Carotid blowout syndrome can be a life-threatening late complication of surgical and radiation therapy for head and neck tumors in the vicinity of the cervical carotid artery. The syndrome spans a spectrum of pathology from impending to acute rupture of the artery. These cases are uncommon, can be dramatic in terms of blood loss, and are often true emergencies. The optimal management of these patients requires quick recognition, and often advanced trauma life-support skills and creative endovascular solutions. Definitive endovascular treatment is the therapy of choice in this condition; open surgical options are very limited. In this article, we present some background information regarding the clinical and pathologic aspects of the syndrome and our experience in endovascular management.
Carotid blowout syndrome can be a life-threatening late complication of surgical and radiation therapy for head and neck tumors in the vicinity of the cervical carotid artery. The syndrome spans a spectrum of pathology from impending to acute rupture of the artery. These cases are uncommon, can be dramatic in terms of blood loss, and are often true emergencies. The optimal management of these patients requires quick recognition, and often advanced trauma life-support skills and creative endovascular solutions. Definitive endovascular treatment is the therapy of choice in this condition; open surgical options are very limited. In this article, we present some background information regarding the clinical and pathologic aspects of the syndrome and our experience in endovascular management.
Head and neck tumor overview
More than 500,000 patients worldwide are diagnosed with squamous cell carcinoma of the head and neck each year. The primary site of the tumor can affect the nasopharynx, oropharynx, larynx, and hypopharynx. Smoking, alcohol abuse, and smokeless tobacco are major risk factors for the development of squamous cell cancer of the head and neck. There are also associations between marijuana use and occupational exposures including nickel refining.
There is increasing evidence to suggest that certain viruses are associated with head and neck tumors. Specifically, human papilloma virus (HPV) has an association with squamous cell cancer of the head and neck. Epstein Barr Virus (EBV) has a specific association with nasopharyngeal cancer. Most head and neck tumors occur in men older than 50 years of age. Presenting symptoms can include sore throat, dysphagia, and odynophagia. Nasopharyngeal cancer can present with sore throat, sinusitis, hoarseness, nasal obstruction, epistaxis, and serous otitis media. Patients with more advanced disease may present with cranial neuropathies or cervical lymphadenopathy.
The TNM (Tumor, Node, Metastases) staging system is used, as for most cancer types. Overall outcomes are better in patients with low-grade disease, with an 80% cure rate in patients with stage I disease, and 60% cure rate in patients with stage II disease. Advanced disease (stage III and Stage IV) has a less than 30% cure rate. Nasopharyngeal cancer in particular will often present with nodal metastases, and has a high rate of treatment failure. Organ preservation strategies are preferred when possible. Chemotherapy and radiation therapy are common adjuncts to surgery.
Surgical approaches to patients with head and neck tumors include radical neck dissection, modified radical neck dissection, and selective lymph node dissection.
Radical Neck Dissection
Radical neck dissection involves en bloc removal of the lymph node–bearing tissues on one side of the neck, as well as the removal of the spinal accessory nerve, internal jugular vein (IJV), and sternocleidomastoid muscle. Usually radical lymph node dissections are performed when there are multiple cervical lymph node metastases, particularly involving the posterior triangle of the neck, or if tightly related to the spinal accessory nerve. The presence of a large metastatic tumor mass or matted lymph nodes in the upper part of the neck is also an indication for a radical lymph node dissection. At many institutions, fewer than 20% of neck dissections for tumor are radical lymph node dissections.
Modified Radical Neck Dissection
Modified radical neck dissection attempts to preserve the IJV, the sternocleidomastoid muscle, or the spinal accessory nerve, with the goal of reducing morbidity. Resection of the spinal accessory nerve results in shoulder disability and a cosmetic deformity, which can be avoided sometimes by a modified radical neck dissection.
Selective Lymph Node Dissection
Selective lymph node dissection involves removal of only the lymph node groups at the highest risk of containing metastases.
Radical neck dissection for treatment of primary head and neck tumors can be complicated by carotid artery injury, wound breakdown, and tumor recurrence. Carotid artery rupture occurs primarily if there is thrombosis of the vasa vasorum, which can occur with radiation therapy or surgical stripping of the carotid sheath and has been associated with up to 4% of radical neck dissections.
Carotid blowout syndrome
Carotid blowout syndrome is classically defined as rupture of the extracranial carotid artery or its branches. This is usually a result of wound breakdown after surgical and radiation therapy for head and neck cancer or as a result of trauma. This rupture can result in active bleeding into the airway, pseudoaneurysm, or arteriovenous fistula (AVF) formation. Carotid blowout syndrome is associated with high morbidity and mortality, although outcomes have improved with the advent of endovascular treatment modalities.
Radiation therapy, more extensive surgery, wound breakdown, infection, and tumor recurrence are all predisposing factors for the carotid blowout syndrome. Radiation therapy almost certainly weakens the arterial wall, likely by obliterating the vasa vasorum, resulting in an increased risk of carotid blowout syndrome. Although usually seen in patients with major head and neck resections and concurrent radiation therapy, it can also occur in patients who have had radiation therapy only. Patients with radical neck dissections and wound breakdown are at a high risk of carotid artery rupture. Carotid peel, when tumor encasing the carotid artery is surgically removed, also increases chances of a later carotid blowout.
Tumor recurrence is also a predisposing factor for carotid blowout syndrome, especially when the tumor recurrence invades the carotid artery. Wound breakdown from a previous radical neck dissection or flap mobilization can result in an exposed carotid artery. Patients with squamous cell cancer have many factors that contribute to poor wound healing, which can include poor tissue oxygenation, infection, and the long-term presence of mobile foreign bodies (tracheostomy and nasogastric tube placement). Direct exposure to saliva can result in digestion of the vessel wall by salivary enzymes, as occurs in a pharyngocutaneous fistula.
The initial clinical description of carotid blowout syndrome was by Borsany and the first clinical series reported by Ketcham and Hoye. Chaloupka and colleagues defined carotid blowout as a syndrome with the following three primary subtypes.
Exposed Carotid Artery
Postoperative wound breakdown from radical neck dissection or flap mobilization can result in an exposed carotid artery. This can be treated with placement of healthy well-vascularized tissue over the exposed carotid artery, or if it is not possible to cover the exposed carotid artery with healthy well-vascularized tissue, with a test balloon occlusion and possible carotid sacrifice. Recently this definition has been expanded to include cases where there is radiologic evidence of tumor extension and neoplastic invasion of the carotid system as well as a nonhemorrhagic pseudoaneurysm on angiography.
Impending Carotid Rupture
This subtype refers to patients who present with a sentinel hemorrhage, usually from a pseudoaneurysm. The bleeding in these cases is profuse but self-limited, and can be transoral, transcervical, or through a surgical wound or fistula. An impending carotid rupture is usually from a pseudoaneurysm that leaks intermittently. This type of lesion must be treated emergently.
Acute Carotid Blowout
This subtype refers to acute uncontrolled hemorrhage, which is not controlled with surgical packing. Standard ICU care for these types of patients includes hemodynamic stabilization and airway protection. Adequate venous access is necessary for administration of fluids and blood products, and to maintain an adequate blood pressure. These patients must be treated emergently. Hypotension is a major risk factor for the development of stroke in these patients.
Carotid blowout syndrome
Carotid blowout syndrome is classically defined as rupture of the extracranial carotid artery or its branches. This is usually a result of wound breakdown after surgical and radiation therapy for head and neck cancer or as a result of trauma. This rupture can result in active bleeding into the airway, pseudoaneurysm, or arteriovenous fistula (AVF) formation. Carotid blowout syndrome is associated with high morbidity and mortality, although outcomes have improved with the advent of endovascular treatment modalities.
Radiation therapy, more extensive surgery, wound breakdown, infection, and tumor recurrence are all predisposing factors for the carotid blowout syndrome. Radiation therapy almost certainly weakens the arterial wall, likely by obliterating the vasa vasorum, resulting in an increased risk of carotid blowout syndrome. Although usually seen in patients with major head and neck resections and concurrent radiation therapy, it can also occur in patients who have had radiation therapy only. Patients with radical neck dissections and wound breakdown are at a high risk of carotid artery rupture. Carotid peel, when tumor encasing the carotid artery is surgically removed, also increases chances of a later carotid blowout.
Tumor recurrence is also a predisposing factor for carotid blowout syndrome, especially when the tumor recurrence invades the carotid artery. Wound breakdown from a previous radical neck dissection or flap mobilization can result in an exposed carotid artery. Patients with squamous cell cancer have many factors that contribute to poor wound healing, which can include poor tissue oxygenation, infection, and the long-term presence of mobile foreign bodies (tracheostomy and nasogastric tube placement). Direct exposure to saliva can result in digestion of the vessel wall by salivary enzymes, as occurs in a pharyngocutaneous fistula.
The initial clinical description of carotid blowout syndrome was by Borsany and the first clinical series reported by Ketcham and Hoye. Chaloupka and colleagues defined carotid blowout as a syndrome with the following three primary subtypes.
Exposed Carotid Artery
Postoperative wound breakdown from radical neck dissection or flap mobilization can result in an exposed carotid artery. This can be treated with placement of healthy well-vascularized tissue over the exposed carotid artery, or if it is not possible to cover the exposed carotid artery with healthy well-vascularized tissue, with a test balloon occlusion and possible carotid sacrifice. Recently this definition has been expanded to include cases where there is radiologic evidence of tumor extension and neoplastic invasion of the carotid system as well as a nonhemorrhagic pseudoaneurysm on angiography.
Impending Carotid Rupture
This subtype refers to patients who present with a sentinel hemorrhage, usually from a pseudoaneurysm. The bleeding in these cases is profuse but self-limited, and can be transoral, transcervical, or through a surgical wound or fistula. An impending carotid rupture is usually from a pseudoaneurysm that leaks intermittently. This type of lesion must be treated emergently.
Acute Carotid Blowout
This subtype refers to acute uncontrolled hemorrhage, which is not controlled with surgical packing. Standard ICU care for these types of patients includes hemodynamic stabilization and airway protection. Adequate venous access is necessary for administration of fluids and blood products, and to maintain an adequate blood pressure. These patients must be treated emergently. Hypotension is a major risk factor for the development of stroke in these patients.
Diagnostic imaging
The affected artery in carotid blowout syndrome can include the common carotid artery, the internal carotid artery, and the external carotid artery or its branches. Vascular imaging tests, in particular CT angiography, are valuable in planning appropriate treatment for these lesions by accurately determining the location of the lesion and guiding therapy. This is true even in the setting of active hemorrhage.
CT Angiography
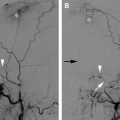
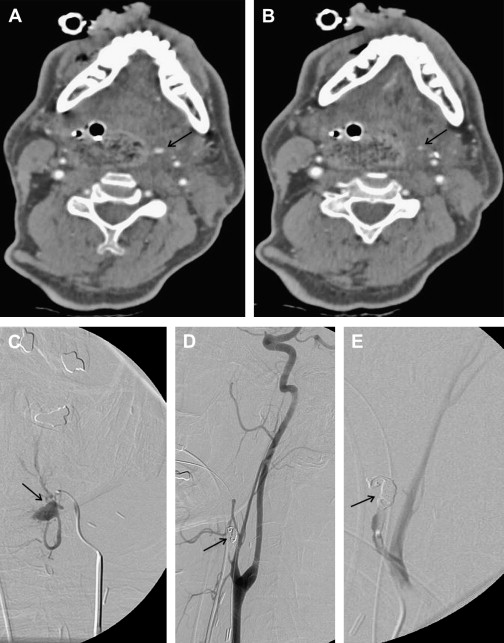
Computed tomography angiography (CTA) can be a very effective screening examination to evaluate for the site of active extravasation and to identify the underlying vascular lesion, such as a pseudoaneurysm. There is value to this information even in the setting of acute hemorrhage, as the localization of a bleeding source can help target the endovascular procedure and save critical time ( Fig. 1 ). In addition, the images also provide very complementary information to the catheter angiogram regarding the soft tissue (if any!) surrounding the artery ( Fig. 2 ). This can be useful in determining whether to sacrifice the vessel or pursue another vessel-preserving strategy such as a stent. The advantages of CT angiography include its speed, allowing the rapid acquisition of data in an unstable patient, and ready availability in the emergency department and inpatient setting. With high-resolution modern multidetector scanners and advanced postprocessing techniques such as multiplanar reconstruction, an effective roadmap for further angiographic evaluation and endovascular treatment can be obtained. Disadvantages of using CT angiography as a screening tool include extra contrast administration and additional radiation exposure, which are usually not prominent concerns in this patient population.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree