Key Points
- ▪
Knowledge of normal and variant anatomy of the lower extremity venous vasculature is critical.
- ▪
A standardized and comprehensive duplex examination protocol is critical.
- ▪
Knowledge of possible diseases/lesions potentially within the lower extremity venous vasculature, and how to maximize their recognition, is critical.
Venous Anatomy of the Lower Extremity
The venous system of the lower extremity consists of three components:
- 1.
Thick-walled superficial veins
- 2.
Thin-walled deep veins
- 3.
Perforating veins, which cross the fascia and drain blood from the superficial to the deep system
Approximately 85% of the venous return is accomplished by the deep venous system and 15% by the superficial system.
All of the vein components mentioned previously contain one-way bicuspid valves, preventing reflux, and they are embedded in an area referred to as a venous sinus, an enlargement of the vein wall that allows unimpeded movement of the valve. There are fewer valves in the superficial venous system compared with the deep venous system, where, for example, in the posterior and peroneal veins of the calf, there may be one valve per inch. In approximately 20% of people, there are no valves between the groin and the heart; in approximately 20% of people, there is one valve in the external iliac vein; and in 60% of people, there is one valve in the common femoral vein.
The Superficial Venous System
The main veins of the superficial system are the:
- □
Greater or long saphenous vein
- □
Lesser or short saphenous vein
The long saphenous vein, which contains up to 20 valves (mostly within the calf), runs from the medial marginal vein of the foot and along the medial aspect of the calf and thigh. This vein terminates in the common femoral vein at the level of the groin, at what is known as the saphenofemoral junction.
Large accessory saphenous veins, which run parallel with the main vein but anterior to the saphenous fascia (either anterior-laterally or posteriorly), are said to be present in 50% to 70% of people, and are thinner walled and considerably less muscular than the main vein. They can appear as duplicated veins, may enter the main vein at variable levels, and drain parts of the thigh and lower abdominal wall.
Several other superficial veins drain into the greater saphenous vein before it enters into the common femoral vein: the superficial external pudendal vein, the superficial circumflex iliac vein, and the superficial epigastric veins, which drain the parts of the hip, genital, and pubic areas.
The lesser or short saphenous vein is a continuation of the lateral marginal vein. This vein runs along the line that at one time was known as the “stocking” line, referring to the nylon stockings worn by women after World War II where the seam was supposed to run straight down the middle of the back of the leg. The terminus is variable; it could drain into the deep system anywhere from the popliteal to the distal superficial femoral vein and might also join the popliteal vein via the gastrocnemius vein.
The long saphenous vein is often duplicated in the thigh, but the short saphenous vein is less frequently duplicated in the calf.
The vein of Giacomini, named after the anatomist who first identified this vein in 1837, is another superficial vein, present in approximately 70% of limbs. It connects the proximal short saphenous and proximal long saphenous veins.
The Perforating Veins
Perforating veins are so-named because they pierce (traverse) the fascia. They are also referred to as “communicating veins” because they carry blood from one venous system to another. Some perforating veins carry blood from the superficial to the deep venous system and are short, straight vessels that can become dilated and tortuous when the valves are congenitally either absent or become damaged, and others connect the gastrocnemius and soleal veins with the superficial veins.
The Deep Venous System
The deep veins begin in the foot, where the plantar and dorsal digital veins communicate via a network of interlacing branches with the plantar cutaneous venous
- ▪
When scanning calf veins, have the patient sit with leg dangling over the side of the stretcher to increase venous “pooling” so that the veins are more distended.
- ▪
Use a curved array transducer for the distal superficial femoral vein; this provides more weight for compression and at the same time achieves acoustic penetration into the adductor hiatus.
- ▪
When scanning a particularly muscular thigh or one of substantial girth, if possible, use manual pressure from the opposite side of the thigh to achieve good coaptation of the walls of the distal superficial femoral vein.
- ▪
When scanning the popliteal vein, position the patient so that the leg is abducted and on a pillow while in either the prone/oblique or supine position, and scan from the medial aspect of the leg. Abducting the knee helps avoid compression of the vein by the tibial tuberosity.
- ▪
If the patient cannot bend his or her knee at all (e.g., after hip or knee replacement), scan the leg from its lateral aspect (vein is on the lateral side of the popliteal fossa).
- ▪
Lack of familiarity with variants of venous anatomy leads to misunderstanding and potentially to failure of recognition of lesions within variant vessels. The following are common variant lesions, but there are many others:
- ▪
Bifid/trifid popliteal veins
- ▪
High tibial bifurcation
- ▪
Bifid superficial femoral vein
- ▪
The vein of Giacomini extending from the short/lesser saphenous vein to greater saphenous vein
- ▪
- ▪
Precision with anatomic descriptions is not as straightforward as is often taken for granted. For example, the levels of the common femoral artery and vein are different; the venous femoral bifurcation is 1 to 2 cm distal to the arterial femoral bifurcation. Hence, an arteriovenous fistula may run from the superficial femoral artery to the common femoral vein.
- ▪
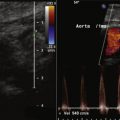
In its proximal segment, flow patterns in the inferior vena cava (IVC) are affected by:
- ▪
Respiratory effort and mode
- ▪
Regurgitation from the right atrium during atrial systole and from tricuspid valve insufficiency
- ▪
The gastrocnemius veins, each with its accompanying artery, are the most superficial in the calf and form a small plexus in the gastrocnemius muscle of the calf, which drains into the popliteal vein at about the same level as the short saphenous vein. They, together with the soleal veins that travel within the deep fascia, are sometimes called sural veins and are considered to be part of the deep venous system. The soleal veins drain blood from the flat soleal muscle, which lies anterior to the gastrocnemius muscle, and in turn drain into the paired peroneal and posterior tibial veins.
At the level of the popliteal fossa, three components of the venous system—the subcutaneous, intermuscular, and intramuscular veins—run in three superimposed planes.
The mostly paired and occasionally triplicate deep veins of the calf consist of the posterior tibial, anterior tibial, and peroneal veins, and they accompany a single artery in each case. The peroneal and posterior tibial veins join to become the tibioperoneal trunk.
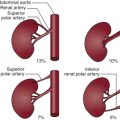
The popliteal vein is formed by the confluence of anterior tibial and tibioperoneal trunks and begins at various levels—below, above, or at the level of the knee joint. It is duplicated in approximately 5% of limbs and becomes the superficial femoral vein at approximately the level of the adductor hiatus, then running in parallel with its accompanying artery to the saphenofemoral junction.
The superficial femoral vein is duplicated in as many as 33% of patients. It may have a complicated course in 1% to 2% of cases, such as being triplicated in a segment (usually in the distal third).
The deep femoral or profunda femoris vein receives flow from numerous branches along its course and invariably communicates distally with the popliteal vein and proximally with the inferior gluteal vein, an arrangement that supplies collateral flow when the superficial femoral vein is thrombosed. It joins the common femoral vein approximately 4 cm below the inguinal ligament.
The lateral and medial circumflex veins, draining blood from the muscles of the hip, thigh, knee, and iliopsoas, also drain into the deep femoral vein.
The common femoral vein becomes the external iliac vein as it passes under the inguinal ligament and in turn becomes the common iliac vein at the level of the pelvic brim, anterior to the sacroiliac joint, where it is joined by the internal iliac vein.
The pubic, inferior epigastric, and deep iliac circumflex veins all drain into the external iliac vein.
Pelvic wall, viscera, reproductive organ, and buttock venous drainage almost completely parallels the arterial supply and with a few exceptions is performed entirely by branches of the internal iliac vein, which in turn drains into the common iliac vein. Exceptions to this include various segments of the bowel, which are drained by the portal vein via branches of the inferior mesenteric, and the ovaries, which drain into the renal vein or in some cases, the IVC via the ovarian veins.
On the left side, the common iliac vein runs medial to the artery but then as it courses proximally, its position rotates and stays behind the artery. It is at this point that the vein is sometimes compressed by the artery against the fifth vertebra in May-Thurner syndrome. Interestingly, this compressive syndrome has been found to exist in healthy asymptomatic individuals. The right common iliac vein runs straight up proximally and medially to a position on the right side and anterior to the fifth lumbar vertebra, where it is joined by the left common iliac vein. An iliolumbar vein drains into each common iliac vein.
The IVC, the largest vein in the body, begins at the confluence of the right and left common iliac veins on the right side of the aorta at the level of the fifth lumbar vertebra and continues proximally. There it enters the porta hepatis, a large groove, in the posterior aspect of the right lobe of the liver, then pierces through the diaphragm and enters the right atrium of the heart. Uncommon variants of the IVC include a left-sided IVC in 0.2% to 0.5% of cases, where the IVC runs to the left of the aorta, terminates in the left renal vein, and crosses over the aorta into the right renal vein, and then follows its usual course. Another uncommon variant is the double IVC, which is present in 0.2% to 0.3% of people, where typically there is a right-sided IVC running from the right common iliac vein and a left-sided IVC extending from the left common iliac vein and terminating in the left renal vein.
Azygos continuation of the IVC is present in 0.6% of people, where the inferior vena cava becomes the azygos vein proximal to the diaphragm and then joins the superior vena cava draining all lower extremity blood. In the case of azygous continuation, the hepatic vein often drains directly into the right atrium.
The inferior vena cava receives six pairs of veins:
- □
Four lumbar veins, which drain the abdominal wall, skin, and muscles of the vertebral column and the spinal cord. An ascending lumbar vein connects the lumbar veins and the common iliac vein with the azygos vein on each side.
- □
Two spermatic or ovarian veins from the testes and ovaries, both containing valves. As with the uterine veins, the ovarian veins become considerably enlarged during pregnancy.
- □
Four to six hepatic veins begin in the parenchyma of the liver where they are divided into upper and lower groups. The upper group consists of three large veins that join the IVC when it is in the porta hepatis groove of the liver. The lower group consists of smaller veins and comes from the right and caudate lobes of the liver.
- □
Two renal veins (per kidney) (normally). The left renal vein receives the left testicular or ovarian vein. Renal venous anomalies include:
- •
Circumaortic left renal veins (8.7%), where there are two left renal veins, the superior running across the aorta anteriorly and the inferior branch running posteriorly
- •
Retroaortic left renal vein (2.7%), where the left renal vein runs behind the aorta
- •
Renal and IVC anomalies, which may coexist
- •
- □
Left and right inferior phrenic veins, which drain the diaphragm. These are thought to be a major source of collateral flow in the presence of portal hypertension.
- □
The right suprarenal vein draining the adrenal glands, which enters the IVC, and the left, which enters into either the left renal or inferior phrenic vein
The venous supply of the organs of the digestive tract drains first into the liver via the portal vein and then into the IVC via the hepatic veins. The portal veins form behind the neck of the pancreas at the level of the second lumbar vertebra, are approximately 8 cm long, and are created by the union of the splenic vein, which drains the lower duodenum and splenic flexure of the bowel, and of the superior mesenteric vein, which drains parts of the small and large intestine. The right gastric vein, which receives flow from the lesser curvature of the stomach, and the left gastric vein, which drains the lower end of the esophagus, flow into the portal vein.
The cystic vein drains blood from the gallbladder into the portal vein, and the paraumbilical vein also drains into the portal vein. The most typical pattern of the portal vein is division into right and left branches at the porta hepatis, which in turn subdivide further in the lobes of the liver. Variants are said to occur in 20% of people; the most common variant is trifurcation of the main portal vein, but there are numerous other branching variants and those associated with malposition of the gallbladder.
The three most common reasons to perform a venous duplex examination of the lower extremity are for the assessment of suspected venous thrombotic disease, for the mapping of venous conduits for arterial bypass surgery, and for the evaluation of venous incompetence.
Venous Thromboembolism
Approximately 0.1% of the population annually develop recognized venous thromboembolism; more develop it and die from it than are recognized. The mortality from thromboembolism is approximately 10%. Only half of fatal thromboembolic episodes are recognized and likely, far fewer nonfatal episodes. The diagnosis of deep vein thrombosis (DVT) and pulmonary embolism (PE) has shifted from invasive venography and pulmonary angiography to serum testing for D-dimer, nuclear ventilation-perfusion testing, duplex DVT scanning, and computed tomography (CT) pulmonary angiography and proximal venography. Although there are potentially benefits to the current diagnostic approach, the reality is that noninvasive testing, if not assiduously performed, is unlikely to be as accurate as what it replaced. Furthermore, inconsistencies and assumptions plague the noninvasive evaluation of venous thrombotic disease.
Although most (90%) venous thrombosis occurs within the deep lower extremity veins, venous thrombosis may be present at any level of veins in the lower and upper extremities, as well as in the visceral veins, the head and neck veins, and the superior and inferior vena cava. Again, although most pulmonary thromboembolism originates from the deep lower extremity veins, not all does.
Use of Duplex Ultrasound for the Evaluation of Suspected Venous Thrombosis
Comprehensive scanning of the lower extremity veins—from the iliac veins down to the feet (including calf veins)—is the preferred duplex method to assess for suspected lower extremity DVT. Such a scan does take more time, but evaluation of the calf veins is relevant. Abridged duplex scanning protocols (scanning of only the femoral and popliteal veins to rule out DVT) are popular simply because of their brevity and ease. However, calf DVT is relevant because it may be symptomatic, may incite post–phlebitic syndrome, and may progress to proximal DVT and may result in PE. The rate of calf to proximal DVT progression is poorly characterized and is likely influenced by the clinical context but may be as high as approximately 5%. Hence, abridged scanning for suspected DVT should be used with discretion, and often it should be repeated at least once to enable detection of DVT progression.
The role of DVT scanning in the assessment of PE is controversial. Approximately 20% of cases of PE are without detectable DVT by venography because the entire bulk of DVT embolized and left insufficient residual bulk to detect. Approximately 70% of cases of PE are without detectable DVT by duplex scanning. CT pulmonary angiography protocols are often adjuncts to lower extremity CT venography. The actual yield of CT venography compared with duplex scanning is poorly established. It does not yet appear comparable. Although the identification of lower extremity DVT is a standard indication for anticoagulation unless contraindications are present, the duration of the course of anticoagulation is emergently different for DVT versus PE. Therefore, establishing whether PE has occurred in the context of recognition of DVT influences the duration of therapy and is useful information.
Risk Factors for Deep Vein Thrombosis
- □
History of deep or superficial venous thrombosis
- □
Prolonged bed rest or immobilization
- □
Recent surgery
- □
Familial history of DVT
- □
Pregnancy
- □
Congestive heart failure
- □
Cancer or history of cancer
- □
Local trauma
- □
Thrombophilia (protein C deficiency, protein S deficiency, antithrombin III deficiency, factor V Leiden, partial thromboplastin mutation)
Summary: Problems with the Use of Duplex Scanning for the Evaluation of Thromboembolic Disease
- □
DVT: abridged protocols often do not address calf level DVT, which is the original site of proximal DVT.
- □
Superficial venous thrombosis scanning
- •
Superficial and deep venous disease may coexist or exist independently; therefore, exclusion of superficial thrombosis does not exclude DVT.
- •
Rarely, a superficial thrombus may extend into the common femoral vein via the saphenofemoral junction.
- •
- □
PE
- •
Only a minority of patients with PE have duplex findings of DVT.
- •
Identification of DVT establishes an indication for anticoagulation but not necessarily of the same duration as does identification of PE.
- •
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree