Key Points
- ▪
Maximizing and easing optimal image acquisition is achieved by:
- ▪
Integration of knowledge of anatomy, disease, machine factors, and scanning technique
- ▪
Effort and persistence
- ▪
Basic Guidelines
Optimizing Settings: Beyond Factory Presets
Although providing a useful starting point, factory settings and algorithms are designed for optimal scanning of patients of average body habitus, without consideration of precisely what is to be depicted or measured. Further optimization and enhancement of the image and color or spectral Doppler for a particular study/zone can be achieved by directed empiric manual adjustment of machine settings. Knowledge and confidence with machine settings provides incremental diagnostic yield and avoidance of many artifacts.
Knowledge of Anatomic Variants: As Important As Knowledge of Normal Anatomy
Arterial, and especially venous, anatomy is subject to a considerable range of variation. Failing to consider anatomic variation in the evaluation of a suspected disease may preclude its recognition. For example, normally, the superficial femoral vein lies posterior to the superficial femoral artery. However, in as many as 30% of cases, the superficial femoral vein/popliteal venous anatomy is that of a bifid, and occasionally trifid, variant. Thrombosis of such an anatomic variant system commonly involves only one of its limbs. If the thrombosed limb of a bifid system is situated posterior to the artery, then only the anterior venous limb is seen at first glance. Failure to search for the presence of a diseased posterior limb may miss the presence of thrombosis. Failure to search the entire field may lead to failure to detect thrombosis of an anomalous vein.
Flow Direction: Should Be Determined Rather Than Assumed
The direction of flow within a vessel should never be assumed. In several pathologies (those that involve upstream tight stenosis or occlusion with large downstream collaterals or complex recanalization), flow within an artery may be reversed in direction, which would therefore clearly establish the presence of significant pathology. Examples, such as subtotal or complete occlusion of the common carotid artery where collaterals from the external carotid artery reconstitute flow at the bifurcation to maintain patency of the internal carotid artery, abound.
Encountering Technical Difficulties
If part of a scan is technically difficult, try the following maneuvers: (1) change the patient/body part position, (2) change the scanning angle of approach, (3) change the transducer frequency, or (4) call in a colleague—sometimes a different hand or eye can help. If these do not yield improved image quality, proceed to scan another vessel or segment and return to the difficult section later.
Optimal Sonographer Positioning for Carotid Scanning
For all scanning, when possible, use the elbow of the scanning arm and part of the scanning hand (such as a finger) as a fulcrum to maximize manual stability and to minimize muscle and joint strain. Perform hand and arm stretches and exercises before scanning every day to minimize repetitive strain injury. Consider scanning with both left and right hands and learn to scan with the ultrasound machine at both the foot and the head of the patient. This is useful on the ward, where monitoring equipment is inevitably in the way.
Scanning with the Nondominant Hand
Scanning with the nondominant arm and hand is easier than it first appears and can be learned quickly (often within a week). Distribution of the repetitive strain of scanning between the upper extremities may help stave off wear-and-tear injuries to the upper extremities and spine. Developing some versatility of scanning with both hands is particularly useful when having to perform portable scans at the bedside, such as in the intensive care unit, where there is medical equipment around the bed, rendering it impossible for the sonographer to stand in the ideal/usual position for scanning. In such a case, lack of access to positioning oneself above the head of the patient for carotid scanning results in the need to scan facing the patient and use of the hands in the reverse position from usual. Use of a triangle-wedge sponge pad or towel to support the scanning limb may also avoid excess strain.
Optimal Patient Position for Scanning
Patient comfort during scanning is important, and the patients’ position should be such that they are comfortable throughout. Patients who are uncomfortable may: (1) adjust their body position to alleviate the discomfort and move during scanning, (2) often tense their limb muscles, and (3) be unable to undergo a complete scan. Neck stretches for carotid scanning are not necessary and may be counterproductive because they provoke discomfort in many patients. Similarly, leg abduction (to scan the popliteal fossa) in elderly or orthopedic patients with hip or other leg problems is often uncomfortable for patients and unnecessary because the distal superficial femoral and popliteal vessels can be scanned from the posterolateral side.
Internal Consistency of Testing
Retain an understanding of the “big picture”—how all the pieces may (or may not) fit together. If, for instance, a lower extremity study consists of both ankle-brachial index recordings and an arterial lower extremity duplex scan, and the results from the two components do not lead to the same conclusion, consider: (1) repeating one or part of one of the tests, (2) disease-based reasons that may explain the observations, and (3) the role of further testing.
Standardization of Laboratory Algorithms and Criteria
A standard diagnostic algorithm, per pathology, should be established and adhered to in the laboratory. Just as importantly, diagnostic criteria should be standardized. Standard, but adaptable, diagnostic algorithms and diagnostic criteria keep results consistent from one patient visit to the next, from one patient to another, and from one sonographer to another.
Clinical Context and Complementary Data
Review available notes and compile an appropriate medical history to establish and understand the clinical profile of the case. Whenever possible, seek the results of subsequent follow-up testing.
Scanning the Anatomic Length of the Vessel
To maximize the recognition of disease within an artery or vein, scan along the complete length of the vessel from its ostium to terminus when possible. Although the more proximal and distal aspects of vessels are regularly more difficult to image, they are particularly important to scan. For example, atherosclerosis occasionally occurs at the origin of the common carotid artery, as it may at the ostia of the vertebral and innominate arteries. Ostial lesions are often, but not necessarily, suggested by the detection of turbulent flow encountered further downstream in the more readily imaged portions of vessels, and there is no plausible explanation of the origin of the turbulence, other than downstream transmission from an upstream lesion. Ostial lesions that send elevated velocities downstream render assessment of more distal stenoses difficult, unless there has been recovery of flow velocity to normal levels before such downstream lesions.
Avoiding Singularization of Focus and Findings
Beware of focusing on one lesion to the exclusion of others that are present. This can readily occur, particularly when the scan is difficult. Common examples include (1) finding one endoleak but missing others, (2) finding an iatrogenically created pseudoaneurysm but missing an arteriovenous fistula, and (3) finding an extensive deep venous thrombosis but missing concomitant superficial venous thrombosis.
Localizing Lesions by Anatomic Reference Points
Using landmarks to localize the position is helpful when comparing findings with radiographic studies. For example, lesional position in the superficial femoral artery measured with respect to inguinal ligament/groin crease, with respect to the lower border of the patellar (knee joint), or of the internal carotid artery with respect to the angle of mandible may facilitate comparison with findings from angiographic, computed tomography, or magnetic resonance angiography studies. The referencing of lesions by superficial or deep anatomy facilitates intertest comparisons, such as preintervention and postintervention.
Avoiding Mistaken Identity: Differentiation of Collateral from Native Vessels
When interrogating peripheral arteries, beware of mistaking a stem vessel (the collateral or efferent artery that is the first part of the bypass system around a significant occlusion) for a stenosis. Typically, flow at the point where the stem vessel branches out exhibits a high velocity profile (because flow in the branch is being sampled off-axis with angle possibly unknown and flow velocity will be higher as compensation for the stenosis/occlusion downstream) and turbulent (because flow in the branch vessel is not being sampled necessarily in midstream, because most are small arteries).
Similarly, when scanning the superficial femoral artery, it is possible to mistake a straight segment of bridging collaterals as the anticipated/intended native vessel, particularly if the course of the collateral vessels is near to and parallel with the occluded vessel, facilitating “mistaken identity.” A midzone collateral network may be distinguished from a diseased, stringy, but patent native lumen by use of a lower frequency transducer that enables a wider field of view and often allows visualization of both collateral and patent native vessel segments in the same planes. Identification of the vein that accompanies the artery and knowledge of the vessels’ usual alignment may assist with distinguishing parallel collaterals from an occluded main artery, because a collateral vessel most likely runs quite separately from the vein.
Always try to follow a vessel from its origin to be certain of its source. This lessens potential confusion in the case of complex, and often very important, lesions. For example, in the presence of distal aortic occlusion, it is common for the inferior mesenteric to enlarge, supply collaterals around the blockage, and, as it invariably runs parallel, take on the appearance of a patent iliac artery.
Grayscale Imaging Issues
Grayscale Settings
To optimize grayscale images, in addition to gain controls, consider adjusting the following settings/parameters to enhance detail:
- 1.
Persistence. Optimization of persistence smoothes the appearance of the image and reduces speckle artifact.
- 2.
Harmonics. Optimization of harmonic frequency enhances the depiction of deep structures as well as improving grayscale contrast (although increasing the selected harmonic frequency reduces the frame rate and can be attempted, for example, when trying to image a poorly depicted distal internal carotid artery, before resorting to a deeper penetrating transducer.
- 3.
Tissue colorization (allows the eye to see detail that was not readily apparent in the plain grayscale image)
- 4.
Scanning initially without color Doppler flow mapping to pick up nuances in grayscale findings, because such fine detail may be washed over by color (as a general rule, only apply color Doppler flow mapping after the grayscale image has been optimized and acquired).
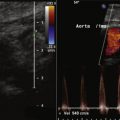
Grayscale imaging issues are illustrated in Figures 1-1 to 1-5 .





Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree