commonly difficult to image. The anatomy and its physiology of the ICA must be interrogated along its full extracranial course. More than 50% stenosis of the proximal ICA renders the flow turbulent in the middle and often in the distal ICA as well. Severe stenosis of the proximal ICA renders the distal ICA flow profile “parvus et tardus.” High-grade obstruction or occlusion in the distal ICA or intracranial ICA makes the flow pattern of the proximal/middle ICA high resistance. Proximal ICA stenosis severity is established on the basis of grayscale appearance, the PSV of the ICA, the end-diastolic velocity of the ICA, and the PSA of the CCA.
Grayscale imaging in long axis view is performed to localize and characterize plaque severity as less than 50%, greater than or equal to 50%, or occlusion. Optimized color Doppler flow mapping is useful to define the lumen, because hypoechoic plaque and restenosis material may by inapparent by regular grayscale imaging ( Fig. 2-11 ).